How Pain Relievers Affect PCOS Medications
Managing PCOS often involves pain relievers for symptoms like cramps, headaches, and inflammation. However, certain painkillers can interfere with PCOS treatments such as metformin, hormonal contraceptives, and spironolactone. This can impact kidney function, blood sugar levels, and even ovulation. Here's what you need to know:
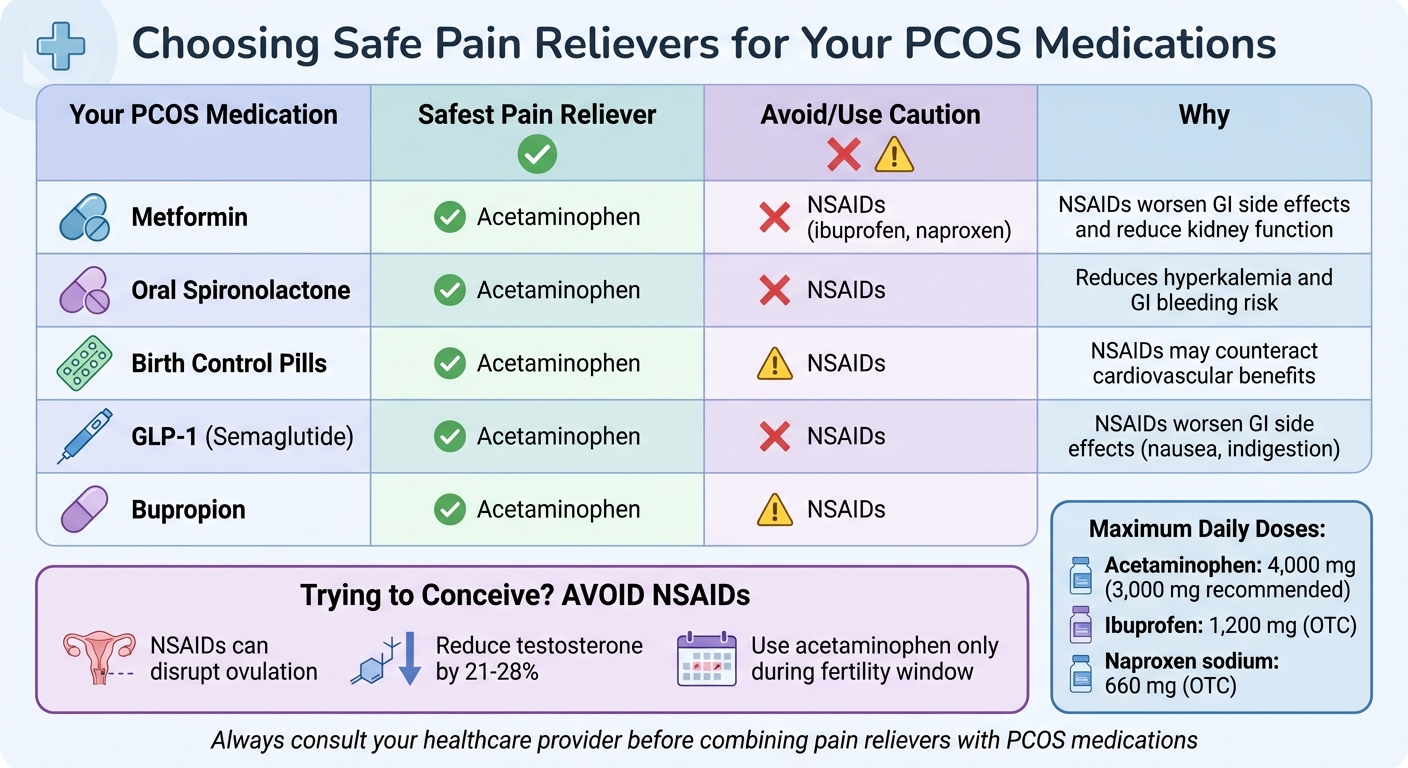
- Acetaminophen is generally the safest option for pain relief as it avoids kidney strain and doesn’t interfere with most PCOS medications.
