Managing insulin resistance requires consistent lifestyle changes like improving diet, exercising regularly, and reducing stress. But staying on track can be tough. Here’s the key takeaway: accountability can significantly improve your chances of success. Whether it’s through a partner, technology, or professional support, having a system in place keeps you consistent and motivated.
Key Points:
- Insulin resistance affects millions and can lead to type 2 diabetes, heart disease, and PCOS if unmanaged.
- Lifestyle changes - like losing 5–10% of body weight - can improve insulin sensitivity by 58%, but staying consistent is challenging.
- Accountability tools, such as telehealth services, glucose monitors, and support systems, make it easier to stick to healthy habits.
Actionable Steps:
- Use an accountability partner or telehealth service for regular check-ins.
- Track progress with tools like glucose monitors and fitness apps.
- Set SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals to create manageable habits.
- Consider professional guidance and explore options like topical or oral metformin for added support.
If you’re struggling to manage insulin resistance, starting small and seeking support can help you build lasting habits.
How to Prevent or Reverse Insulin Resistance
Common Barriers to Sticking with Lifestyle Changes
Before diving into accountability strategies, it’s important to grasp the psychological and practical challenges that often make sticking to lifestyle changes so difficult.
Psychological and Emotional Obstacles
Stress can wreak havoc on insulin resistance. When stress levels rise, cortisol surges, which not only worsens insulin sensitivity but also triggers cravings for sugary and fatty foods. This creates a vicious cycle of stress, emotional eating, and further health challenges.
Past failures can also chip away at confidence. This often leads to an all-or-nothing mindset - one missed workout or indulgent meal can spiral into abandoning efforts altogether. On top of that, depression and anxiety can sap the energy and motivation needed for consistent self-care, making it even harder to stay on track.
"I used to struggle a lot with the side effects for oral metformin and this is a great alternative for me. I get the same benefits but no more upset stomach and nausea, and this helps me stick with it a lot more consistently." - Carrie S. [1]
Practical Challenges to Healthy Living
Time is one of the biggest hurdles. With work, family, and other responsibilities, finding room for the recommended 150 minutes of exercise, meal planning, or cooking can feel impossible. As a result, fast food or prepackaged meals often become the default.
Other obstacles include high costs, limited access to safe spaces for exercise, and the overwhelming amount of conflicting nutrition advice out there. To make matters worse, more than 96 million adults in the U.S. have prediabetes, yet over 80% are unaware of it. Without symptoms, many don’t feel the urgency to change their habits.
Understanding these barriers underscores the importance of accountability strategies, which will be explored next.
Accountability Strategies That Work
Once you've identified the challenges, it's time to put accountability strategies into action. Combining social support, technology, and self-monitoring can make a big difference. Let’s dive into how partners, support systems, and tools can help you stay on track.
Using Partners and Support Systems
Having someone to rely on can make all the difference. An accountability partner - whether it’s a spouse, friend, coworker, or family member - can help you stick to your goals by sharing the experience. You might plan weekly grocery trips together, commit to short daily walks after dinner, or send each other updates to confirm you’re meeting goals like staying within your carbohydrate budget.
To keep the relationship productive, it’s important to set clear boundaries. Decide on a communication style upfront, such as “encourage me, but avoid criticism” or “ask before offering advice”. When setbacks occur, focus on problem-solving by asking questions like, “What got in the way today?” This approach is far more effective than blame and helps avoid the all-or-nothing mindset that can derail progress.
Professional support can also be incredibly helpful. Specialists like registered dietitians, endocrinologists, and telehealth services such as Oana Health provide structured guidance, personalized goals, and regular monitoring of key metrics like weight, fasting glucose, and A1C. These tools not only enhance accountability but also improve outcomes for insulin resistance. Virtual check-ins are especially convenient for women managing insulin-resistance-related conditions like PCOS, unwanted hair growth, or weight challenges. When you combine personal support with technology to track progress, you create a comprehensive system for success.
"Oana's telehealth service is fantastic! It's helped manage my insulin levels and reduce excess hair growth I was experiencing due to PCOS. I'm recommending this to all my friends with PCOS." - Victoria A. [1]
Technology for Tracking Progress
Real-time data turns vague goals into actionable insights. Tools like continuous glucose monitors (CGMs) provide immediate feedback by showing how meals, stress, and exercise impact your blood sugar and insulin levels. Nutrition apps can help you track macronutrients and sugars, which are crucial for improving insulin sensitivity. Fitness trackers, on the other hand, monitor steps, activity levels, heart rate, and sleep - all factors that contribute to better insulin function.
