Breaking the Weight Cycling-Insulin Resistance Loop
If you’re struggling with PCOS, the cycle of weight loss, regain, and worsening symptoms may feel endless. This frustrating loop often stems from insulin resistance, a condition affecting many women with PCOS, regardless of weight. Insulin resistance increases abdominal fat, disrupts hormones, and worsens PCOS symptoms. Restrictive diets often fail because they slow metabolism, increase hunger, and lead to weight regain, especially visceral fat. This not only worsens insulin resistance but also raises the risk of type 2 diabetes.
The solution? Focus on improving insulin sensitivity through balanced nutrition, regular exercise, targeted medications like metformin or GLP-1 receptor agonists, and sustainable lifestyle changes. Key strategies include:
- Eating moderate-carb, high-fiber, low-glycemic meals (e.g., Mediterranean-style foods).
- Incorporating 150–300 minutes of aerobic activity weekly and resistance training.
- Avoiding extreme diets and prioritizing gradual, long-term changes.
- Managing stress, improving sleep, and seeking medical support when needed.
Platforms like Oana Health offer telehealth options to help women with PCOS access personalized care plans, medications, and ongoing support. Breaking the cycle is possible with the right approach and consistent effort.
The Connection Between PCOS, Insulin Resistance, and Weight Cycling
Insulin Resistance's Role in PCOS
Insulin resistance happens when the body's cells don't respond effectively to insulin, prompting the pancreas to produce more of it to keep blood sugar levels in check. This excess insulin, known as hyperinsulinemia, doesn’t just impact blood sugar - it also triggers the ovaries and adrenal glands to produce more androgens while reducing sex hormone–binding globulin (SHBG). Lower SHBG levels mean more free testosterone in the bloodstream, which can lead to symptoms like acne, unwanted hair growth, scalp hair thinning, and irregular menstrual cycles.
Studies suggest that around 35–80% of women with PCOS experience insulin resistance and compensatory hyperinsulinemia. Interestingly, this can occur even in women with a normal body mass index (BMI). Elevated insulin levels contribute to the buildup of visceral fat, which exacerbates hormonal imbalances [2, 12, 13]. These imbalances set the stage for negative metabolic changes, especially during periods of weight cycling.
How Weight Cycling Affects Metabolism and Hormones
Weight cycling, or the repeated loss and regain of weight, often amplifies the metabolic disruptions caused by insulin resistance. When weight is regained, it tends to come back as fat, particularly around the abdomen [2, 12, 13]. This increase in visceral fat heightens inflammation and worsens insulin resistance, which can lead to even higher levels of insulin and androgens [2, 12].
These changes also slow down the metabolic rate and disrupt hunger-regulating hormones. For example, ghrelin, the hormone that stimulates appetite, increases, while leptin, which signals fullness, decreases [2, 3, 11]. This imbalance can lead to cravings for refined carbohydrates. In women with PCOS, these metabolic shifts worsen hormonal imbalances, causing more dramatic blood sugar spikes and crashes after meals. These fluctuations often result in energy dips, intense cravings, and overeating. Additionally, weight cycling can interfere with the hormonal signals needed for ovulation, leading to irregular or missed menstrual cycles [2, 10, 12]. Over time, many women find that each dieting attempt becomes less effective, with faster plateaus and worsening symptoms.
To break this cycle, focusing on improving insulin sensitivity is key. This can be achieved through balanced nutrition, regular physical activity, and, when needed, targeted medications. Telehealth platforms like Oana Health offer tailored, evidence-based plans that include lab testing and medication support, helping women manage their metabolism and hormonal health sustainably.
Why Standard Diets Don't Work for Women with PCOS
Metabolic Changes from Restrictive Dieting
For women with PCOS, restrictive diets often create more problems than they solve. These diets, especially low-calorie crash plans, can trigger unique metabolic reactions. Insulin resistance - a condition affecting up to 75% of lean women and 95% of women with obesity who have PCOS - makes the typical "eat less, move more" advice less effective. When calories are severely restricted, the body responds by conserving energy, reducing the resting metabolic rate by 10–25%. This slowdown can linger, meaning fewer calories are burned daily, even after the diet ends.
