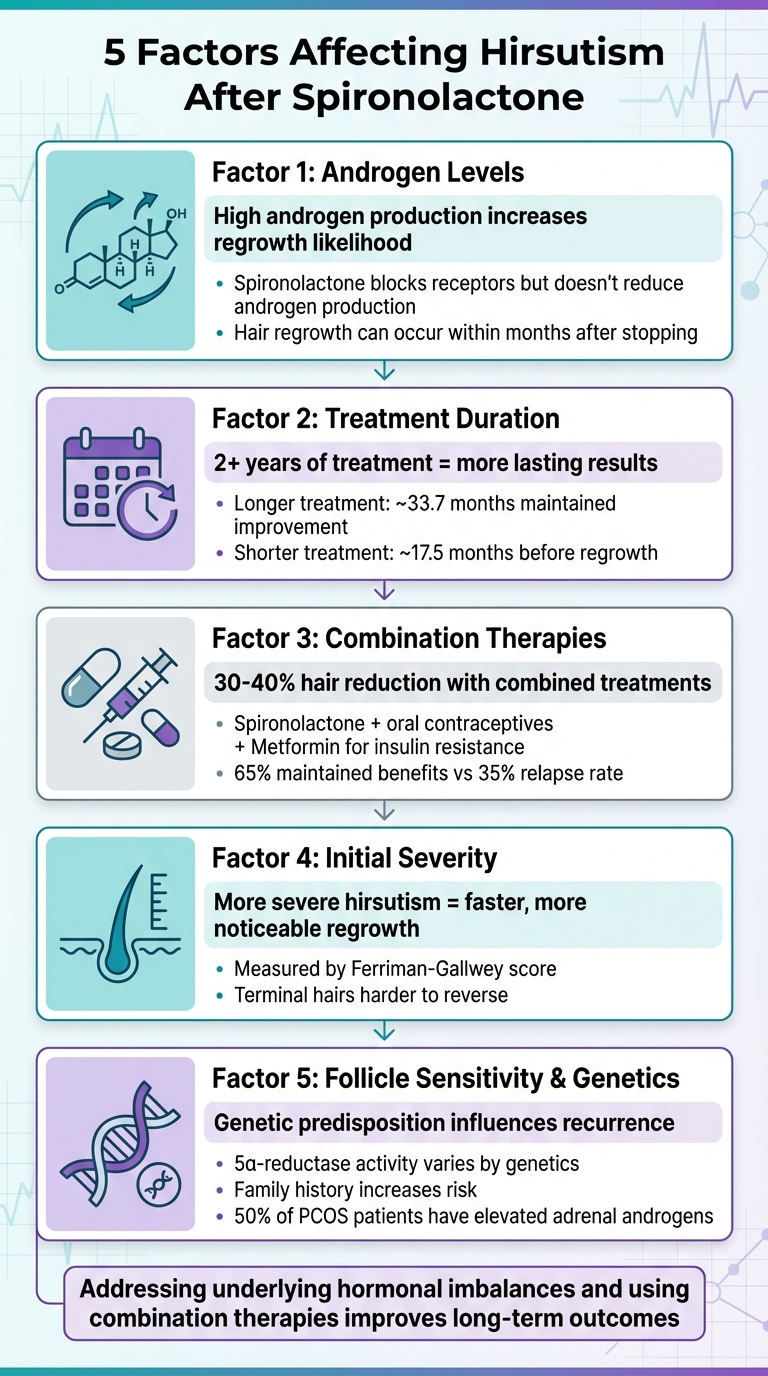
Hirsutism, or excessive male-pattern hair growth in women, often stems from hormonal imbalances like PCOS. Spironolactone is a widely used treatment that blocks androgen receptors, reducing hair growth over time. However, its effects are temporary, and hair can return after discontinuation. Here are the five main factors influencing this recurrence:
- Androgen Levels: High androgen production (e.g., from PCOS or adrenal issues) increases the likelihood of hair regrowth.
- Treatment Duration: Longer use (2+ years) typically leads to more lasting results.
- Combination Therapies: Pairing spironolactone with other treatments, like oral contraceptives or metformin, helps maintain improvements.
- Initial Severity: Women with more severe hirsutism often experience faster and more noticeable regrowth.
- Follicle Sensitivity & Genetics: Genetic predisposition and follicle sensitivity to androgens play a major role in recurrence.
