Checklist for Evaluating PCOS Weight Loss Therapies
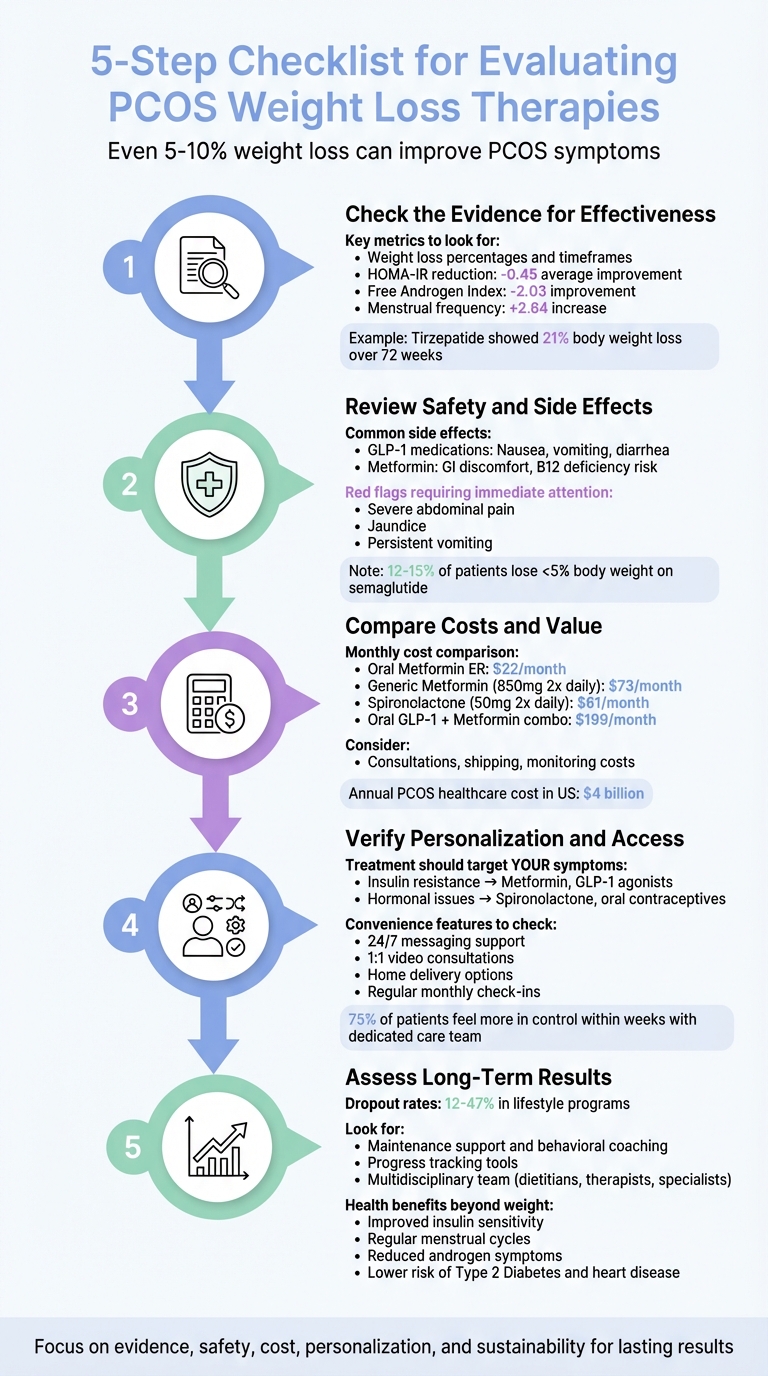
Losing weight with PCOS can be challenging due to insulin resistance, hormonal imbalances, and inflammation. To find the right treatment, focus on five factors: effectiveness, safety, cost, personalization, and long-term results. Even a small weight loss (5%-10%) can improve symptoms like ovulation and insulin sensitivity. Here's a quick guide to evaluating therapies:
- Effectiveness: Look for clinical trial data showing improvements in weight, insulin resistance, and PCOS symptoms.