On top of that, restrictive diets disrupt hunger and fullness hormones. Ghrelin, the hormone that signals hunger, increases, while leptin, which helps you feel full, decreases. For women with PCOS, who already struggle with appetite regulation due to high insulin and androgen levels, this hormonal imbalance worsens the cycle of strict dieting followed by overeating or binge eating. Each binge spikes blood sugar and insulin levels, further aggravating insulin resistance and making future dieting efforts even harder. In fact, an Australian survey revealed that 96.3% of women with PCOS had tried to lose weight, with more than half reporting distressing cycles of weight loss and regain.
Restrictive Dieting and Increased Belly Fat
One of the most concerning effects of restrictive dieting isn't just regaining weight - it’s where that weight is stored. Women with PCOS are more likely to accumulate visceral fat, the type of fat that surrounds internal organs, even when their body mass index is similar to those without PCOS. A 2023 study published in Scientific Reports found that women with PCOS and insulin resistance had significantly higher levels of visceral fat. They also showed elevated triglycerides, blood pressure, and liver enzymes compared to women with PCOS who didn’t have insulin resistance.
Restrictive diets tend to worsen this issue. They encourage the body to store regained weight as visceral fat, which is more metabolically active and promotes inflammation. This, in turn, further damages insulin sensitivity. It’s a vicious cycle: insulin resistance leads to weight gain, which prompts another round of restrictive dieting, only to result in rapid weight regain, particularly around the belly. This cycle not only worsens insulin resistance but also raises the risk of type 2 diabetes, high blood pressure, and cardiovascular disease - conditions already more common in women with PCOS.
Standard diets that promise quick fixes often end up making these metabolic challenges worse. Instead of solving the problem, they amplify it. Recognizing these unique metabolic responses is crucial for developing personalized strategies that address the root causes of PCOS, rather than perpetuating the cycle of frustration and poor health outcomes.
PCOS Insulin Resistance And Weight Gain? (How to STOP it) | PCOS Weight Loss
sbb-itb-6dba428
Strategies to Break the Cycle
Crash diets can harm metabolic health, especially for those with PCOS. Breaking free from the cycle of weight fluctuations and insulin resistance requires a multi-pronged approach that addresses nutrition, exercise, medications, and mindset to tackle the root causes and promote lasting stability.
Nutrition Approaches to Improve Insulin Sensitivity
For women with PCOS, the best eating plan emphasizes moderate carbohydrates (about 40–45% of daily calories), high fiber, low-glycemic index foods, and Mediterranean-style meals. Build your meals around non-starchy vegetables, lean proteins (like chicken, fish, eggs, Greek yogurt, tofu), healthy fats (such as olive oil, nuts, avocado), and smaller portions of high-fiber carbs like beans, quinoa, brown rice, or steel-cut oats.
Low-glycemic carbohydrates, such as berries, apples, sweet potatoes, lentils, and whole grains, help prevent blood sugar spikes and insulin surges, which can lead to cravings. Avoid refined options like white bread, white rice, and sugary drinks. Adopting a Mediterranean-style approach means using extra-virgin olive oil as your primary cooking fat, eating fish at least twice a week, focusing on vegetables and fruits daily, and swapping processed snacks for whole foods. Aim for 25–30 grams of fiber daily to further enhance insulin sensitivity.
For example, a burrito bowl with half the rice, double the beans, extra vegetables, and guacamole is a better choice for blood sugar control than a large flour tortilla burrito. Avoid extreme low-calorie or very low-carb diets, as these can slow your metabolism and lead to weight regain. The next step? Incorporating regular exercise to amplify these benefits.
