HOMA-IR Score Checklist for Women with PCOS
For women managing PCOS, understanding your insulin resistance is key. The HOMA-IR test measures this by analyzing fasting glucose and insulin levels, offering insights into your metabolic health. With 35%-80% of women with PCOS facing insulin resistance - and over half at risk of developing type 2 diabetes by age 40 - this test helps shape effective treatment plans.
Here's what you need to know:
-
What is HOMA-IR?
A formula calculates insulin resistance:
HOMA-IR = (Fasting Glucose × Fasting Insulin) / 22.5
Results:- Below 1.0: Optimal sensitivity
- 1.0 to 2.5: Normal sensitivity
- Above 2.5: Possible insulin resistance
-
Why it matters:
Insulin resistance worsens PCOS symptoms (irregular periods, weight gain, acne) and increases risks of diabetes, heart disease, and other conditions. -
How to prepare for the test:
- Fast for 8–12 hours (water only).
- Avoid intense exercise 24 hours before.
- Inform your doctor about medications or supplements.
-
Treatment options:
- Lifestyle changes: Balanced diet, exercise (150 minutes/week), stress management.
- Medications: Metformin, GLP-1s, or topical alternatives.
- Supplements: Inositol, cinnamon, or berberine (consult your doctor).
Telehealth services like Oana Health offer accessible PCOS care, providing personalized plans, medications, and ongoing monitoring.
Regular HOMA-IR testing helps track progress and adjust treatments, empowering you to manage PCOS effectively.
What is HOMA-IR and How Does it Relate to PCOS
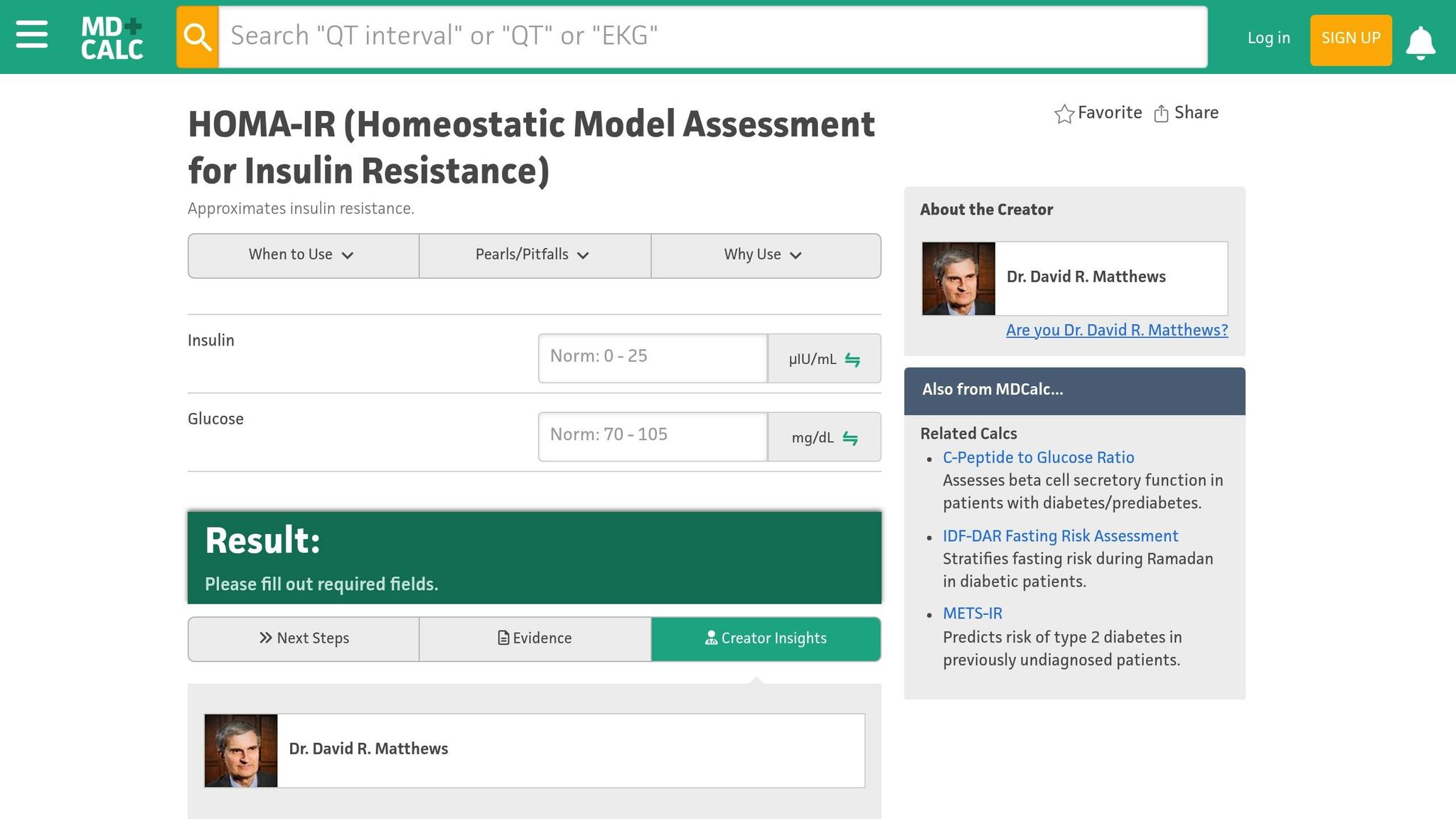
HOMA-IR Test Explained
HOMA-IR stands for Homeostatic Model Assessment of Insulin Resistance. It’s a method used to assess the balance between fasting blood glucose and fasting insulin levels. The formula for calculating HOMA-IR is:
HOMA-IR = (Fasting Glucose × Fasting Insulin) / 22.5.