Addressing underlying causes, such as hormonal imbalances or insulin resistance, and using combination therapies can improve long-term outcomes. Personalized care is essential for managing symptoms effectively.
5 Key Factors Affecting Hirsutism Recurrence After Stopping Spironolactone
1. Your Body's Androgen Levels
Impact on Hirsutism Recurrence
A key factor in whether unwanted hair returns after stopping spironolactone is your body's baseline androgen production. Hirsutism occurs when excess androgens - mainly testosterone from the ovaries and DHEA-S from the adrenal glands - bind to hair follicle receptors, triggering male-pattern hair growth. Spironolactone helps by blocking these androgen receptors, but it doesn’t reduce the actual production of androgens. Once spironolactone is discontinued, high androgen levels can cause hair to regrow within months.
Women with persistently high androgen levels - due to conditions like untreated PCOS, adrenal hyperandrogenism, or insulin resistance - are more likely to experience hair regrowth. On the other hand, women whose hormone imbalances have been treated or whose androgen levels are closer to normal tend to see longer-lasting results after stopping spironolactone. This highlights the importance of addressing underlying hormonal issues for better long-term outcomes.
Clinical Evidence or Research Backing
Research has consistently shown spironolactone's effectiveness in reducing hair growth, but also its limitations. A 1975 study involving 30 women with hirsutism revealed that while spironolactone lowered hair growth and serum testosterone levels, it didn’t resolve the root cause of excess androgen production. More recent studies observed mixed results: one tracked women with hyperandrogenic conditions and found that, after an average of 25.7 months on spironolactone, 38 women maintained improvement for about 33.7 months post-treatment, while 20 experienced hair regrowth after roughly 17.5 months. Interestingly, testosterone levels alone didn’t reliably predict these outcomes.
These findings suggest that individual hormonal dynamics and genetic predispositions play a significant role in determining how effective treatment will be over the long term.
Influence of Hormonal and Genetic Factors
Your hormonal feedback systems are central to managing androgen levels and the risk of hirsutism. For example, insulin resistance, common in PCOS, can elevate testosterone and lower SHBG (sex hormone-binding globulin), increasing the amount of free testosterone in the body. Additionally, genetic factors or heightened 5-alpha reductase activity can make hair follicles more sensitive to even small increases in androgens, leading to hair regrowth.
Some women develop idiopathic hirsutism despite having normal androgen levels. This condition often stems from increased hair follicle sensitivity to androgens, influenced by genetic factors or enhanced 5-alpha reductase activity, which converts testosterone into the more potent dihydrotestosterone (DHT). Stress and inflammation can also exacerbate androgen production, particularly in women with PCOS, where up to 50% experience elevated adrenal androgens like DHEA-S.
Effectiveness of Treatment Combinations
Since spironolactone focuses solely on blocking androgen receptors, combining it with therapies that reduce androgen production can help maintain results for longer. Elevated androgens drive hair regrowth, so targeting these levels through additional treatments strengthens the overall effectiveness. For instance, oral contraceptives containing low-androgenic or anti-androgenic progestins can suppress ovarian testosterone production and increase SHBG, thereby lowering free androgen levels when used alongside spironolactone. Similarly, addressing insulin resistance through lifestyle changes like moderate weight loss, regular exercise, or medications such as metformin can help reduce insulin-driven androgen production and boost SHBG over time.
For women in the U.S. looking for comprehensive care, telehealth platforms like Oana Health offer personalized treatment plans for PCOS, insulin resistance, and unwanted hair. These services provide prescription-based solutions delivered to your doorstep, guided by licensed medical professionals. By tackling multiple contributing factors simultaneously, combined approaches can slow the recurrence of hirsutism after spironolactone is discontinued.
2. How Long You Used Spironolactone
Impact on Hirsutism Recurrence
Taking spironolactone for at least two years tends to offer longer-lasting results compared to shorter treatment durations. A retrospective study found that women who used spironolactone for extended periods maintained improvements for nearly three years on average. In contrast, those with shorter courses of treatment experienced hair regrowth much sooner. Women with ovulatory PCOS, who typically undergo shorter treatment courses, often see symptoms return earlier than those with classic PCOS. This highlights that the length of treatment plays a crucial role, separate from initial androgen levels.
Clinical Evidence or Research Backing
In an early trial involving 30 women with hirsutism, significant hair reduction was observed within 3 to 5 months, along with a drop in testosterone levels. Longer-term studies have shown that while most participants experienced noticeable improvements in hirsutism and other hyperandrogenic symptoms during treatment, symptoms often return about a year after stopping antiandrogen therapy. This suggests that spironolactone effectively manages symptoms but does not address the root cause of the condition.