Exercise for Insulin Sensitivity and Weight Stability
Physical activity directly improves how muscles use insulin by increasing the GLUT4 transporters, which help glucose enter cells more efficiently. Exercise also reduces visceral fat, the belly fat linked to inflammation and worsening insulin resistance.
A good weekly exercise routine includes 150–300 minutes of moderate aerobic activity (like brisk walking, cycling, or swimming) or 75–150 minutes of vigorous activity (such as jogging or cardio classes), spread across at least three days. Add resistance training two to three times weekly, focusing on major muscle groups with exercises like squats, lunges, dumbbell presses, and rows. Aim for 2–3 sets of 8–12 repetitions. Building muscle not only boosts your resting metabolism but also improves glucose uptake over time.
For those cleared by their doctor, high-intensity interval training (HIIT) once or twice a week can significantly enhance insulin sensitivity and reduce visceral fat in as little as 10–20 minutes. A simple HIIT session might include 30 seconds of fast walking or jogging alternated with 60 seconds of easy walking, repeated 8–10 times. Even short post-meal walks of 10–15 minutes can help lower glucose and insulin levels.
If joint pain is a concern, start with low-impact activities like water aerobics, stationary cycling, or using an elliptical machine. When lifestyle changes alone aren't enough, medications can provide additional support.
Medication Support for Insulin and Weight Management
For some women, lifestyle changes may need the added help of medications to break the cycle. Many women with PCOS experience insulin resistance even at a healthy weight, and obesity can worsen both insulin resistance and cardiovascular risks.
Metformin is a common treatment that helps muscles and the liver respond better to insulin, lowers fasting insulin levels, and reduces glucose production by the liver. It can also lower androgen levels and improve ovulation. Metformin is particularly helpful for women with prediabetes, impaired glucose tolerance, or a family history of type 2 diabetes. Options include Oral Metformin ER ($22/month) or a topical lotion, which may reduce gastrointestinal side effects.
"I'm so glad I discovered Oana's metformin lotion! I used to struggle a lot with the side effects of oral metformin, and this is a great alternative for me. I get the same benefits but no more upset stomach and nausea, and this helps me stick with it a lot more consistently." - Carrie S., Topical Metformin user
GLP-1 receptor agonists, such as semaglutide and liraglutide, offer another option. These medications enhance insulin secretion, slow gastric emptying, and reduce appetite, leading to weight loss (often over 10% of body weight) and better blood sugar control. They’re especially useful for women with a BMI of 30 or higher (or 27 with additional health issues) who struggle with weight cycling despite structured lifestyle changes.
Medications should always be prescribed and monitored by a licensed clinician. They’re most effective when combined with a tailored nutrition and exercise plan. Telehealth services like Oana Health make access easier by providing remote evaluations, prescriptions, and follow-ups. Medications are shipped directly to your home, saving time and reducing barriers. Options like the Oral GLP-1 & Metformin plan ($199/month) or the Metformin & Spironolactone pack ($32/month) address both metabolic and hormonal symptoms.
"Thanks to Oana, my menstrual cycles are more regular, and my skin has never looked better! I also love the 24/7 accessibility and customer service that always goes the extra mile." - Margaret K., MetSpiro user
Behavioral Changes for Long-Term Success
Since PCOS is a lifelong condition, shifting your focus from rapid weight loss to improving metabolic health is key. Instead of relying on the scale, celebrate non-scale victories like more regular cycles, better energy, fewer sugar cravings, improved sleep, and healthier lab results (e.g., A1C, fasting insulin, triglycerides, blood pressure).
Ditch the "good versus bad foods" mindset and adopt a flexible structure. This means consistent meal timing, balanced plates with protein, fat, and fiber, and portion awareness - without rigid rules that could lead to binges. Link new habits to existing routines; for instance, take a 10-minute walk after dinner or drink water before your morning coffee. Focus on process goals like "three strength workouts per week" or "add one vegetable to lunch daily" rather than solely on weight loss.
