Coping with PCOS Infertility: Mental Health Tips
Struggling with PCOS-related infertility can feel overwhelming, but there are ways to manage the emotional toll and improve your well-being. Women with PCOS are more likely to experience depression, anxiety, and stress due to hormonal imbalances, physical symptoms, and fertility challenges. Yet, practical strategies like mindfulness, self-care routines, and support networks can make a difference.
Key Takeaways:
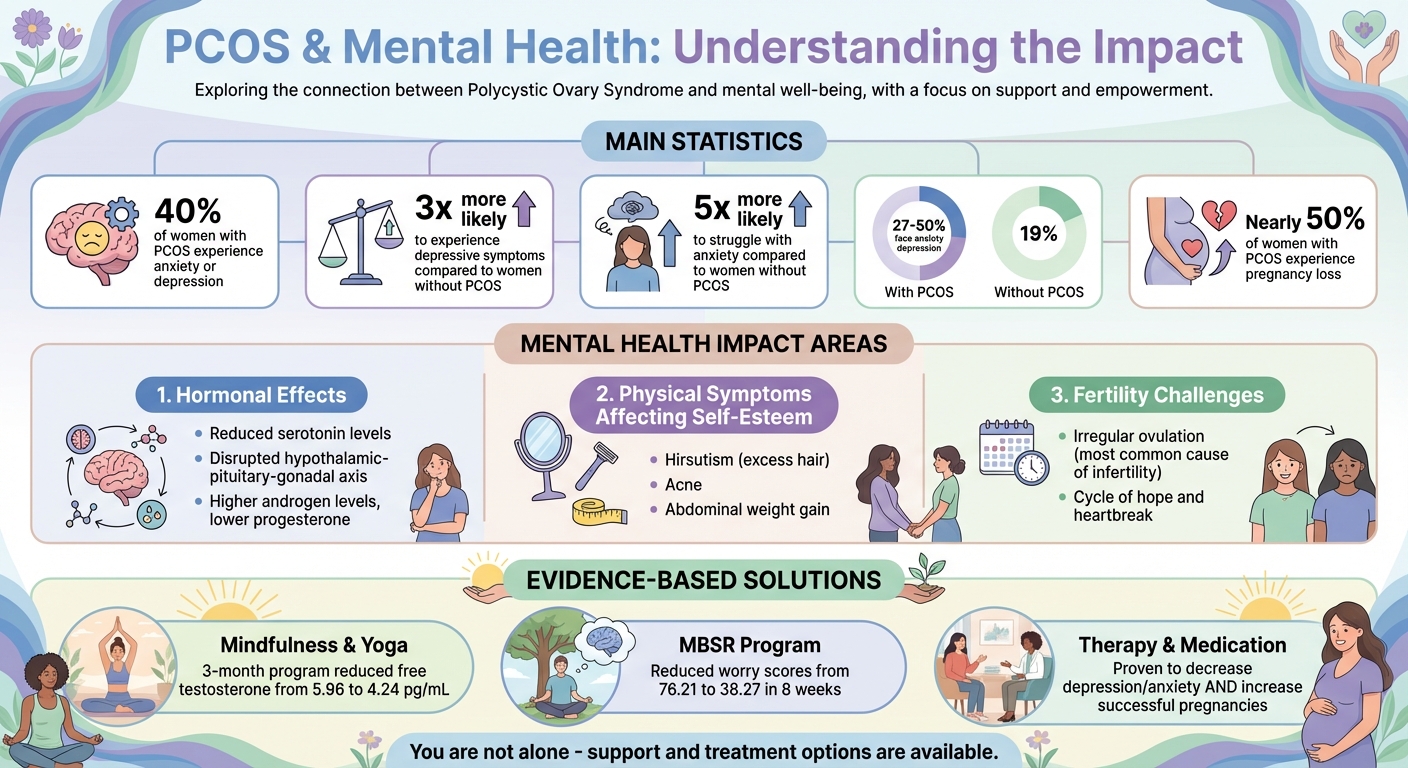
- PCOS impacts mental health, with up to 40% of women diagnosed with anxiety or depression.
- Stress management techniques, like mindfulness and yoga, can reduce emotional distress and even improve fertility outcomes.