The key is turning this data into practical steps. Dedicate 10 to 15 minutes each week to review your progress. For example, if your CGM shows that sweetened cereal causes a glucose spike every morning, try switching to eggs with vegetables and whole-grain toast, then compare the results. If your step tracker shows you’re averaging only 3,000 to 4,000 steps a day, add two 10-minute walks - one after lunch and one after dinner - to gradually increase your daily total to 7,000 or 8,000 steps, which supports better insulin sensitivity. Many telehealth programs, including Oana Health, can integrate this data to refine treatment plans and adjust medications over time.
Self-Monitoring with Journals and Logs
Keeping a journal helps you slow down and spot patterns. Studies show that self-monitoring improves adherence to diet and exercise plans, helps identify problem behaviors early, and enhances glycemic control in those with metabolic conditions. A simple daily log takes just five minutes to fill out. Include details like wake and sleep times, stress levels (rated 1 to 10), whether you took your medications, brief meal descriptions, exercise type and duration, and two reflection questions: “Did I meet today’s goals?” and “What’s one small win from today?”.
Reviewing your entries weekly can reveal trends, such as frequent high-carb takeout on busy workdays or less activity on weekends. Use these insights to make small, actionable changes - like meal-prepping on Sundays or scheduling a Saturday morning walk. If your clinician recommends tracking fasting blood sugar or reviewing CGM data, include those metrics in your log. Sharing your journal with a partner, group, or telehealth provider adds another layer of accountability and allows for expert feedback and guidance.
sbb-itb-6dba428
Working with Healthcare Professionals and Telehealth Services
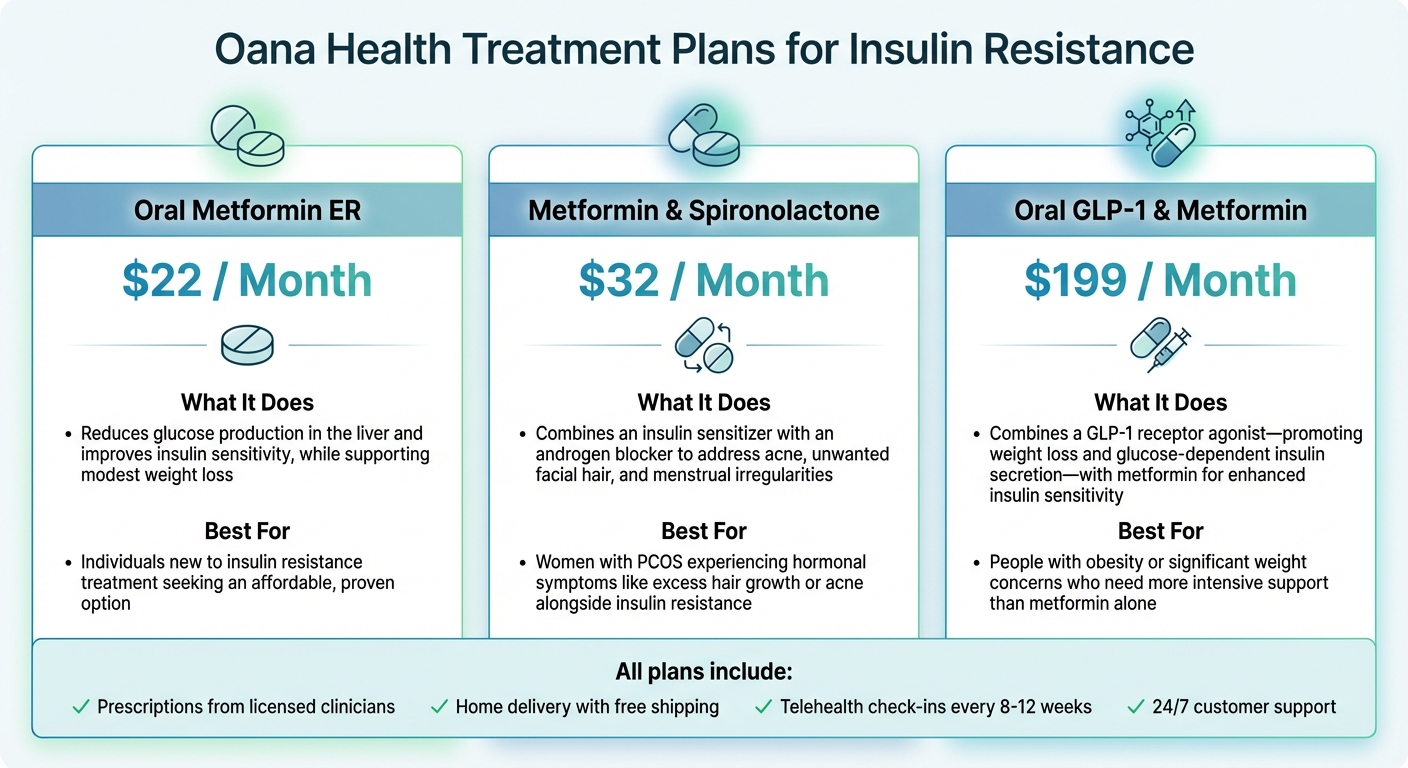
Oana Health Insulin Resistance Treatment Plans Comparison
Licensed clinicians play a critical role in turning health goals into tangible outcomes. Through personalized treatment plans, they combine self-monitoring tools with professional guidance. Healthcare experts - such as primary care doctors, endocrinologists, and registered dietitians - craft these plans based on your lab results, medical history, and lifestyle. When lifestyle adjustments alone aren’t enough, they can prescribe medications like metformin or GLP-1 receptor agonists. They also keep track of key health markers like fasting glucose, A1C, and lipid panels, making adjustments to your plan as needed. Research from the Diabetes Prevention Program showed that lifestyle modifications reduced the progression from prediabetes to type 2 diabetes by 58%, while adding metformin under medical supervision led to a 31% reduction compared to placebo.
Next, let’s explore how telehealth services make accessing this level of care more convenient.
How Telehealth Helps with Insulin Resistance Management
Telehealth breaks down barriers to consistent care. Virtual visits save time by eliminating the need for travel and reducing disruptions to your day, like missed work. You can book appointments outside of standard office hours, review lab results securely online, and message your care team anytime with questions about side effects or progress. For topics like weight management, body image, or symptoms of PCOS, many people find it easier to have honest conversations via video or messaging rather than in a traditional exam room, leading to better engagement and outcomes.