Effectiveness of Treatment Combinations
Since hirsutism tends to gradually return after stopping spironolactone - even with prolonged use - combining treatments can extend the benefits. Using spironolactone alongside oral contraceptives or targeting underlying issues like insulin resistance can help maintain results and reduce the chances of rebound hair growth after discontinuation. Combining extended treatment with these additional therapies offers better symptom control and delays hair regrowth.
3. Single Treatment vs. Combined Treatments
Impact on Hirsutism Recurrence
Spironolactone on its own can improve hirsutism, but when it comes to reducing hair regrowth long-term, combination treatments tend to be more effective. Here's why: spironolactone works by blocking androgen receptors in hair follicles, but it doesn't address the underlying hormonal imbalances. As a result, once the treatment stops, unwanted hair often makes a comeback. Some clinical observations even suggest that hair regrowth can start around 17–18 months after discontinuing spironolactone.
On the other hand, combined treatments tackle the issue from multiple angles. For instance, pairing spironolactone with oral contraceptives not only blocks androgen receptors but also reduces ovarian androgen production and boosts sex hormone–binding globulin levels. This lowers free testosterone in the body. For women dealing with PCOS or insulin resistance, adding metformin or focusing on weight management can address the metabolic factors that contribute to excess androgen production. This approach ties in with the previously discussed roles of androgen levels and treatment duration, offering a more comprehensive solution.
Clinical Evidence or Research Backing
Studies back up the advantage of combination therapies. Research shows that high-dose spironolactone alone can reduce hirsutism in more than two-thirds of women. However, when spironolactone is combined with oral contraceptives or insulin-sensitizing agents, the results are often more consistent. Improvements in hair growth reduction typically range between 30–40% after 6–12 months of combined treatment.
The difference becomes even more apparent when considering underlying conditions. For example, up to 50% of women with PCOS have elevated adrenal androgens. While spironolactone can help with symptoms, it doesn't fully address insulin resistance, which can drive ovarian androgen production. This means that monotherapy might not be enough for PCOS patients, as it doesn't tackle the root causes. Addressing these metabolic issues through a combined approach can help prevent unwanted hair from returning.
Effectiveness of Treatment Combinations
Combination treatments not only extend the benefits but also slow the recurrence of hirsutism. Women who use spironolactone alongside oral contraceptives and insulin-sensitizing therapies often experience slower and less severe hair regrowth compared to those relying solely on spironolactone. This multifaceted approach, which can also include cosmetic treatments like laser hair removal, is increasingly recommended in modern medical guidelines because it targets multiple factors at once.
Many clinicians suggest starting with a combination regimen, such as 100–200 mg of spironolactone with oral contraceptives. For women with PCOS, adding lifestyle changes - like improved diet and exercise - and insulin-sensitizing medications can further enhance long-term results. When it's time to stop spironolactone, tapering the dose gradually under a doctor’s supervision is often recommended to reduce the risk of rebound effects. Keeping up with other therapies during this time can help maintain progress and ensure more lasting results.
4. How Severe Your Hirsutism Was at the Start
Impact on Hirsutism Recurrence
The severity of hirsutism at the beginning of treatment plays a key role in how quickly and significantly hair regrowth occurs after stopping spironolactone. Women who start with more severe hirsutism are at a higher risk of noticeable and faster regrowth. This happens because severe cases often involve more established terminal hairs, which are harder to reverse . Androgen levels also heavily influence these outcomes, further linking initial severity to treatment results.
To assess hair growth in androgen-sensitive areas, clinicians rely on the Ferriman–Gallwey score. Higher scores indicate stronger androgen influence and predict quicker regrowth. While women with mild hirsutism may also notice some changes after stopping spironolactone, the regrowth tends to be slower and less pronounced, especially when hormonal and metabolic factors are well-managed .
Clinical Evidence or Research Backing
Research supports these observations. A retrospective study of women with hyperandrogenic skin disorders treated with spironolactone for an average of 26 months found that 38 patients maintained benefits for an average of 33.7 months after stopping the medication. However, 20 patients experienced relapse, with symptoms returning after an average of 17.5 months . Although baseline differences between the two groups weren’t statistically significant, clinicians note that women with more severe hyperandrogenism - such as pronounced hirsutism - are more likely to relapse sooner, especially if underlying conditions like PCOS or insulin resistance are not addressed .