Stress management, quality sleep, and mental health support are equally critical. Chronic stress raises cortisol levels, worsening insulin resistance and promoting visceral fat storage. Poor sleep disrupts hunger hormones and glucose metabolism. Consider Omega-3 supplements (1,000 mg EPA+DHA daily) to help reduce inflammation and support mood, as anxiety and depression are common in women with PCOS [1].
Combining these behavioral strategies with your nutrition, exercise, and medication plan can help create lasting improvements. Regular check-ins with a clinician, dietitian, or coach are essential for tracking progress and preventing burnout, ensuring your efforts lead to sustainable results.
Building a PCOS Management Plan
PCOS Challenges and Evidence-Based Solutions Guide
Tackling insulin resistance and breaking the cycle of weight fluctuations starts with understanding your current health and tailoring a plan to your specific symptoms. By establishing baseline metrics and working through a structured approach, you can track progress, adjust strategies, and avoid the all-or-nothing mindset that often worsens metabolic health.
Baseline Assessments and Lab Screening
Before making any lifestyle changes, it's crucial to establish a solid starting point with the help of a clinician. This involves gathering key metrics such as weight, height, BMI, waist circumference (in inches), and blood pressure. These measurements help identify metabolic targets, as visceral fat is closely linked to insulin resistance and cardiovascular risks. Additionally, keeping track of your menstrual cycles, PCOS symptoms, family history of diabetes or heart disease, and past dieting attempts can help pinpoint potential triggers for weight fluctuations.
Lab tests are another essential component. Important screenings include fasting plasma glucose (normal: <100 mg/dL; prediabetes: 100–125 mg/dL; diabetes: ≥126 mg/dL), A1C levels (normal: <5.7%; prediabetes: 5.7–6.4%; diabetes: ≥6.5%), and fasting insulin (levels above 15–20 µIU/mL may indicate concerns). A lipid panel (measuring total cholesterol, LDL, HDL, and triglycerides) provides additional insights. For many women with PCOS, checking liver enzymes for fatty liver disease and hormone levels - such as total and free testosterone, SHBG, LH, FSH, and TSH - can help assess androgen levels and ovulatory function.
These assessments allow you and your clinician to set achievable goals, like reducing an A1C from 6.1% to below 5.7% or bringing triglycerides into a healthier range. With a clear understanding of your starting point, you can focus on improving insulin sensitivity while avoiding cycles of weight regain.
Coordinating Lifestyle Changes with Medical Support
Once baseline data is in place, the next step is to combine lifestyle adjustments with medical guidance. A strong management plan brings together nutrition, exercise, medications, and behavior changes, all while being monitored and adjusted over time. Platforms like Oana Health offer remote support through evaluations, tailored prescriptions, and follow-ups. For instance, clinicians can prescribe medications like Oral Metformin ER (starting at $22/month) or an Oral GLP-1 & Metformin plan (at $199/month) to address insulin resistance and weight concerns.
Virtual dietitians and health coaches can also play a key role, offering PCOS-specific meal plans and exercise routines that consider challenges like fatigue or joint discomfort. Regular digital check-ins provide support for emotional eating, stress, and motivation, all of which are common hurdles in managing PCOS.
A typical weekly routine might include:
- Three balanced meals with 20–30 grams of protein each
- 30–40 minutes of brisk walking three times a week
- Two resistance training sessions
- 7–9 hours of sleep every night
- Daily stress management practices
- Taking prescribed medications, such as metformin, as directed
This steady, supported approach encourages gradual improvements in metabolic health without the ups and downs of short-term diets.