Platforms like Oana Health make managing your care even simpler. They combine a quick 5-minute online medical intake, personalized prescriptions from licensed professionals, and medications shipped directly to your door with free shipping. Features like automatic refills ensure you never run out of treatments, and 24/7 customer support is available whenever you need help. For those who experience nausea or an upset stomach with oral metformin - a common issue - Oana Health offers topical metformin starting at $89 per month. This option provides the same insulin-sensitizing benefits without the gastrointestinal discomfort[1]. These user-friendly services seamlessly integrate into customized treatment plans designed to meet a variety of needs.
Oana Health Treatment Plans for Insulin Resistance
Oana Health builds on the telehealth model by offering treatment plans tailored to individual needs, ensuring consistent medical oversight and accountability. Each plan includes prescriptions from licensed clinicians, home delivery with free shipping, and ongoing support to remove common obstacles to treatment.
| Treatment Option | Monthly Price | What It Does | Best For |
|---|---|---|---|
| Oral Metformin ER | $22 | Reduces glucose production in the liver and improves insulin sensitivity, while supporting modest weight loss. | Individuals new to insulin resistance treatment seeking an affordable, proven option. |
| Metformin & Spironolactone | $32 | Combines an insulin sensitizer with an androgen blocker to address acne, unwanted facial hair, and menstrual irregularities. | Women with PCOS experiencing hormonal symptoms like excess hair growth or acne alongside insulin resistance. |
| Oral GLP-1 & Metformin | $199 | Combines a GLP-1 receptor agonist - promoting weight loss and glucose-dependent insulin secretion - with metformin for enhanced insulin sensitivity. | People with obesity or significant weight concerns who need more intensive support than metformin alone. |
Telehealth check-ins, typically every 8 to 12 weeks, allow clinicians to assess weight trends, lab results, and any side effects, ensuring your plan evolves with your needs. This ongoing cycle of feedback and adjustments transforms a prescription into a sustainable path toward progress.
Building Habits That Last
Daily habits are the cornerstone of lasting change, especially when managing insulin resistance. While structured treatment plans and external support are essential starting points, it's the personal routines you develop that truly make the difference. These habits transform short-term strategies into long-term success.
Professional guidance and prescriptions provide a solid foundation, but the real work happens in the day-to-day. And here's the thing: lasting habits aren’t built overnight. Gradual steps are far more effective than trying to overhaul everything at once.
Setting SMART Goals
SMART goals help turn vague intentions into actionable steps. For instance, instead of saying, "I want to eat healthier", you could set a goal like: "Include at least 1 cup of non-starchy vegetables at lunch and dinner 5 days a week for the next 4 weeks." This goal is:
- Specific: You're adding vegetables to two meals.
