GLP-1 Insurance Denials: What to Do
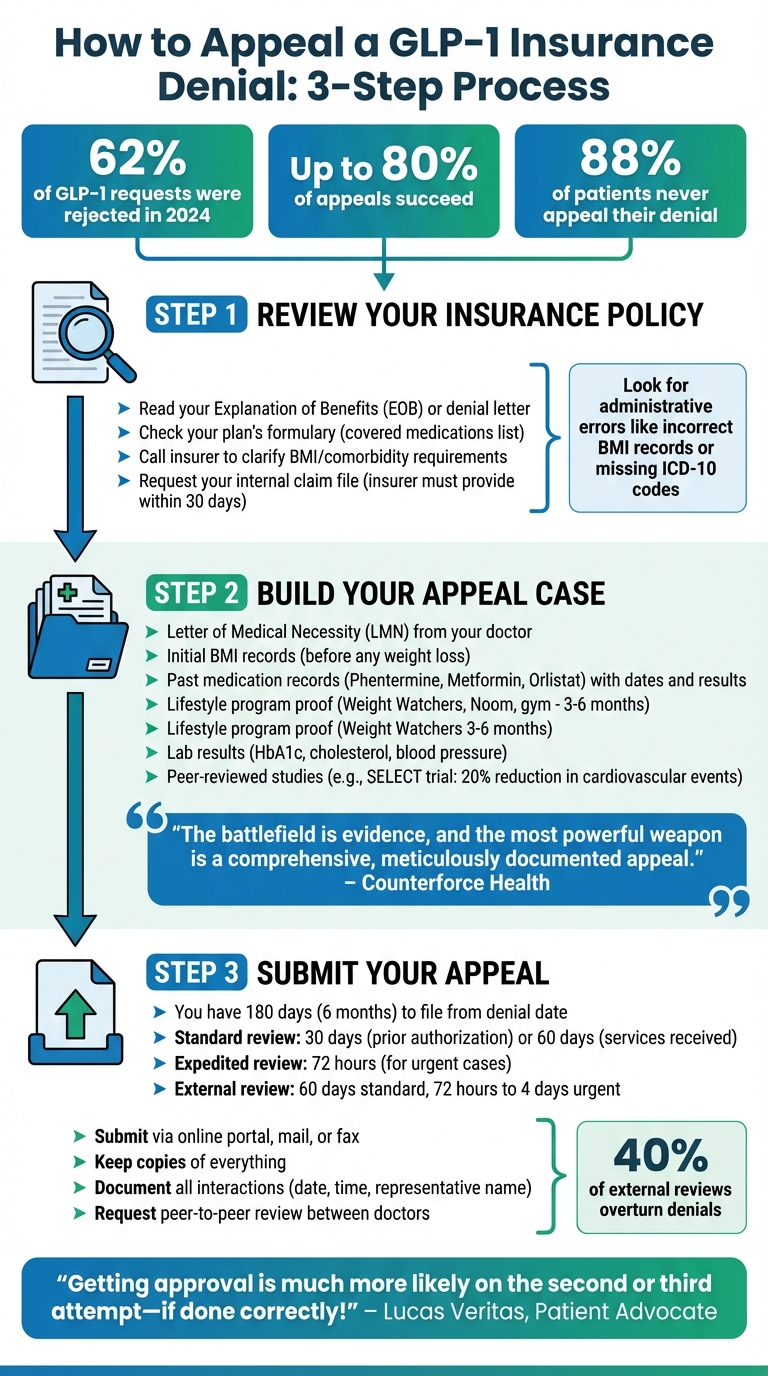
If your insurance denied coverage for GLP-1 medications like Ozempic or Wegovy, you’re not alone - 62% of requests were rejected in 2024. But here’s the good news: up to 80% of appeals succeed. This guide explains why denials happen and how you can appeal effectively.
Key Points:
- Common Denial Reasons: Off-label use (e.g., for weight loss), step therapy requirements, or insurers classifying treatments as non-essential.