- Safety: Understand common side effects (e.g., nausea with GLP-1 medications, B12 deficiency with Metformin) and check for contraindications.
- Cost: Compare monthly prices, including medication, consultations, and monitoring.
- Personalization: Choose treatments tailored to your symptoms (e.g., insulin resistance, hormonal acne).
- Long-Term Results: Opt for programs with maintenance support to avoid regaining weight.
Telehealth platforms like Oana Health provide personalized care, convenient delivery, and ongoing support, making PCOS management more accessible. Focus on treatments that address both weight loss and broader health improvements.
5-Step Checklist for Evaluating PCOS Weight Loss Therapies
How To Lose Weight With PCOS And Metformin
1. Check the Evidence for Effectiveness
When evaluating therapies for PCOS, it's essential to focus on treatments with proven results. Seek out clinical trial data that measure outcomes like weight loss, improved insulin sensitivity (HOMA-IR), and normalization of PCOS symptoms such as menstrual regularity and androgen levels. For instance, a meta-analysis of 29 studies involving 1,529 participants revealed that weight loss interventions reduced HOMA-IR by an average of -0.45, improved the Free Androgen Index by -2.03, and increased menstrual frequency by 2.64. These data points reflect meaningful progress in addressing the root causes of PCOS.
Look for Clinical Trial Data
Pay close attention to studies that assess both weight loss and metabolic markers. A therapy that merely reduces weight without addressing insulin resistance or hormonal imbalances won’t fully tackle the challenges of PCOS. For example, clinical trials for tirzepatide (Zepbound) showed participants losing an average of 21% of their body weight over 72 weeks at the highest dose. Evidence like this - complete with percentages, timeframes, and participant numbers - should guide your evaluation of any therapy.
"Weight loss interventions were associated with improvements in some important features of PCOS and should be considered as a routine treatment option for people with PCOS." - Jadine Scragg, MSci, PhD, University of Oxford
Once you’ve reviewed clinical trial data, compare these findings to existing treatment benchmarks.
Review Standard Treatment Options
Understanding how current treatments perform helps establish a baseline for comparison. For example, GLP-1 receptor agonists like liraglutide have outperformed both orlistat and metformin in reducing total weight and waist circumference in PCOS patients. Metformin remains a reliable first-line option, especially for non-obese women (BMI < 30-32) dealing with anovulatory infertility, where it delivers live birth rates comparable to clomiphene. However, clomiphene tends to yield better fertility outcomes in obese patients. When evaluating treatments, prioritize those that address both hormonal imbalances and glucose metabolism.
Keep in mind that some trials may not show substantial improvements in symptoms like hirsutism or quality of life. This is often due to limited sample sizes or short study durations. Setting realistic expectations is key. Strong, well-supported data not only validates a treatment’s effectiveness but also helps guide decisions around cost and tailoring therapies to individual needs.
2. Review Safety and Side Effects
When considering a PCOS weight loss therapy, it's just as important to weigh the potential risks as it is to assess how effective the treatment might be. Understanding the safety profile of a therapy early on allows for better decision-making. For example, GLP-1 medications like semaglutide and tirzepatide often lead to gastrointestinal issues, such as nausea, vomiting, diarrhea, or constipation, particularly as the dosage increases . Similarly, metformin is known to cause gastrointestinal discomfort, including nausea and diarrhea. Starting metformin at a low dose, such as 500 mg twice daily, or taking it with meals can help reduce these symptoms . This information provides a foundation for carefully evaluating the risks associated with each treatment option.
Identify Common Side Effects
It's important to consider both mild and potentially serious side effects. For instance, GLP-1 therapies often cause mild gastrointestinal discomfort, but they also carry more serious risks, such as pancreatitis or medullary thyroid cancer. Metformin, while generally well-tolerated, has a rare but serious risk of lactic acidosis. Long-term use may also lead to a vitamin B12 deficiency . Additionally, GLP-1 medications can interfere with the effectiveness of oral contraceptives, making backup or alternative birth control methods necessary . Another concern with GLP-1 therapies is reduced appetite, which can sometimes result in malnutrition or protein deficiency, potentially causing muscle loss and a slower metabolism.