In rare cases, less than 1% of hirsutism patients develop virilization, which is a rapid and severe worsening of symptoms. This can indicate the presence of tumors and typically predicts a higher recurrence rate after discontinuing spironolactone.
Influence of Hormonal and Genetic Factors
Severe hirsutism often signals underlying androgen excess from ovarian or adrenal sources, such as PCOS, nonclassic congenital adrenal hyperplasia, or Cushing's syndrome. It may also result from heightened receptor sensitivity, both of which can accelerate regrowth after treatment ends . Without addressing these hormonal or genetic factors, regrowth is often more rapid and noticeable.
Genetics also play a role. Some women develop significant hirsutism even with relatively modest androgen levels due to increased androgen-receptor sensitivity and follicle responsiveness. Others with similar hormone levels may experience minimal hair growth. Women with genetically high follicular sensitivity are more likely to have severe hirsutism at the start and are at greater risk of recurrence, even if their hormone levels change only slightly after stopping treatment .
Effectiveness of Treatment Combinations
For women with severe hirsutism, combining spironolactone with estrogen-progestin contraceptives and metabolic interventions can offer better outcomes. This approach suppresses ovarian androgen production, reduces insulin-driven androgen increases, and enhances hair removal, providing more effective long-term control . Clinical experience suggests that women with moderate to severe hirsutism typically need 6–12 months to see maximum benefits and often require multi-year treatment to stabilize hair growth before tapering .
Specialists often recommend that women with severe hirsutism continue therapy for an extended period and taper off gradually while monitoring for early signs of regrowth. This sustained, combined treatment strategy is essential for delaying recurrence and maintaining results .
sbb-itb-6dba428
5. Your Hair Follicle Sensitivity and Genetics
How Sensitivity Affects Hirsutism Recurrence
The sensitivity of your hair follicles to androgens plays a major role in how quickly hirsutism can return after stopping spironolactone. This is especially true for those with idiopathic hirsutism, where the issue isn’t just about hormone levels. Spironolactone works by blocking androgen receptors, but it doesn’t alter the follicles' inherent sensitivity. So, when the medication is stopped, sensitive follicles may start responding to androgens again, leading to renewed hair growth.
Research Insights on Recurrence
A study involving 58 patients with hyperandrogenic disorders revealed some interesting patterns. About 35% of participants experienced a relapse, typically 17.5 months after stopping spironolactone. Meanwhile, 65% maintained the benefits for roughly 33.7 months. Interestingly, there was no notable difference in androgen levels between those who relapsed and those who didn’t, either at the start or end of treatment. This suggests that genetic factors and follicle sensitivity are likely more influential than hormone levels alone in determining whether hirsutism will return.
This understanding of genetic factors highlights the need for therapies that specifically address follicle sensitivity.
Hormonal and Genetic Influences
Genetics and hormones often work hand in hand when it comes to hirsutism. For example, genetic variations - like increased 5α-reductase activity in certain ethnic groups - can enhance the effects of androgens, even when levels are relatively low. Additionally, about half of women with PCOS produce excess adrenal androgens, such as DHEA-S, which further stimulate sensitive follicles. Insulin resistance can also play a role by reducing SHBG levels, which increases free androgens that target these sensitive hair follicles. Family history matters too; if your mother or sisters have dealt with hirsutism, you may be more prone to it due to inherited follicle sensitivity.
By addressing these genetic and hormonal factors, treatment plans can be tailored to improve long-term outcomes.
Benefits of Combination Treatments
For those with high follicle sensitivity, combining spironolactone with other medications can lead to better long-term results. Research shows that pairing spironolactone (100–200 mg/day) with either finasteride or low-dose cyproterone acetate can enhance effectiveness for up to 12 months after treatment. These combinations work by targeting multiple pathways - blocking androgen receptors and inhibiting the enzyme that converts testosterone to DHT. This multi-pronged approach is more effective at managing genetic sensitivity than spironolactone alone.
A Magic Pill for Acne, PCOS, Female Hair Loss, Hirsutism and HS
Oana Health Treatment Options
Oana Health offers telehealth solutions specifically designed to address androgen excess and insulin resistance. Licensed healthcare providers create personalized treatment plans based on your medical history, and all prescribed medications are delivered directly to your doorstep with free shipping across the United States.