- What You Can Do:
- Review your denial letter for specific reasons.
- Work with your doctor to create a Letter of Medical Necessity.
- Provide detailed records of past treatments and health conditions.
- File an appeal within 180 days and consider an external review if needed.
- Alternative Options: Explore compounding pharmacies, cash-pay programs, or oral GLP-1 medications like Rybelsus.
Insurance denials can feel overwhelming, but with persistence and the right approach, you can improve your chances of getting coverage - or find affordable alternatives.
What If My GLP-1 Appeal Is Still Denied? Next Steps and FAQs
How to Appeal a GLP-1 Insurance Denial
Step-by-Step Guide to Appealing GLP-1 Insurance Denials
Did you know that up to 80% of patients who appeal their insurance denial eventually succeed?. If you’ve been denied coverage for a GLP-1 medication, don’t lose hope. With the right approach, you can fight back effectively. Here’s how to get started.
Review Your Insurance Policy
The first step is understanding why your claim was denied. Carefully review your Explanation of Benefits (EOB) or denial letter. It will specify the reason, such as "not medically necessary", "plan exclusion", or a requirement for "step therapy". Knowing the exact reason will help you craft a targeted appeal.
Next, check your plan’s formulary - the list of medications your insurance covers. Some plans may cover GLP-1 medications like Ozempic for diabetes but exclude others like Wegovy or Zepbound for weight loss. If your medication isn’t on the list, you’ll need to request a "formulary exception" rather than filing a standard appeal.
It’s also worth calling your insurer directly to clarify whether weight management is covered, what the BMI or comorbidity requirements are, and whether you need to complete step therapy or a lifestyle program first. Be aware that some employers exclude weight-loss drug coverage entirely to cut costs. If this is the case, even a flawless appeal might not succeed.
You’re entitled to request your internal claim file from the insurer. They must provide this within 30 days, and it often reveals administrative errors or missing documentation - like incorrect BMI records or absent ICD-10 codes - that you can address in your appeal. Once you’ve gathered all the details, you’ll be ready to build a strong case.
Build Your Appeal Case
A successful appeal hinges on presenting a medical argument supported by evidence. The cornerstone of your case is a Letter of Medical Necessity (LMN) from your doctor. This letter should explain how your specific health conditions - such as your BMI, lab results, or comorbidities like high blood pressure or prediabetes - make the GLP-1 medication essential for your treatment.
"The battlefield is evidence, and the most powerful weapon is a comprehensive, meticulously documented appeal." – Counterforce Health
If your denial involves step therapy, include detailed records of past medications you’ve tried, such as Phentermine, Metformin, or Orlistat. Document the dates, side effects, and lack of results for each. If lifestyle changes were required, provide proof of participation in programs like Weight Watchers, Noom, or gym memberships over the last 3–6 months.
Make sure to include your initial BMI if you’ve lost weight during treatment. Insurers sometimes deny claims if your current BMI doesn’t meet their criteria, even if you qualified when you started. Add lab results showing HbA1c levels, cholesterol, or blood pressure to highlight the health risks tied to obesity.
Cite peer-reviewed studies to strengthen your case. For example, the SELECT trial demonstrated that semaglutide reduced major cardiovascular events by 20% in overweight patients. This shifts the narrative from "weight loss" to "medical necessity."
Submit Your Appeal
You typically have 180 days (six months) from the denial date to file an appeal. Submit your appeal through your insurer’s online portal, by mail, or via fax, and keep copies of everything for your records.
If your health could be at risk due to delays, request an expedited review. Insurers are legally required to respond within 72 hours for urgent cases. For standard appeals, the timeline is 30 days for prior authorization requests and 60 days for services already received.
| Appeal Type | Decision Timeline (Standard) | Decision Timeline (Urgent) |
|---|---|---|
| Prior Authorization (Pre-service) | Within 30 days | Within 72 hours |
| Medical Services Already Received | Within 60 days | N/A |
| External Review | Within 60 days | 72 hours to 4 business days |
If your internal appeal is denied, you can request an external review by an independent third party. Nearly 40% of external reviews overturn insurance denials. Under the Affordable Care Act, insurers must honor the external reviewer’s decision if it’s in your favor.