- Building a support network, including peer groups and professional therapy, helps address feelings of isolation and grief.
- Lifestyle changes, such as a nutrient-rich diet, regular exercise, and better sleep habits, can support both mental and physical health.
PCOS Mental Health Statistics and Impact on Women's Well-being
Polycystic Ovary Syndrome (PCOS) and Mental Health
The Emotional Impact of PCOS-Related Infertility
Dealing with PCOS-related infertility goes far beyond the physical symptoms - it takes a heavy emotional toll. The struggle to conceive often brings feelings of sadness and isolation, leaving many women caught in a relentless cycle of hope and heartbreak. These emotions are deeply tied to biological changes happening within the body. Let’s dive into the science behind these challenges.
How PCOS Affects Fertility and Mental Health
PCOS disrupts the hypothalamic-pituitary-gonadal axis, which leads to higher androgen levels and lower progesterone due to irregular ovulation. This hormonal imbalance not only impacts fertility but also influences mood. Irregular ovulation is one of the most common causes of infertility in women with PCOS.
The link between these hormonal shifts and mental health is more profound than many realize. Women with PCOS often experience reduced levels of serotonin, the chemical in the brain that helps regulate mood. Insulin resistance, another hallmark of PCOS, contributes to fatigue and irritability, while chronic inflammation linked to insulin resistance has been directly associated with depressive symptoms.
"Sudden fluctuations in hormones may result in unpredictable mood changes... High androgen levels can affect brain function and mood regulation." - Women's Care of Beverly Hills
Physical symptoms add another layer to the emotional burden. Hirsutism (excess facial or body hair), acne, and abdominal weight gain can erode self-esteem and negatively impact body image, both of which are closely tied to depression. Concerns about infertility and weight often lead to a lower quality of life for women managing PCOS.
Common Emotional Reactions to Infertility
The emotional challenges of PCOS-related infertility often include grief, frustration, hopelessness, and mood swings. These responses aren’t personal failings - they’re natural reactions to a difficult medical condition. Studies suggest that women with PCOS may have an altered biological stress response, which could heighten their reactions to everyday stressors.
"PCOS is one of the main causes of infertility. The mere thought or reality of struggling to conceive can be emotionally draining, leading to feelings of sadness, frustration, and anxiety." - Daniel S. Kushner, MD, Board-certified OB/GYN
Acknowledging and addressing these emotions is crucial because they are treatable. Healthcare providers should screen for depression and anxiety as part of a PCOS diagnosis. Without proper intervention, the chronic nature of PCOS can intensify emotional challenges over time, affecting not just fertility but overall quality of life. Understanding these emotional hurdles is key to developing effective stress management and self-care strategies.
Managing Stress to Build Emotional Strength
Managing stress is essential not only for emotional well-being but also for creating a supportive environment for fertility. Stress levels tend to rise with the challenges of infertility and physical symptoms, which in turn worsen conditions like insulin resistance and PCOS through elevated cortisol levels. Hormonal imbalances linked to PCOS amplify stress, making it crucial to adopt effective coping strategies. Women with PCOS are three times more likely to experience heightened emotional stress compared to those without the condition. Breaking this cycle requires practical tools to reduce stress and build emotional resilience.
Interestingly, research has found that addressing depression and anxiety through stress management can increase the likelihood of successful pregnancies. This goes beyond just improving mood - it's about fostering both mental and physical recovery. The key lies in developing consistent habits that help regulate emotions and lower stress levels.
Using Mindfulness and Relaxation Methods
Mindfulness techniques offer practical ways to manage the emotional burden of infertility. For example, an 8-week Mindfulness-Based Stress Reduction (MBSR) program significantly reduced worry scores in women with PCOS, dropping from 76.21 to 38.27 within just one month of follow-up. These programs often include practices like mindful eating, body scans, sitting meditation, and mindful walking, all designed to ease psychological distress.
Being present in the moment can help you respond to stress more thoughtfully, which is particularly helpful for reducing depression and emotional eating associated with PCOS.