The test itself is simple. You’ll need to fast for 8–12 hours before a single blood draw. No medications are involved, and in some cases, samples can even be collected at home.
Your HOMA-IR score helps measure how sensitive your body is to insulin. A higher score points to greater insulin resistance. While a score above 2.5 is often used as a marker for insulin resistance, the exact threshold can vary depending on individual factors. Here’s a quick breakdown:
| HOMA-IR Value | Interpretation |
|---|---|
| Below 1.0 | Optimal insulin sensitivity |
| 1.0 to 2.5 | Normal sensitivity |
| Above 2.5 | Indicates possible insulin resistance |
This test provides a foundational understanding of insulin resistance, which is a key issue in polycystic ovary syndrome (PCOS).
Why Women with PCOS Often Have Insulin Resistance
There’s a strong link between PCOS and insulin resistance. Studies show that about 85% of women with PCOS experience some degree of insulin resistance. This issue is highly prevalent in both obese and lean women with PCOS, affecting 70–95% of women with obesity-related PCOS and 30–75% of those with lean PCOS.
High insulin levels disrupt ovulation and cause the body to produce excess testosterone, which worsens PCOS symptoms. What’s notable is that insulin resistance can occur regardless of body weight.
The effects of insulin resistance go beyond PCOS symptoms. It increases the risk of conditions such as type 2 diabetes, gestational diabetes, heart disease, high blood pressure, abnormal cholesterol levels, sleep apnea, and stroke. Additionally, PCOS is associated with higher rates of depression and anxiety.
Understanding this connection highlights the importance of using HOMA-IR scores to guide treatment plans.
How HOMA-IR Results Guide PCOS Treatment
Your HOMA-IR score plays a critical role in shaping a personalized treatment strategy for PCOS and can help detect risks early. Research indicates that up to 70% of women with PCOS are insulin resistant, with around 10% already diagnosed with diabetes. Even women with normal glucose metabolism may see a 25% shift to abnormal levels within three years.
HOMA-IR scores are often used when deciding on treatments like metformin, especially in fertility protocols. For instance, women with a HOMA-IR score of 2.71 or higher may benefit from metformin before undergoing frozen IVF or ICSI-ET cycles, as this can improve clinical pregnancy rates. This targeted approach ensures that treatment aligns with your specific metabolic needs.
Addressing insulin resistance based on HOMA-IR results can lower both insulin and androgen levels, improve ovulation, reduce the risk of diabetes, and alleviate symptoms of metabolic syndrome. Depending on your score, your healthcare provider may recommend lifestyle changes, medications, or a combination of both. Even small steps, like losing 5% of body weight, can significantly reduce hyperandrogenism and improve insulin sensitivity. In fact, lifestyle interventions often outperform metformin alone in preventing diabetes progression.
Insulin & HOMA-IR Test Results Explained...Do You Have a Good Insulin Level or Insulin Resistance?
Pre-Test Preparation Checklist
To get reliable HOMA-IR test results, it's important to prepare properly. Following these steps will help ensure the test accurately reflects your insulin resistance and aids in managing your PCOS effectively.
Fast for 8-12 Hours Before Testing
Fasting for 8–12 hours is essential to obtain accurate HOMA-IR results. This allows your body to reach baseline insulin and glucose levels without interference from recent meals.