- Measurable: It’s easy to track - 1 cup, 5 days a week.
- Achievable: Adding vegetables is a manageable step.
- Relevant: Non-starchy vegetables are high in fiber, which supports insulin sensitivity.
- Time-bound: You’ll review progress after 4 weeks.
For physical activity, you might try: "Walk briskly for 20 minutes after work on Monday, Wednesday, and Friday for the next 3 weeks." Or for weight management: "Lose 4–6 pounds in 8 weeks by cutting sugary drinks and portioning meals." Research shows that even modest weight loss can significantly improve insulin resistance.
Allison L., a patient with Oana Health, shared her experience with setting realistic expectations:
"It's been a little over 5 weeks, and I've noticed a dramatic reduction in my facial hair growth... You really have to stick with it and be patient to notice results!" [1]
This highlights the importance of giving yourself time. For example, medications like metformin may take 3–4 weeks to show noticeable effects. Setting realistic timelines can help avoid frustration and keep you on track.
Once your goals are clear, regular progress reviews are key to maintaining and refining your habits.
Regular Progress Check-Ins
Consistent check-ins help you stay accountable and adjust as needed. During the first 2–3 months, weekly self-reviews can be incredibly effective. For example, track how many days you meet your movement, nutrition, and sleep goals, or monitor your average daily steps.
In addition to self-assessments, schedule monthly or bimonthly check-ins with your healthcare provider or telehealth clinician. These sessions are an opportunity to review weight trends, lab results like fasting glucose and A1C, and address any challenges you’re facing. Carrie S., another Oana Health patient, shared her experience with adjustments:
"I used to struggle a lot with the side effects for oral metformin and this [topical version] is a great alternative for me. I get the same benefits but no more upset stomach and nausea, and this helps me stick with it a lot more consistently." [1]
Celebrate small wins along the way, like better energy, improved sleep, or increased endurance. These milestones can keep you motivated between formal check-ins and remind you that progress is happening, even if it feels slow at times.
Conclusion
Managing insulin resistance calls for steady, achievable steps paired with solid accountability systems. By focusing on balanced eating, regular exercise, modest weight loss, and quality sleep, you can improve insulin sensitivity and reduce the risks of diabetes and heart disease. With these benefits in mind, creating a reliable structure for accountability becomes a cornerstone of success.
Accountability turns good intentions into lasting habits. Knowing you'll check in with someone makes it easier to stick to meal plans, stay active, and follow prescribed treatments. It’s a simple yet powerful way to stay on track.
Start small: choose an accountability partner and set one SMART goal to work on over the next two weeks. This approach helps lay the groundwork for meaningful, long-term changes.
If managing insulin resistance feels overwhelming, consider reaching out for professional help. Services like Oana Health offer personalized, science-based treatment plans designed to support your journey. Their licensed medical professionals can provide options like topical metformin, starting at $89 per month, delivered straight to your door with free shipping. Combining accountability with expert support creates a sustainable path to better health.
FAQs
How does accountability help with managing insulin resistance?
Accountability is a crucial part of managing insulin resistance. It helps you stick to your treatment plan and stay committed to the lifestyle changes needed for improvement. Regular check-ins - whether with a healthcare provider, support group, or a trusted friend - can keep you motivated and on the right path.
Another key aspect is tracking your progress and setting goals that are both realistic and achievable. These practices encourage healthy habits, boost insulin sensitivity, and contribute to lasting health benefits. Even small, consistent steps can lead to meaningful changes in your overall well-being.
What are some practical ways to stay accountable while managing insulin resistance?
Managing insulin resistance effectively becomes much more manageable with the right approach. Begin by setting realistic, personalized goals that align with your health needs and monitor your progress consistently. Tools like telehealth consultations and sticking to your prescribed treatment plan can play a key role in maintaining accountability.
Support from qualified healthcare professionals can also provide a steady foundation. Services offering evidence-based, tailored care for insulin resistance and related health concerns can give you the guidance and structure needed to stay on track and achieve your goals.
How can telehealth help manage insulin resistance?
Telehealth brings a new level of convenience to managing insulin resistance by allowing you to connect with licensed medical professionals without leaving your home. Through virtual consultations, you can receive customized treatment plans designed specifically for your needs, including options like prescription insulin sensitizers.
On top of that, telehealth services make it easier to access your medications by arranging for them to be delivered straight to your door. This hassle-free approach helps you maintain your health goals while cutting down on time and effort.
.webp)