Simple breathing exercises, like the 4-7-8 technique, can calm the body's stress response. This involves inhaling for four counts, holding the breath for seven, and exhaling for eight. For deeper relaxation, try Progressive Muscle Relaxation (PMR) - a method where you tense and release muscle groups one at a time, working from head to toe, to release physical tension.
Mindful yoga is another powerful tool for managing PCOS. A 3-month yoga program, practiced three times a week, lowered free testosterone levels from 5.96 to 4.24 pg/mL in women with PCOS, while also improving anxiety and depression scores. Researcher Vishesha Patel highlights its benefits:
"The improvements observed suggest that regular mindful yoga practice can be a useful complementary therapeutic option for women with PCOS, particularly for improving serum androgen levels."
For a quick mindfulness boost, the Three-Minute Breathing Space (3MBS) encourages you to step out of "autopilot" mode and tune into your current thoughts and body sensations. Another simple exercise is the "Raisin Exercise," where you focus intently on the texture, smell, and taste of a single raisin to practice mindful eating. Apps like FertiCalm offer cognitive and behavioral tools tailored to infertility stress, while Calm and Headspace provide general guided meditations.
Incorporating these mindfulness practices into your daily routine can help strengthen your emotional resilience over time.
Creating a Self-Care Routine
Complementing mindfulness practices with a self-care routine can provide a sense of control in the face of an unpredictable condition. This approach helps quiet negative thoughts and boosts self-esteem. Addressing physical, emotional, mental, social, and spiritual needs through self-care contributes to your ability to handle infertility challenges. What's most important is consistency - short, regular self-care sessions are often more effective for mental health than occasional, lengthy ones.
Start by improving sleep hygiene. Turn off electronics at least an hour before bed and stick to a consistent sleep schedule to help regulate hormones and reduce fatigue. Poor sleep disrupts cortisol levels, which can make managing stress during the day more difficult. Avoid caffeine or heavy meals in the hours leading up to bedtime to help your body better handle stress hormones.
Journaling is another effective way to process emotions and pinpoint stress triggers. Setting clear social boundaries can also protect your emotional energy and limit interactions that increase stress. Dr. Nazanin E. Silver, an obstetrician-gynecologist and psychiatrist, explains the value of this:
"Just knowing that you're not alone can be a huge relief. You'll also learn how to deal with the ideas and thoughts that cause stress, anxiety, and depression."
If you miss a planned self-care activity, reschedule it instead of canceling. This reinforces the importance of prioritizing your emotional health. Incorporate affirmations like "I am worthy" and calming practices like aromatherapy with lavender to nurture self-worth and promote relaxation.
Building a Support Network
Adding to stress management techniques, creating a strong support network can significantly boost your emotional resilience. Alongside mindfulness and self-care, connecting with compassionate individuals plays a key role in overall well-being. For women with PCOS, these networks can make it easier to stick with lifestyle changes and stay engaged with treatment plans. The focus should be on quality, not quantity - a small circle of understanding individuals can make all the difference.
Between 27% and 50% of women with PCOS face anxiety or depression, compared to 19% of women without the condition. Building connections with others who share similar experiences can create a sense of validation and comfort that medication alone often cannot provide. Dr. Nazanin E. Silver, an obstetrician-gynecologist and psychiatrist, highlights this:
"Just knowing that you're not alone can be a huge relief".
Your support network can include healthcare providers, family, friends, and peer groups who understand the challenges - both physical and emotional - of PCOS. Sharing experiences with others helps normalize your journey and reminds you that you’re not facing it alone.
Talking with Loved Ones
When dealing with infertility, open communication with your partner, family, and friends is essential - but it’s equally important to establish boundaries. For example, attending medical appointments with your partner can help them better understand the clinical and emotional aspects of PCOS. This shared experience can strengthen your bond and reduce feelings of isolation within your relationship.
Before diving into intensive fertility treatments, have honest conversations with your partner about potential outcomes and alternative family-building paths, such as adoption. If communication becomes strained, couples therapy or professionally-led support groups can provide a neutral space to work through emotions.
Setting boundaries is crucial for protecting your mental health. Dr. Silver offers this advice:
"With friends and family, try to set boundaries with those who say things that bother you. If someone's behavior keeps hurting you, you could limit contact or even end contact temporarily".