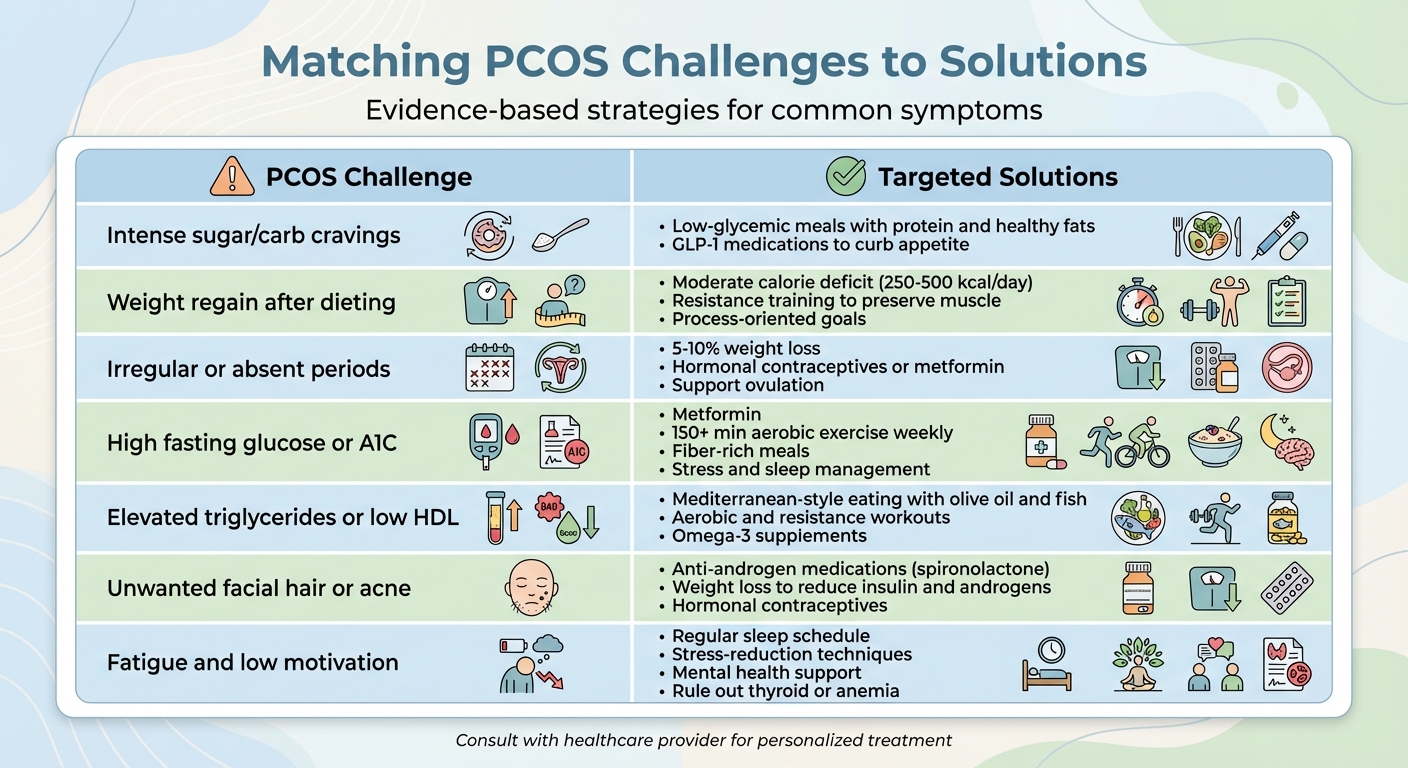
Matching PCOS Challenges to Solutions
A successful management plan addresses your specific PCOS challenges with targeted strategies. The table below links common symptoms to practical solutions, helping you focus your efforts where they matter most:
| PCOS Challenge | Targeted Solutions |
|---|---|
| Intense sugar/carb cravings | Opt for low-glycemic meals that include protein and healthy fats; GLP-1 medications may also help curb appetite. |
| Weight regain after dieting | Maintain a moderate calorie deficit (250–500 kcal/day), include resistance training to preserve muscle, and focus on process-oriented goals rather than outcomes. |
| Irregular or absent periods | Aim for modest weight loss (5–10%) and consider hormonal contraceptives or metformin to regulate cycles and support ovulation. |
| High fasting glucose or A1C | Use insulin-sensitizing medications like metformin, aim for at least 150 minutes of aerobic exercise weekly, eat fiber-rich meals, and manage stress and sleep. |
| Elevated triglycerides or low HDL | Follow a Mediterranean-style eating plan with olive oil and fish, maintain aerobic and resistance workouts, and consider omega-3 supplements. |
| Unwanted facial hair or acne | Anti-androgen medications like spironolactone can help, along with weight loss to reduce insulin and androgen levels; hormonal contraceptives may also be effective. |
| Fatigue and low motivation | Stick to a regular sleep schedule, incorporate stress-reduction techniques, seek mental health support, and rule out thyroid or anemia issues with your clinician. |
Conclusion
For those with PCOS, the frustrating cycle of repeated dieting and weight regain often stems from insulin resistance and hyperinsulinemia. These biological factors - paired with elevated androgens - create a loop that conventional restrictive diets fail to address. Extreme calorie cuts not only slow metabolism but also heighten hunger and lead to the return of belly fat, perpetuating the issue.