"Physicians must be vigilant for signs of pancreatitis and monitor kidney function among people taking GLP-1RA medications. Kidney problems can occur without symptoms until the condition is at an advanced stage." – Ziyad Al-Aly, MD, Clinical Epidemiologist
If you experience severe abdominal pain, jaundice (yellowing of the skin or eyes), persistent vomiting, or difficulty with bowel movements, seek medical attention immediately . It's also worth noting that clinical trials have shown that 12% to 15% of individuals taking semaglutide lost less than 5% of their body weight, highlighting that these medications are not effective for everyone. Supportive measures can help manage side effects if they arise.
Check for Contraindications
Some conditions may make certain therapies unsuitable. For instance, GLP-1 medications are not recommended if you or a family member has a history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Caution is also advised for individuals with a history of pancreatitis, kidney issues, or diabetic retinopathy. Metformin, on the other hand, should only be used if kidney and liver functions are normal, as it is contraindicated in cases of severe kidney or liver disease and advanced congestive heart failure. Additionally, GLP-1 medications should be discontinued at least two months before trying to conceive. Anti-androgens like spironolactone require effective contraception due to the risk of birth defects and may also lead to hyperkalemia, especially when combined with oral contraceptives containing drospirenone .
3. Compare Costs and Value
When exploring treatments for PCOS, cost is a major consideration. But it’s important to think beyond the upfront price. Expenses like prescription fees, shipping, consultations, and ongoing monitoring can add up quickly. In the U.S., managing PCOS costs the healthcare system about $4 billion annually, impacting 5% to 10% of women of childbearing age. To get a clear picture, calculate the total cost - everything from medications and shipping to consultations and follow-ups. Then, look at monthly pricing to evaluate how cost-effective each option is.
Compare Monthly Prices
Monthly costs for PCOS weight loss treatments vary depending on the type of therapy and how it’s delivered. For instance:
- Oral Metformin ER starts at $22 per month as a basic insulin sensitizer.
- Oral GLP-1 & Metformin combination therapy costs $199 per month, offering dual-action weight loss support along with telehealth access.
- Generic Metformin (850 mg twice daily) averages $73 per month.
- Spironolactone (50 mg twice daily) comes in at about $61 per month.
Telehealth services can reduce costs by removing traditional pharmacy markups. Platforms like Oana Health even include free shipping on all treatments, eliminating an expense that brick-and-mortar pharmacies often charge. Over time, comparing these monthly prices alongside your treatment needs will help you understand which option offers the best overall value.
Calculate Long-Term Costs
Since PCOS is a chronic condition, treatment costs can build up over the years. Telehealth subscriptions provide predictable monthly pricing, often without extra charges for office visits or lab work. In contrast, traditional care can include co-pays for appointments and tests, such as monitoring for vitamin B12 deficiencies with Metformin or hyperkalemia with Spironolactone.
It’s also worth noting that over 50% of PCOS patients will eventually develop prediabetes or type 2 diabetes. That makes early intervention with cost-effective therapies even more important. While combination therapies priced at $199 per month may seem expensive upfront, they often deliver better weight loss results for the money, especially when you consider the added convenience of telehealth consultations and home delivery, which save both time and travel expenses.
sbb-itb-6dba428
4. Verify Personalization and Access
Polycystic Ovary Syndrome (PCOS) doesn't manifest the same way for everyone. For example, between 38% and 88% of women with PCOS also experience obesity, but symptoms can vary widely. You might face challenges like insulin resistance, irregular menstrual cycles, hormonal acne, or excess hair growth. This is why a one-size-fits-all approach simply doesn’t work. It's essential to ensure that your treatment plan is tailored to your specific symptoms and medical history. This kind of customization builds on the evidence and safety considerations discussed earlier.