It’s okay to decline invasive questions about family planning or distance yourself from relationships that consistently cause emotional harm. Preparing simple, polite responses for social situations can help you feel more in control when faced with insensitive comments.
In addition to personal conversations, structured support groups can provide a safe space for shared understanding and emotional support.
Joining PCOS and Infertility Support Groups
Support groups offer a welcoming environment to share fears, triumphs, and emotional struggles with others who truly understand. They can be especially helpful in combating the isolation that often comes with PCOS symptoms like weight gain, acne, and hirsutism. Participating in these groups not only provides emotional relief but can also boost self-esteem and counter feelings of depression.
There are two main types of support groups to consider:
- Peer-led groups: These are run by trained volunteers who share similar experiences. They are usually free and focus on resource sharing and mutual understanding.
- Professionally-led groups: Facilitated by licensed therapists, these groups provide a structured setting to work through deeper emotional challenges. They often involve a fee and typically include 8–10 participants.
Here’s a quick comparison:
| Support Type | Led By | Primary Goal | Cost |
|---|---|---|---|
| Peer-Led Group | Volunteers/Peers | Connection and shared experience | Generally Free |
| Professionally-Led Group | Licensed Therapists | Processing emotional trauma/grief | Often Fee-based |
To find a group, ask your doctor or fertility specialist for recommendations. You can also explore resources from organizations like RESOLVE: The National Infertility Association or PCOS Challenge: The National Polycystic Ovary Syndrome Association, the largest advocacy group for PCOS. If you’re hesitant to share at first, consider joining a peer-led "drop-in" group to observe and decide how much you’re comfortable disclosing.
Virtual groups are another great option, especially if you live in a remote area or have a packed schedule. These online spaces allow you to connect with others on specific topics from anywhere. For daily encouragement, follow Instagram accounts like @pcossupportgirl, @pcos.positivity, or @thatpcoscoach. Experiment with different types of groups until you find one that feels right for you.
sbb-itb-6dba428
Getting Professional Mental Health Support
Building on earlier strategies, seeking professional mental health support can provide targeted tools to break the cycle of emotional distress often tied to PCOS-related infertility. Research shows that women with PCOS are three times more likely to experience depressive symptoms and five times more likely to struggle with anxiety compared to those without the condition. This stems from hormonal imbalances that affect neurotransmitters like serotonin, dopamine, and GABA.
Dr. Nazanin E. Silver, an OB-GYN and women's behavioral health psychiatrist, highlights the importance of addressing mental health:
"Talk with your doctor about treating depression and anxiety with medication and therapy. These treatments are proven to work. They are shown to decrease levels of depression and anxiety and even increase the number of successful pregnancies."
Therapy can play a crucial role in breaking the connection between mental distress and physical symptoms. Anxiety and depression often sap the motivation needed to stick with the lifestyle changes crucial for managing PCOS, which can, in turn, worsen symptoms and deepen emotional challenges. This creates a compelling case for targeted therapy options.
Therapy Options for Anxiety and Depression
Cognitive Behavioral Therapy (CBT) is widely regarded as the most effective evidence-based treatment for managing PCOS-related anxiety and depression. This structured approach helps individuals identify and change distorted thought patterns - like rumination, overgeneralization, and catastrophic thinking - that can amplify the emotional struggles associated with infertility.
Studies show that group CBT not only reduces depression and anxiety scores but also improves quality of life. When paired with lifestyle changes, it can even enhance weight loss outcomes.
CBT provides tools that foster lasting improvements, such as:
- Cognitive reframing: Replace negative, distressing thoughts with more balanced and realistic perspectives.
- Behavioral activation: Build motivation to implement and sustain lifestyle changes that support PCOS management.
- Stress management: Practice relaxation techniques to lower cortisol levels, which can otherwise worsen inflammation and hormonal imbalances.
Other therapy options include couples therapy, which can address relationship strain caused by infertility, and grief counseling, which may help process the pain of pregnancy loss - a challenge faced by nearly half of women with PCOS.
Telehealth for Mental Health Support
If in-person therapy isn’t accessible, telehealth offers a convenient alternative. Virtual therapy sessions provide flexibility, privacy, and ease of access - especially for those who may feel self-conscious about visible PCOS symptoms like hirsutism or weight gain.