"Fasting for insulin test is essential because food intake stimulates insulin production. To obtain accurate baseline insulin levels, you must avoid eating or drinking anything except water for 8–12 hours before the test." - Lupindiagnostics.com
During this fasting period, you should only drink water. Avoid all food and beverages, including sugary drinks, coffee, tea, and alcohol, as any caloric intake can trigger insulin production and skew the results.
Stay hydrated by drinking water, as this can make the blood draw easier. It’s best to schedule your test early in the morning.
Avoid intense exercise for 24 hours prior to testing, as physical activity can temporarily alter blood glucose and insulin levels.
Lastly, be sure to inform your doctor about any medications or supplements you’re taking.
Tell Your Doctor About All Medications and Supplements
Certain medications and supplements can impact your glucose or insulin levels, potentially affecting your test results. Provide your doctor with a complete list of everything you’re taking.
Include prescription drugs, over-the-counter medications, vitamins, herbal supplements, and even birth control pills. This helps your healthcare provider account for how these may influence your results.
Do not stop taking prescribed medications without consulting your doctor. If you’re on diabetes medications like metformin, your doctor may give you specific instructions about dosage or timing before the test.
Finally, organizing your personal health details can help your doctor better interpret your results.
Gather Your Health Information
Providing your doctor with accurate background information enhances their ability to interpret your HOMA-IR score and tailor your PCOS management plan. Prepare the following:
- Track your menstrual cycle: Note the length, start date, and any irregularities.
- Record your symptoms: Include weight changes, hair growth patterns, acne, mood shifts, energy levels, and sleep quality.
- Compile your medical history: Include previous diabetes or glucose tests, family history of diabetes or PCOS, past pregnancies (including gestational diabetes), hormone test results, and prior HOMA-IR scores for comparison.
- List your current treatments: Document any PCOS medications, birth control methods, dietary changes, exercise routines, or other treatments.
Having this information ready ensures a productive discussion with your doctor, enabling them to create a treatment plan that aligns with your specific needs.
How to Read Your HOMA-IR Test Results
Understanding your HOMA-IR test results is key to managing PCOS effectively. These numbers reveal how your body handles insulin and help guide your treatment plan. Let’s dive into what your HOMA-IR score means.
Normal vs. High HOMA-IR Scores
There’s no universal "normal" HOMA-IR score - it can vary based on factors like age, ethnicity, and specific population groups. Typically, thresholds range between 2.1 and 3.8, but these numbers aren’t set in stone. Researchers caution against using fixed cut-offs without considering population-specific data or individual characteristics, as this can lead to inaccurate conclusions.
If your HOMA-IR score is above the threshold defined by your doctor, it suggests reduced insulin sensitivity. While this doesn’t necessarily mean you have diabetes, it does indicate a higher risk of developing it.
What Can Affect Your HOMA-IR Score
Several factors can influence your HOMA-IR results, making them higher or lower than expected. Here are some key contributors:
- Chronic Stress: Stress increases cortisol levels, which can interfere with insulin function. For instance, a study involving 766 workers in Beijing found that chronic stress was linked to higher HOMA-IR scores.
- Medications: Certain drugs, such as steroids, some blood pressure medications, and HIV treatments, can impact insulin sensitivity.
- Recent Illness or Infection: Being sick can temporarily alter your insulin response. Your doctor might suggest retesting after recovery.
- Personal Factors: Body weight, BMI, age, ethnicity, and even the specific type of PCOS you have can all influence your insulin sensitivity.
Treatment Options Based on Your Results
Your HOMA-IR score plays a crucial role in shaping your PCOS treatment plan. The main goals are to improve insulin sensitivity, reduce androgen levels, delay or prevent diabetes, and address other PCOS symptoms.
If your results indicate insulin resistance, lifestyle changes are often the first step. Research shows that dietary adjustments - like adopting a calorie-restricted or Mediterranean-style eating plan - combined with regular exercise (at least 150 minutes of aerobic activity per week) can significantly reduce the risk of diabetes progression. Managing stress through practices like yoga, meditation, or other relaxation techniques can also help lower cortisol levels.
In some cases, medication may be necessary. Metformin is a common choice for enhancing insulin sensitivity in PCOS patients. Additionally, some doctors may recommend thiazolidinediones, which can improve insulin resistance and address lipid imbalances in specific scenarios.
Ongoing monitoring is vital for managing PCOS effectively. Your doctor will likely track your glucose levels, blood pressure, and cholesterol to identify any changes early and adjust your treatment plan accordingly. Insulin resistance is common in PCOS, but its severity varies from person to person. Your HOMA-IR score serves as a valuable baseline for tracking progress and tailoring your care.
sbb-itb-6dba428
Questions to Ask Your Doctor About Your Results
Your HOMA-IR results are just the beginning. To get the most out of your appointment and create an effective plan for managing PCOS, come prepared with focused questions about your insulin sensitivity and overall health.