Confirm PCOS-Specific Treatment
Your treatment should focus on your most pressing symptoms - whether that's insulin resistance, weight management, or androgen-related issues like acne or excess hair growth. For those dealing with insulin resistance and weight gain, medications such as Metformin or GLP-1 receptor agonists (e.g., semaglutide or tirzepatide) can enhance insulin sensitivity and aid in weight loss . On the other hand, if hormonal imbalances are the primary concern, medications like Spironolactone or oral contraceptives are often recommended to address androgen excess .
Many modern telehealth platforms provide access to specialized care teams, including clinicians trained in obesity and registered dietitians with expertise in PCOS and metabolic health. For example, platforms like Oana Health offer personalized treatment plans created by licensed professionals.
If you're planning for a future pregnancy, it’s critical to discuss this with your provider. Certain treatments, such as some birth control pills or anti-androgens, may not be suitable. Additionally, your provider should check for any contraindications - like assessing kidney and liver function before prescribing Metformin.
Once you've confirmed that your treatment plan is tailored to your needs, it's time to assess how convenient it is to access and maintain.
Check Convenience Features
A customized treatment plan is only effective if it fits seamlessly into your life. Access to care should be practical and aligned with your schedule. Many telehealth platforms now offer features like 1:1 video consultations, 24/7 messaging, and regular monthly check-ins to monitor your progress and adjust medications when necessary . This ongoing support is particularly important given that lifestyle intervention programs for PCOS often see dropout rates between 12% and 47%, emphasizing the need for consistent professional guidance.
Be sure to review what’s included in the service's pricing. Some platforms may charge extra for follow-up visits or medication adjustments, while others bundle these services into one comprehensive package. Features like home delivery can also make a big difference, saving you time and eliminating travel expenses. Many platforms even include free shipping. Notably, over 75% of patients who work with a dedicated PCOS care team report feeling more in control of their health within just a few weeks.
5. Assess Long-Term Results
Losing weight in the short term often isn’t the hardest part - it’s keeping it off that presents the real challenge. Research shows that many people regain the weight they’ve lost within a year. That’s why it’s essential to evaluate whether a therapy provides the tools and support needed for lasting success. Beyond the initial evidence, safety, cost, and customization, the ability to maintain results over time is a key factor to consider.
Look for Maintenance Support
High dropout rates, ranging from 12% to 47%, highlight the importance of ongoing, engaged support. While initial results and affordability are important, programs that emphasize maintenance through behavioral coaching, goal-setting tools, and progress tracking are better equipped to help you sustain long-term success. These features encourage the development of habits that stick.
"Achieving this goal [sustainable weight loss] remains a challenge for both patients and healthcare providers. More research focusing on the multidisciplinary approach... is needed." - Journal of Gynecology Obstetrics and Human Reproduction
The most effective programs don’t just stop at weight loss - they involve a team of experts, such as dietitians, behavioral therapists, and exercise specialists. For example, platforms like Oana Health offer ongoing access to licensed medical professionals who can adapt your treatment plan as your needs evolve. Regular check-ins with these professionals can make a big difference, especially when life throws you curveballs.
Consider Health Benefits Beyond Weight Loss
Even modest weight loss - about 5% to 10% of your body weight - can lead to meaningful health improvements. These include better insulin sensitivity, more regular menstrual cycles, and fewer androgen-related symptoms like acne and excess hair growth. These benefits go beyond the number on the scale, improving overall health in ways that matter day-to-day.
Managing weight effectively can also lower the risk of long-term health issues such as Type 2 Diabetes, heart disease, and endometrial cancer . On top of that, many women report feeling more energetic, mentally sharp, and generally better about their quality of life. When choosing a therapy, it’s worth asking: Does this program track broader health markers like metabolic improvements and menstrual regularity, or does it focus solely on weight? The best approaches take a holistic view, monitoring not just pounds lost but also how you feel and function every day .
Conclusion
Finding the right weight loss therapy for PCOS becomes much simpler when you have a clear framework to guide you. By focusing on five key factors - evidence-based effectiveness, safety, cost, personalization, and long-term sustainability - you can confidently identify an approach that aligns with your individual needs and circumstances.