Platforms like Oana Health integrate mental health support into a comprehensive PCOS care plan. Oana Health connects you with licensed medical professionals who understand the emotional toll of hormonal imbalances and infertility. Their services include personalized, prescription-based treatments - such as Bupropion XL for mental health support at $25 per month. After an online consultation, medications are shipped directly to your home with free shipping, eliminating the hassle of pharmacy visits. This approach addresses both the physical and emotional aspects of PCOS, creating a more cohesive care experience.
When selecting a telehealth provider, prioritize services that offer multidisciplinary care. Look for platforms that combine expertise in endocrinology, psychiatry, and nutrition. Regular mental health screenings should also be part of your ongoing PCOS management, ensuring both hormonal and emotional needs are addressed comprehensively.
Lifestyle Changes for Better Mental and Physical Health
While professional therapy plays a vital role, small, everyday adjustments can make a big difference in improving both mental and physical health. For individuals with PCOS-related infertility, factors like diet, exercise, and sleep have a profound impact. Dr. Shruthi Mahalingaiah, a reproductive endocrinologist, sums it up perfectly:
"Health optimization in people with PCOS is sensitive to a lot of things - especially the things we eat and drink, our sleep-wake cycle, and physical activity".
These changes not only help balance hormones but also build emotional resilience.
How Nutrition Affects Mental Health
What you eat directly influences the brain chemicals that regulate mood, such as serotonin and dopamine. Women with PCOS often have lower levels of these neurotransmitters, which can lead to feeling unmotivated or anxious. Thoughtful dietary choices can help restore this balance, while also addressing insulin resistance - a key factor behind many PCOS symptoms. These dietary adjustments can also support fertility by stabilizing hormones.
For example, a 2024 study published in the British Journal of Nutrition found that women with PCOS who followed the MIND diet for eight weeks experienced notable reductions in depression and anxiety compared to those on typical diets. The MIND diet, which blends Mediterranean and DASH principles, focuses on foods like berries, leafy greens, and whole grains. These are packed with antioxidants that combat inflammation, a factor often linked to mood disorders.
Here are some practical tips for improving nutrition:
- Increase fiber intake: Aim for 40 grams daily from sources like beans, lentils, oats, or apples. Fiber not only supports weight management but also stabilizes blood sugar, which helps maintain a steady mood.
- Incorporate omega-3s: Add a tablespoon of ground flaxseed or chia seeds to your meals, or snack on a handful of walnuts. These healthy fats reduce inflammation and support emotional well-being.
-
Try plant-based proteins: A 2018 clinical trial showed that replacing 35% of daily animal protein with soy-based options like tofu or tempeh led to reductions in BMI, fasting blood sugar, and testosterone levels for women with PCOS. As registered dietitian Stephanie McBurnett advises:
"Embrace a plant-based diet abundant in fiber and other hormone-regulating compounds, such as soy, to effectively ease numerous painful symptoms and regain control over hormone balance".
- Opt for low-glycemic foods: Swap white bread and rice for options like pumpernickel bread, barley, or quinoa. This helps prevent insulin spikes, which can worsen both physical and emotional symptoms.
Plant-based diets are also effective at reducing harmful compounds called advanced glycation end products (AGEs), which are linked to insulin resistance and inflammation.
Adding Physical Activity to Your Daily Routine
Exercise is another powerful way to address the stress and hormonal imbalances tied to PCOS-related infertility. Different types of exercise offer unique benefits, so a mix of activities is ideal.
- High-Intensity Interval Training (HIIT): Studies show that HIIT can significantly reduce depression and anxiety symptoms in women with PCOS.
- Moderate-intensity aerobic exercise: Activities like brisk walking, cycling, or swimming are particularly effective for reproductive health. They can regulate menstrual cycles and stimulate ovulation, tackling one of the core fertility challenges in PCOS. Aim for 150 minutes per week, broken into 30-minute sessions.
- Strength training: Resistance exercises, such as squats, lunges, and push-ups, improve insulin sensitivity while lowering testosterone and cholesterol levels. You don’t need a gym - bodyweight exercises at home work just as well. Two to three sessions per week can make a noticeable difference.