One option involves oral spironolactone, while combination therapies tackle insulin resistance alongside androgen excess. For localized treatment, topical therapies deliver anti-androgen effects directly to the affected areas. Below is an overview of the available treatments, their benefits, and pricing:
| Treatment | Price | Key Benefits |
|---|---|---|
| Spironolactone | $14/month | Blocks testosterone receptors in hair follicles; affordable and effective; clinical studies show significant hair growth reduction in 23 out of 30 women within 3–5 months |
| Metformin & Spironolactone | $32/month | Combines anti-androgen properties with insulin-sensitizing effects; addresses both hormonal and metabolic factors; ideal for PCOS patients with insulin resistance |
| Topical Spironolactone | $43/month | Targets anti-androgen therapy directly to problem areas; minimizes systemic side effects like fatigue or reduced libido; great for facial hair management |
These treatments are tailored to your specific androgen levels, medical history, and genetic sensitivity, ensuring a customized approach to managing hirsutism.
Choosing the right treatment depends on your symptoms and needs. For mild hirsutism without metabolic concerns, oral spironolactone may suffice. Women with PCOS and insulin resistance often achieve better outcomes with the metformin combination, as it tackles the root cause of excess androgen production. If facial hair is your primary concern or if oral medications have caused side effects, topical spironolactone provides a targeted alternative.
Getting started is simple. Complete a quick five-minute online consultation to share your medical history. Once approved, you’ll benefit from ongoing support, automatic prescription refills, and treatments that address the underlying factors contributing to hirsutism.
Conclusion
The return of hirsutism after stopping spironolactone depends on several factors, including androgen levels, the length of treatment, use of combination therapies, the initial severity of symptoms, and how sensitive hair follicles are to androgens. Individual responses vary - some women maintain their progress for a longer time, while others may experience a quicker relapse of symptoms.
Although spironolactone effectively blocks the effects of androgens, it doesn’t tackle underlying causes like insulin resistance or excess adrenal androgens. Once the medication is discontinued, these root issues can resurface. Women with milder symptoms at the start, well-managed androgen levels, a longer treatment duration, and combination therapies are more likely to see lasting results. On the other hand, those with more severe PCOS, ongoing hyperandrogenism, or a strong family history of hirsutism are at a higher risk of symptom recurrence.
Achieving lasting results requires more than just medication - it calls for a well-rounded approach. Managing weight, improving insulin sensitivity, reducing stress, and balancing hormones are all key to long-term success. Personalized care, such as telehealth services, can play a vital role in monitoring androgen levels, metabolic health, and symptom patterns over time, ensuring treatments are adjusted as needed. Oana Health’s telehealth platform offers tailored prescriptions, nutrition guidance, weight management support, and ongoing monitoring. By addressing not only hirsutism but also related concerns like menstrual irregularities, acne, and mood changes, this service provides a comprehensive solution. With treatments delivered straight to your door, automatic refills, and virtual check-ins, you can maintain a consistent plan that tackles both the visible symptoms and the hormonal imbalances driving them. This integrated strategy underscores the importance of addressing both the symptoms and their root causes for sustainable results.
FAQs
How does spironolactone help reduce unwanted hair growth?
Spironolactone helps manage excessive hair growth, or hirsutism, by targeting androgen levels - hormones that play a role in this condition. It works by blocking androgen receptors and reducing the production of these hormones, gradually decreasing unwanted hair growth.
While many find this treatment helpful, its effectiveness can depend on individual factors such as hormone levels and the root cause of the condition.
How do genetics influence the return of hirsutism after stopping Spironolactone?
Genetics have a significant impact on whether hirsutism returns after stopping Spironolactone. Your genetic makeup affects hormone levels and hair growth patterns, which might make some people more prone to experiencing a resurgence.
Because genetics are something you can't change, some women may require continuous management or additional treatments to keep their results. Working with a healthcare provider can help develop a personalized, long-term plan that suits your specific needs.
Why are combination therapies better for managing hirsutism in the long term?
Combination therapies tend to work better for managing hirsutism over time because they tackle several aspects of the condition at once. By addressing both the hormonal imbalances that drive excessive hair growth and the hair growth itself, these approaches often deliver more lasting and effective results.
For instance, pairing medications that control androgen levels with topical treatments aimed at reducing hair growth can target the underlying causes while also improving the visible symptoms. This well-rounded strategy typically yields better results compared to relying on just one type of treatment.
.webp)