But here’s the encouraging part: this cycle can be broken. Small, sustainable changes - like losing 5–10% of body weight, increasing protein and fiber intake, taking daily 20–30 minute walks, and improving sleep habits - can make a real difference. These adjustments can help regulate menstrual cycles, lower androgen levels, and reduce the risk of diabetes. Research shows that many women with PCOS experience better fasting insulin levels, improved ovulation, and reduced androgen levels when they combine these lifestyle strategies with insulin-sensitizing medications prescribed by knowledgeable healthcare providers. The key lies in creating a plan rooted in metabolic science and tailored to the unique challenges of PCOS.
Ready to take action? Start small. Schedule baseline lab tests like fasting glucose, A1C, fasting insulin, and lipid panels. Or try a simple step, such as a 10-minute walk after dinner. For more comprehensive support, Oana Health offers virtual access to clinicians who specialize in PCOS, insulin resistance, and weight management. They provide personalized care plans, including medications prescribed by licensed professionals, delivered directly to your door with free shipping. This makes consistent treatment and follow-up more convenient than ever.
Breaking free from the weight cycling and insulin resistance loop isn’t something you have to tackle alone. With the right mix of lifestyle changes, medical guidance, and ongoing support, you can move toward more stable health, improved energy, and better management of PCOS symptoms - all while keeping it practical for your daily life.
FAQs
How does insulin resistance lead to weight cycling in people with PCOS?
Insulin resistance is a major factor in weight cycling for people with PCOS, as it disrupts the body’s ability to handle glucose properly. This disruption can lead to unstable blood sugar levels, which often trigger increased hunger and intense cravings.
These blood sugar swings make it more difficult to maintain a consistent weight, frequently causing a pattern of losing and regaining weight. Over time, this repeated cycle can worsen insulin resistance and amplify PCOS symptoms, creating a tough cycle to escape.
What dietary changes can help break the cycle of insulin resistance?
Improving insulin sensitivity begins with embracing a balanced, nutrient-rich diet. Prioritize low-glycemic options like whole grains, non-starchy vegetables, berries, nuts, seeds, and fatty fish. Incorporate lean proteins and healthy fats into your meals, while cutting back on processed foods, added sugars, and refined carbs.
Keeping a consistent meal schedule and practicing portion control can also help maintain stable blood sugar levels. For personalized guidance, it’s a good idea to consult a licensed healthcare provider who can design a plan tailored to your specific needs.
Can exercise alone help stop the cycle of weight gain and insulin resistance in PCOS?
Exercise plays an important role in managing PCOS, but it’s rarely enough by itself to disrupt the cycle of weight gain and insulin resistance. This cycle is complex and often requires a mix of approaches, including balanced nutrition, medical treatments, and lifestyle changes.
For many people with PCOS, tackling insulin resistance involves a personalized strategy that combines physical activity with addressing hormonal imbalances. Working with a healthcare provider can help you develop a plan that fits your specific needs.