"Getting approval for expensive GLP-1 medications is much more likely on the second or third attempt - if done correctly!" – Lucas Veritas, Patient Advocate
Throughout the process, keep a detailed record of every interaction. Note the date, time, and name of each representative you speak with. If possible, ask your doctor to arrange a peer-to-peer review with the insurance company’s medical director. These direct conversations can sometimes be more persuasive than written appeals.
Other Ways to Access GLP-1 Treatments
If your insurance appeals don’t work out, there are still alternative ways to access GLP-1 treatments. Options like compounding pharmacies, cash-pay programs, and oral medications provide other paths to consider.
Compounding Pharmacies
Compounding pharmacies create customized medications using the active ingredients found in brand-name GLP-1 drugs like semaglutide and tirzepatide. These pharmacies became popular as a more affordable option when the cost of brand-name drugs skyrocketed or shortages occurred. For instance, compounded semaglutide typically costs between $99 and $350 per month, compared to the $900 to $1,500 monthly price tag for brand-name options like Ozempic and Wegovy.
That said, it’s important to note that compounded GLP-1 medications are not FDA-approved as finished products. By July 31, 2025, the FDA had received 605 reports of adverse events linked to compounded semaglutide and 545 reports for compounded tirzepatide. Many of these incidents involved dosing errors, especially when vials and syringes were used instead of pre-filled pens.
"Compounded drugs should only be used in patients whose medical needs cannot be met by an FDA-approved drug." – U.S. Food and Drug Administration
Compounded GLP-1 medications can often be accessed through telehealth services that work with state-licensed compounding pharmacies, which ship directly to patients. Some pharmacies even add ingredients like vitamin B12 or offer alternative forms like oral pills. However, these variations often lack robust clinical data to confirm their effectiveness and safety.
| Medication Type | Estimated Monthly Cost |
|---|---|
| Compounded Semaglutide | $99 – $350 |
| Compounded Tirzepatide | $199 – $399 |
| Brand-name Ozempic (Retail) | $900 – $1,200 |
| Brand-name Wegovy (Retail) | $1,300 – $1,500 |
If you choose this route, it’s critical to verify the source. Make sure your medication comes from a state-licensed pharmacy and is prescribed by a licensed healthcare provider. Be cautious of unusually low prices, missing prescription requirements, or packaging issues. Injectable GLP-1s must also be refrigerated - avoid any medication that arrives warm or without proper cooling. Additionally, the FDA warns against using semaglutide sodium or semaglutide acetate in compounded medications, as these differ from the approved drug ingredients.
"Just because it's cheaper doesn't mean it's better or safe. If it sounds too good to be true, it probably is." – Supriya Rao, MD, Obesity Physician
For those seeking other cost-saving options, cash-pay programs may provide another solution.
Cash-Pay Options and Discount Programs
Paying out of pocket can sometimes be a more practical approach. Several programs offer reduced costs for those willing to pay directly. Manufacturer copay cards, for example, can lower out-of-pocket expenses to as little as $25 per month for individuals with commercial insurance. Direct-to-consumer pharmacy models also provide transparent cash-pay pricing, often hundreds of dollars less than traditional retail rates. For instance, Zepbound vials through LillyDirect cost between $299 and $449 per month, while Wegovy via NovoCare Pharmacy is around $349 per month - significantly less than retail prices that can exceed $1,000.