Important Questions About Your Score
Start by asking your doctor to break down what your HOMA-IR score means for you. Since this test measures insulin resistance, understanding your specific result is key. For instance, you might ask, "What does my HOMA-IR score reveal about my insulin sensitivity and metabolic health?"
Your doctor should explain that a higher score points to greater insulin resistance. It’s also helpful to ask how your score compares to normal ranges referenced earlier.
Be sure to discuss what might have influenced your score. Factors like age, lifestyle, diet, stress, medications, and even underlying health conditions can all play a role. For example, you could ask, "Could my current medications or recent stress levels have impacted my results?"
If your results were affected by temporary factors - like illness, stress, or medication changes - it’s worth asking whether retesting is necessary. Your doctor might recommend waiting until these factors stabilize before testing again, especially since certain medications can increase insulin resistance.
Don’t forget to touch on your cardiovascular health. Research shows that a 1-unit increase in (log)HOMA-IR is linked to a higher risk of cardiovascular disease, with odds ratios of 1.31 at baseline and 1.56 during follow-up. Understanding this connection can help you see the bigger picture of how insulin resistance affects more than just PCOS symptoms.
Creating Your Personal Treatment Plan
Once you’ve discussed your score, work with your doctor to create a treatment plan tailored to your needs.
Start by asking about weight management. Even losing 10–15 pounds can improve PCOS symptoms. Your doctor can help you set realistic goals and determine whether weight loss should be a focus for you.
Ask for personalized dietary advice. For example, you could inquire about adding more low glycemic index foods to your meals to regulate blood sugar. Fiber-rich foods might also help stabilize glucose levels. If needed, your doctor may suggest working with a nutritionist who specializes in PCOS and insulin resistance.
Discuss exercise options that fit your lifestyle. A common recommendation is at least 150 minutes of moderate-intensity exercise per week, combining cardio with strength training. Ask your doctor what type of physical activity would be most effective for you.
Medications might also be part of your plan. Ask if metformin, a medication often used to improve insulin sensitivity in PCOS patients, could be right for you.
You might also consider supplements. Certain options, like inositol, cinnamon, or berberine, have shown potential in supporting insulin sensitivity. Ask your doctor whether these supplements could be beneficial and how they might interact with other treatments.
Finally, establish a follow-up plan. Ask how often you should retest your HOMA-IR score and whether additional markers, like blood glucose or insulin levels, should be monitored. Regular check-ins can help you track progress and adjust your treatment plan as needed.
Telehealth Treatment Options for Insulin Resistance
Dealing with insulin resistance caused by PCOS can feel overwhelming, but telehealth services are making it easier than ever to manage your care from the comfort of home. With science-backed solutions, these platforms bring specialized treatment to your doorstep, saving time and simplifying the process.
How Oana Health Addresses Insulin Resistance
Oana Health focuses on providing telehealth services for women with PCOS and insulin resistance. Their licensed medical professionals design personalized treatment plans aimed at improving insulin sensitivity and managing PCOS symptoms. After reviewing your HOMA-IR results and medical history, Oana's doctors prescribe medications tailored to your needs.
They offer a variety of insulin sensitizer options to suit different preferences and budgets. For instance, Oral Metformin ER is available starting at $22 per month, while the Metformin & Spironolactone pack costs $32 monthly.
For those who can't tolerate oral metformin, Oana provides topical alternatives. Carrie S., a patient, shared her positive experience:
"I'm so glad I discovered Oana's metformin lotion! I used to struggle a lot with the side effects for oral metformin, and this is a great alternative for me. I get the same benefits but no more upset stomach and nausea, and this helps me stick with it a lot more consistently."
For more advanced cases of insulin resistance, Oana offers GLP-1 medications combined with metformin. Options like the Oral GLP-1 & Metformin pack and Oral Semaglutide GLP-1 are available for $199 monthly.
Victoria A., another patient, praised Oana's approach:
"Oana's telehealth service is fantastic! It's helped manage my insulin levels and reduce excess hair growth I was experiencing due to PCOS. I'm recommending this to all my friends with PCOS."
These treatments are easy to access through a streamlined telehealth process.
Convenient PCOS Care at Your Fingertips
Getting started with Oana is quick and hassle-free. In just 5 minutes, you can begin your treatment journey with an online consultation. During this step, you’ll share your health history and HOMA-IR results. For a $20 doctor visit fee, a licensed medical professional will review your information and create a personalized treatment plan.