- Mind-body practices: Yoga and meditation can reduce cortisol levels (the stress hormone) while improving mental clarity. Even 10 minutes of stretching or breathing exercises can help ease anxiety and support your overall well-being.
By combining regular exercise with other lifestyle changes, you can alleviate stress and improve symptoms that impact fertility.
Getting Better Sleep for Emotional Health
Quality sleep is essential for maintaining hormonal balance. Poor sleep not only worsens insulin resistance but also increases the risk of depressive symptoms. Women with PCOS are more than twice as likely to experience depression compared to those without the condition. For those dealing with infertility, sleep deprivation can amplify metabolic disruptions and inflammation, further complicating ovulation.
Additionally, women with PCOS are at higher risk for obstructive sleep apnea, a condition linked to insulin resistance and cognitive issues. If you find yourself excessively tired during the day or waking up gasping for air, it’s worth discussing a sleep apnea screening with your doctor.
To improve sleep quality, try these steps:
- Stick to a consistent bedtime routine and aim for 7 to 9 hours of uninterrupted rest each night.
- Create a sleep-friendly environment by keeping your bedroom cool, dark, and quiet.
- Limit screen time at least an hour before bed, as blue light interferes with melatonin production.
As Summit Health highlights:
"Managing PCOS actually works best when you focus on building sustainable habits... Good sleep is crucial. Your hormones and mood depend on it".
If sleep issues persist, Oana Health offers personalized support, addressing both the physical and mental health challenges of PCOS. Their licensed professionals can help identify underlying problems, such as insulin resistance or anxiety, and provide tailored treatment plans delivered right to your door with free shipping.
Coping Strategies for Emotional Overwhelm
Building on earlier discussions about support networks and lifestyle changes, let's dive into strategies for managing emotional overwhelm head-on. Even the most solid support system can feel strained during moments of intense emotional distress - whether it's a pregnancy announcement, a failed treatment cycle, or a challenging family gathering. In those moments, these quick and effective coping techniques can help you regain a sense of control.
Grounding and Breathing Techniques
When panic sets in, deep, controlled breathing can work wonders to calm your nervous system. Pair this with grounding exercises, like the "5-4-3-2-1" method, to bring your focus back to the present. Here's how it works: identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste. This simple exercise interrupts racing thoughts and anchors you to your surroundings.
For additional support, mindfulness apps like Headspace offer guided meditations that can help you navigate overwhelming emotions. These techniques are not just about calming down in the moment - they also prepare you to handle emotionally charged social situations with greater ease.
Setting Boundaries in Social Situations
Sometimes, protecting your emotional health means giving yourself permission to say "no." Skipping events like baby showers or family gatherings isn't about avoidance - it's about prioritizing your well-being. Dr. Nazanin E. Silver, an ob-gyn and psychiatrist, emphasizes:
"With friends and family, try to set boundaries with those who say things that bother you. If someone's behavior keeps hurting you, you could limit contact or even end contact temporarily".
When it comes to discussing infertility with your partner, the "Twenty Minute Rule" can be a game-changer. Limit these conversations to 20 minutes per evening. Use a timer if necessary, so these discussions don't dominate your relationship. During these talks, be clear about what you need - whether that's a listening ear, a comforting hug, or just some quiet time to process.
Practicing Self-Compassion
One of the hardest habits to break is blaming yourself for feeling bad in the first place. RESOLVE: The National Infertility Association puts it perfectly:
"The first step in reducing the stress of infertility is to stop feeling panicky about feeling rotten!"
It's completely normal to feel anger, grief, or frustration. Studies show that 28% to 39% of women with PCOS experience anxiety disorders, while 11% to 25% face depression. Struggling doesn't make you weak - it makes you human.
Instead of pressuring yourself to "snap out of it", allow space for your emotions. Cry if you need to after hearing pregnancy news. Feel anger about the unfairness of the situation. These feelings need acknowledgment, not suppression. Research even shows that self-compassion therapy can alleviate mood disturbances, anxiety, and body image concerns tied to PCOS. Treat yourself with the same kindness you'd extend to a friend going through something similar. By practicing self-compassion, you're reinforcing the resilience strategies shared earlier, helping you move forward with greater strength.