Even a modest weight loss of 5% to 10% can lead to noticeable improvements in PCOS symptoms. The real challenge lies in choosing a therapy you can maintain over time, as consistency plays a much bigger role than chasing quick fixes. Programs that integrate medical expertise with dietary and behavioral support often deliver the most lasting results.
Telehealth platforms like Oana Health are transforming PCOS care by making it more accessible. These services connect you with licensed medical professionals who specialize in PCOS, offering personalized treatment plans and even convenient home delivery options. By breaking down traditional barriers to care, they ensure that tailored, evidence-backed solutions are within reach.
Ultimately, a multidisciplinary approach offers the most comprehensive care. Effective PCOS management goes beyond weight loss to also address insulin resistance, hormonal imbalances, and overall quality of life. Whether you're just starting your journey or refining your current strategy, this checklist helps you evaluate therapies through the lens of effectiveness, safety, cost, personalization, and sustainability.
FAQs
How can I tell if a PCOS weight loss therapy is working for me?
To assess whether a PCOS weight loss therapy is working for you, begin by keeping track of key measurements related to your symptoms. Monitor your weight, BMI, and waist circumference, aiming for a weight reduction of 5%–10%. Even small changes in weight can lead to noticeable improvements in PCOS-related issues. Be mindful of shifts in areas like menstrual regularity, androgen-related symptoms (such as acne or unwanted hair growth), and insulin resistance. Additionally, take note of how your energy levels, mood, and overall well-being evolve over time - these are crucial signs of progress.
It's also essential to consider the therapy’s safety, affordability, and practicality. Regularly check your progress - at intervals like 4 weeks, 3 months, and 6 months - by reviewing changes in weight, hormone levels, and symptoms. If you’re consistently hitting your goals and feeling better, it’s a good indication that the therapy is effective for you. Programs like those offered by Oana Health provide personalized, prescription-based support to help you monitor these metrics, making it easier to stay on track and measure your success.
What are the possible side effects of PCOS weight loss medications?
Weight loss medications often prescribed for PCOS, like metformin and GLP-1 receptor agonists such as semaglutide (e.g., Ozempic®, Wegovy®), can be effective but may come with side effects. The most common issues are digestive-related, including nausea, diarrhea, vomiting, and constipation. Other symptoms like fatigue, dizziness, and changes in appetite may also arise, especially when adjusting dosages.
Though less frequent, more serious side effects have been reported with GLP-1 medications. These include pancreatitis, gallbladder problems, or thyroid-related concerns. Severe complications, such as lactic acidosis or liver toxicity, are extremely rare. To reduce discomfort, healthcare providers - like those at Oana Health - typically start patients on a low dose, gradually increasing it over time. They also suggest strategies like eating smaller, low-fat meals, staying hydrated, and ensuring regular check-ups.
Being aware of these potential side effects allows patients to weigh the benefits of improved insulin sensitivity and weight loss against any temporary challenges they might experience.
How can I create a personalized and sustainable PCOS weight loss plan?
A tailored approach to managing PCOS-related weight loss begins with understanding your individual hormonal balance, insulin resistance, BMI, and specific symptoms. This groundwork helps create a plan that focuses on four main areas: balanced nutrition, exercise, weight management, and stress reduction. Even a small weight loss of 5–10% can lead to noticeable improvements in symptoms like irregular cycles, acne, and unwanted hair growth.
To keep the plan manageable and long-lasting, integrate healthy habits into your everyday life. Choose meals packed with fiber, lean proteins, healthy fats, and fermented foods, while cutting back on processed and sugary options. Pair strength training (2–3 times a week) with at least 150 minutes of moderate cardio each week to boost metabolism and preserve lean muscle. Make sleep a priority - aim for 7–9 hours of quality rest - and explore stress-relief practices like mindfulness or yoga to stay on track.
For many, PCOS management also involves prescription treatments. Telehealth platforms like Oana Health offer customized plans created by licensed professionals. These services provide medications delivered straight to your door and virtual check-ins to fine-tune your therapy as needed, ensuring your plan adapts to your progress and stays effective over time.