Once approved, your medications are shipped directly to your door with free shipping - no pharmacy visits required. Oana partners with compounding pharmacies to ensure affordable, long-term care for PCOS patients.
The platform also offers savings plans for ongoing treatment. For example, topical metformin starts at $89 per month, while oral options begin at $22 monthly.
If you’re unsure where to start, Oana provides a PCOS quiz that matches you with treatment recommendations based on your symptoms and goals. Whether you’re looking to address insulin resistance, manage weight, reduce unwanted hair growth, or tackle multiple PCOS symptoms, this quiz helps guide you to the right therapy.
Regular online consultations allow for ongoing monitoring of your HOMA-IR scores and symptoms. With telehealth, you can access expert PCOS care no matter where you live or how busy your schedule is. This makes it easier to track your progress and adjust treatments as needed, ensuring your care stays on track over time.
Take Control of Your PCOS with Proper Testing
Once you've prepared for your test, understanding your HOMA-IR results becomes a crucial part of managing PCOS. Insulin resistance is a common issue for women with PCOS, affecting anywhere from 35% to 80% of those diagnosed. Knowing your HOMA-IR score can help you make better decisions about your health and treatment options.
To ensure accurate results, follow these guidelines: fast for 8–12 hours (water is fine), avoid intense exercise for 24 hours before the test, and let your healthcare provider know about any medications or supplements you’re taking, as these can impact your score.
Here’s how to interpret your HOMA-IR score:
- Below 1.0: Indicates optimal insulin sensitivity.
- 1.0 to 2.9: Suggests moderate insulin resistance.
- 3.0 or higher: Reflects significant insulin resistance.
These numbers aren’t just data - they’re a roadmap. Early detection of insulin resistance can lead to timely interventions, potentially reversing the condition.
If your score is high, it’s a signal to take action. Elevated HOMA-IR levels are linked to a higher risk of metabolic disorders. To improve insulin sensitivity, focus on a balanced diet, aim for at least 150 minutes of physical activity each week, prioritize sleep, and find ways to manage stress.
For ongoing support, telehealth options can make monitoring easier. Platforms like Oana Health connect you with licensed medical professionals who specialize in PCOS care. They can review your HOMA-IR results, tailor treatments to your needs, and even deliver medications directly to your door - free of shipping charges.
Regular follow-up tests are essential to track your progress. By seeing how your lifestyle changes and treatments impact your HOMA-IR score, you’ll gain motivation to stick with your health plan.
Managing PCOS effectively starts with reliable testing and a clear understanding of your results. Use this information to take meaningful steps toward better health.
FAQs
How does understanding my HOMA-IR score help me better manage PCOS symptoms?
Your HOMA-IR score is an important indicator of insulin resistance, which plays a significant role in managing PCOS symptoms. By knowing your score, you and your doctor can pinpoint the lifestyle adjustments and treatments needed to boost insulin sensitivity.
Improved insulin control can ease common PCOS symptoms such as weight gain, acne, and irregular periods, while also promoting better overall health in the long run.
What are the best lifestyle changes to boost insulin sensitivity for women with PCOS?
Improving how your body responds to insulin is a crucial step in managing PCOS, and small, steady changes in your daily habits can have a meaningful impact. Here are some practical strategies to consider:
- Choose a low glycemic index (GI) diet: Opt for whole, unprocessed foods like vegetables, lean proteins, and whole grains. These choices can help keep blood sugar levels stable and more manageable.
- Incorporate regular physical activity: Activities such as walking, strength training, or yoga can enhance insulin sensitivity while boosting overall well-being.
- Aim for a healthy weight: Losing even a small amount of weight can make a noticeable difference in reducing insulin resistance.
- Manage stress effectively: Techniques like mindfulness, deep breathing exercises, or meditation can help lower stress levels, which might also support better hormone balance.
- Prioritize quality sleep: Strive for 7 to 9 hours of restful sleep each night to promote healthier hormones and metabolism.
When paired with advice from your healthcare provider, these steps can help you take control of insulin resistance and ease PCOS symptoms. If you're feeling unsure about where to begin, a medical professional can help create a plan tailored to your needs.
What factors can affect my HOMA-IR score, and how can I manage them?
Several things can affect your HOMA-IR score, such as age, hormonal shifts (like those during your menstrual cycle), body composition, activity levels, diet, blood sugar, cholesterol levels (LDL, HDL, and triglycerides), inflammation, and even genetics.
To keep these factors in check, aim for lifestyle habits that support your health: eat a balanced diet, stay active, and regularly monitor your metabolic health. If you're uncertain about your results or need help addressing specific concerns, reach out to your doctor for tailored advice.