Conclusion
Dealing with PCOS-related infertility can deeply affect both your body and mind. In fact, 40% of women with PCOS experience anxiety or depression. This highlights just how important it is to prioritize mental health alongside physical care.
Taking steps to support your emotional well-being can have a positive ripple effect. Techniques like therapy, mindfulness, or lifestyle adjustments not only help reduce stress but might also improve hormonal balance and fertility outcomes. Dr. Nazanin E. Silver, an ob-gyn and psychiatrist, explains:
"These treatments [medication and therapy] are proven to work. They are shown to decrease levels of depression and anxiety and even increase the number of successful pregnancies".
This powerful link between mental health and physical outcomes emphasizes the need for a well-rounded approach. You don’t have to navigate this alone. Tools like grounding exercises, setting boundaries, or exploring Cognitive Behavioral Therapy can make a difference. As Dr. Lora Shahine puts it:
"One of the main reasons people stop fertility treatment is not because of lack of resources, but because of depression, anxiety and lack of support for mental health".
If you're looking for personalized care, Oana Health provides telehealth services designed to address both the physical and emotional challenges of PCOS. Their offerings include treatments for insulin resistance, like Oral Metformin ER (starting at $22/month), and mental health options, such as Bupropion XL ($25/month). Licensed physicians craft tailored plans, delivered straight to your door with free shipping.
FAQs
Can mindfulness help improve fertility for women with PCOS?
Mindfulness practices like meditation, deep breathing, and mindfulness-based programs can play a helpful role in supporting fertility for women with PCOS. Stress, a common trigger for hormonal imbalances, can interfere with regular ovulation. By promoting a calmer state of mind, mindfulness helps the body regulate hormones more effectively.
Studies have shown that mindfulness can reduce cortisol levels, enhance insulin sensitivity, and alleviate symptoms of anxiety and depression - factors that often contribute to PCOS-related hormonal challenges. Women who incorporate mindfulness into their routine may notice more consistent ovulation, which can improve their chances of conception.
For those seeking tailored support, Oana Health provides telehealth services that integrate mindfulness coaching with proven PCOS treatments. Their offerings include hormone regulation, weight management, and mental health care, all delivered by licensed clinicians. With everything shipped directly to your home, it’s easier than ever to make mindfulness a part of your fertility journey.
How can nutrition help manage mental health challenges linked to PCOS-related infertility?
Nutrition plays a crucial role in supporting mental health for those managing PCOS. The food you eat directly influences hormones and metabolic processes that can trigger anxiety, depression, and mood swings. A diet rich in low-glycemic carbs, high-fiber foods, lean proteins, and healthy fats can help stabilize insulin and androgen levels, addressing the hormonal imbalances that often impact emotional well-being.
Adding nutrient-packed foods like leafy greens, non-starchy vegetables, whole grains, nuts, seeds, and omega-3-rich fish can boost energy levels and reduce brain fog. This makes it easier to stay active, manage stress, and maintain focus. Eating regular, evenly spaced meals can also curb binge eating caused by insulin resistance, fostering a healthier relationship with food and further supporting mental health.
For personalized support, Oana Health offers telehealth consultations with licensed professionals who can develop customized nutrition plans and treatments to help manage both the mental and physical challenges of PCOS.
Why is having a support system important for managing PCOS-related infertility?
Having a solid support system is crucial when navigating PCOS-related infertility. It can help ease feelings of isolation and emotional overwhelm. Connecting with people who truly understand what you're going through can bring a sense of comfort, validation, and even practical advice. Whether it's through sharing stories or exchanging strategies in a community - be it in-person or online - this connection can make the journey feel less solitary, while also reducing stress and boosting mental well-being.
Support networks can also be a great source of information. From exploring treatment options to sharing tips on diet, exercise, and managing stress, these connections can provide tools to help you tackle the challenges of infertility. Since stress can exacerbate hormonal imbalances, having people to rely on can make it easier to stick to your care plan. For professional support, Oana Health offers personalized telehealth services focused on PCOS and mental health. Their science-backed approach provides a convenient way to feel more in control and supported throughout your journey.