If you’re uninsured or underinsured, Patient Assistance Programs (PAPs) might provide medications at no cost for eligible individuals. Nonprofit groups like the PAN Foundation and NeedyMeds also offer grants and resources for those struggling with high medication costs. Additionally, prescription discount services like GoodRx and SingleCare can help you save hundreds of dollars. For example, GoodRx offers an introductory price of $199 for the first two fills of Ozempic.
| Medication | Option Type | Estimated Monthly Cost |
|---|---|---|
| Zepbound (vials) | LillyDirect (Cash-Pay) | $299 – $449 |
| Wegovy (injection) | NovoCare Pharmacy (Cash-Pay) | $349 |
| Wegovy (pill) | NovoCare Pharmacy (Cash-Pay) | $299 |
| Ozempic | GoodRx (Introductory Price) | $199 (first 2 fills) |
| Ozempic | NovoCare Pharmacy (Cash-Pay) | $349 – $499 |
To ensure medication authenticity, use barcode scanning tools provided by manufacturers. Some companies have also partnered with organizations like Costco and WeightWatchers to offer exclusive lower prices to members.
Oral GLP-1 Medications
For those who prefer not to use injections, oral GLP-1 medications are another option, though they may not be as effective for significant weight loss. A commonly prescribed oral medication is Rybelsus (semaglutide), which is taken daily rather than weekly like injectable options. While oral versions are effective for managing blood sugar and weight, injectables are often seen as the stronger choice for substantial weight loss.
Rybelsus typically costs around $1,388 for a 30-day supply, but discount coupons can reduce the price to about $875. Many insurance plans require "step therapy", meaning patients must first try oral medications like Rybelsus or metformin before qualifying for injectable treatments like Ozempic. For those denied GLP-1 coverage altogether, other oral alternatives like Qsymia and Contrave may be worth exploring.
| Feature | Oral GLP-1 (e.g., Rybelsus) | Injectable GLP-1 (e.g., Wegovy) |
|---|---|---|
| Dosing Schedule | Daily pill | Once-weekly injection |
| Typical Cost (with coupon) | ~$875 | ~$825–$1,225 |
| Primary Use | Often used as "step therapy" | Preferred for significant weight loss |
| Storage | Room temperature | Requires refrigeration |
Some compounding pharmacies have started offering GLP-1 medications in pill form. However, these compounded versions haven’t undergone rigorous clinical testing to confirm their absorption or safety. Additionally, oral medications like Rybelsus must be taken on an empty stomach with a small amount of water to ensure proper absorption.
"Compounded versions in pill form or mixed with other ingredients haven't undergone rigorous trials. Mixing active compounds without clinical data raises concerns about absorption, bioavailability, and patient safety." – Supriya Rao, MD, Obesity Physician
These options provide various ways to access GLP-1 treatments, offering flexibility for different budgets and preferences.
sbb-itb-6dba428
How Oana Health Can Help with GLP-1 Access

Oana Health simplifies the process of accessing GLP-1 treatments for managing PCOS and weight-related conditions through its telehealth platform. By combining personalized medical care with straightforward pricing, the platform removes many of the typical barriers patients face.
Personalized Telehealth Care
Oana Health offers treatment plans backed by science, developed by licensed experts in metabolic and hormonal health. These plans focus on addressing insulin resistance and hormonal imbalances, which are often key factors in the need for GLP-1 treatments. This targeted approach is particularly helpful for patients whose insurance claims are denied as “not medically necessary,” a frequent tactic used to avoid covering expensive treatments.
Through virtual consultations, patients can connect with healthcare providers without the inconvenience of in-person visits or the delays caused by prior authorization requirements. The goal is to bypass the usual insurance hurdles, making it easier for patients to access the care they need.
Affordable and Convenient Options
Oana Health also prioritizes affordability. With direct cash-pay pricing, patients can avoid the complications of insurance altogether. For instance, their Oral GLP-1 & Metformin combination starts at $199 per month, including free medication delivery to your home, which helps keep costs down.
This direct-to-consumer pricing model is comparable to manufacturer programs that have reduced costs to $349–$499 per month. It’s an accessible option for those who’ve run out of insurance coverage or want to skip the appeals process entirely.
Additional Treatment Options
Oana Health extends its care beyond GLP-1 medications, offering treatments for conditions linked to PCOS and metabolic health. These include:
- Oral Metformin ER: $22/month
- Spironolactone: $14/month
- Bupropion XL: $25/month
- Oral Minoxidil: $25/month
- Eflornithine 12%: $69/month
This broader approach acknowledges that managing PCOS and weight involves tackling multiple interconnected issues. By addressing insulin resistance, hormonal imbalances, and related symptoms simultaneously, Oana Health offers a more comprehensive solution. This is especially important given that fewer than 20% of employer health plans are expected to cover GLP-1 medications for weight loss by 2025.
Conclusion
A denial for GLP-1 medication coverage doesn’t have to be the end of the road. Consider this: while 60% of insurance appeals for GLP-1 drugs are successful, a staggering 88% of patients never challenge their denial. This means countless individuals may be missing out on beneficial treatments simply because they stopped after the first rejection.
To improve your chances, collaborate with your doctor to secure a Letter of Medical Necessity, compile records of past weight-loss efforts, and gather supporting documentation. If your internal appeal is denied, you still have options - requesting an independent external review within 120 days could overturn the decision, with success rates around 40%.
If appeals don’t pan out or you’re exploring other routes, there are alternative solutions to consider. Compounding pharmacies and manufacturer savings programs can help cut costs by $300 to $650 per month. Additionally, generic options like liraglutide or oral GLP-1 medications offer more budget-friendly choices without sacrificing effectiveness.
Telehealth services can also be a game-changer. For example, Oana Health provides a streamlined approach with transparent pricing starting at $199 per month for oral GLP-1 and Metformin combinations, including free home delivery. Their platform connects you with licensed providers who focus on comprehensive metabolic health, ensuring you find treatments that align with both your medical needs and budget.
FAQs
Why do insurance companies deny coverage for GLP-1 medications?
Insurance denials for GLP-1 medications can happen for a variety of reasons. Often, insurers require patients to meet specific BMI or clinical guidelines, and if those criteria aren’t met, coverage may be denied. Another common issue is incomplete paperwork - missing ICD-10 codes or a lack of supporting medical records can result in a rejection. In some cases, insurers enforce step-therapy rules, meaning you may need to try less expensive medications before they’ll approve GLP-1 treatment. On top of that, insurers sometimes categorize these medications as weight-loss drugs and deem them “not medically necessary.”
If you’ve been denied, don’t lose hope. Start by reviewing your insurer’s policy to understand their requirements. Make sure all necessary documentation is in order, and consider filing an appeal. You can also discuss alternative treatment options with your healthcare provider to find an approach that works best for you.
What steps can I take to appeal an insurance denial for GLP-1 medications?
To build a strong appeal, start by gathering all relevant medical records - this should include your BMI, diagnosis, lab results, and precise ICD-10 codes. Ask your doctor for a detailed letter of medical necessity that clearly explains why the prescribed medication is essential for your treatment. Be sure to directly address the insurer’s reason for denial, such as stating the treatment is "not medically necessary", and provide supporting evidence to challenge their decision. Also, double-check your insurance policy to ensure you submit your appeal within the required timeframe.
If you need extra guidance, consider reaching out to a healthcare provider who specializes in weight management and personalized care. For instance, Oana Health offers prescription-based solutions tailored to weight loss, insulin resistance, and related conditions. Their licensed professionals provide science-backed treatment plans and ongoing support to help you at every step.
What can I do if my insurance won’t cover my GLP-1 medication?
If your insurance doesn’t cover your GLP-1 medication, don’t worry - there are several ways to manage the cost. Start by checking out manufacturer savings programs or patient-assistance programs, which can help lower your expenses. You might also explore discount cards or look into more affordable generic alternatives. Some pharmacies or services may even offer competitive pricing if you decide to pay out-of-pocket.
Another option is telehealth services, such as Oana Health. These platforms connect you with licensed professionals who can prescribe personalized, science-based treatments. Plus, the medication is delivered straight to your door, making it a convenient and cost-conscious solution.