- NSAIDs (like ibuprofen and naproxen) can reduce kidney function, worsen gastrointestinal side effects, and affect ovulation. Avoid them if you're trying to conceive.
- Low-dose aspirin can interact with NSAIDs, reducing its heart-health benefits and increasing bleeding risks.
Key Takeaway: Always choose pain relievers carefully based on your PCOS treatment plan. Consult your doctor if you’re unsure, especially during pregnancy or while managing additional health conditions.
Safe Pain Reliever Guide for PCOS Medications
How Pain Relievers Work in the Body
To understand how pain relievers might impact your PCOS treatment, it’s important to first know how these medications function in the body. Each type works through specific pathways, triggering different physiological effects. Let’s break down how these mechanisms work and their potential interactions with treatments.
NSAIDs: Ibuprofen, Naproxen, and High-Dose Aspirin
NSAIDs, such as ibuprofen and naproxen, target enzymes called COX-1 and COX-2. These enzymes play a role in converting arachidonic acid into compounds like prostaglandins, thromboxanes, and prostacyclins, which are responsible for signaling pain, causing inflammation, and regulating body temperature.
Both ibuprofen and naproxen are considered nonselective NSAIDs because they inhibit both COX-1 and COX-2. By reducing prostaglandins, they help decrease inflammation and make pain receptors less sensitive. For over-the-counter use, the daily limit for ibuprofen is 1,200 mg, while naproxen sodium should not exceed 660 mg per day.
Here’s the catch: COX-1 is crucial for maintaining the stomach lining and kidney function, while COX-2 is more active during inflammation. Blocking these enzymes can reduce blood flow to the kidneys, potentially leading to fluid retention or kidney issues. This is why NSAIDs should always be taken with food, milk, or antacids to protect your stomach.
It’s also essential to avoid using NSAIDs for more than three days if you have a fever or 10 days for pain without consulting a doctor. Combining different NSAIDs, like ibuprofen and naproxen, is a bad idea - it increases the risk of side effects.
How Acetaminophen Relieves Pain
Acetaminophen (commonly known as Tylenol) works differently. Instead of targeting inflammation, it changes how pain is perceived in the central nervous system and helps reduce fever. However, it doesn’t have much anti-inflammatory power because its COX-inhibiting effect is neutralized in inflamed tissues where peroxide levels are high. This makes acetaminophen gentler on the stomach and kidneys compared to NSAIDs.
The liver processes acetaminophen primarily through glucuronidation and sulfation. A smaller portion is metabolized via the CYP2E1 pathway, which produces a toxic byproduct called NAPQI. If NAPQI builds up - such as in cases of overdose - it can cause severe liver damage. To stay safe, don’t exceed the maximum daily dose of 4,000 mg.
Watch out for abbreviations like APAP or AC on medication labels, as these indicate the presence of acetaminophen in combination products like cold and flu remedies. If you drink three or more alcoholic beverages daily, it’s best to avoid regular use of acetaminophen to reduce the risk of liver damage.
Low-Dose Aspirin and Its Medical Uses
Low-dose aspirin (usually 81 mg) serves primarily as a blood thinner, not a pain reliever. It works by permanently inhibiting COX-1 in platelets, preventing them from clumping together to form clots. This mechanism is different from higher-dose aspirin (325–650 mg), which is used to manage pain, reduce fever, and treat inflammation.
Dr. Michael J. Blaha, Director of Clinical Research at Johns Hopkins Ciccarone Center, explains:
In low doses, aspirin inhibits platelets and therefore reduces blood clots. Aspirin can reduce heart attacks and strokes, and to some degree, other clots like those in the deep veins of the legs.
However, daily aspirin use isn’t without risks. Nearly 19 million Americans aged 60 and older take aspirin daily, with over 3 million doing so without medical advice. This is concerning because aspirin raises the risk of internal bleeding, particularly for people with a history of gastrointestinal issues or ulcers. The American Heart Association advises against self-prescribing daily aspirin for these reasons.
Low-dose aspirin is sometimes prescribed for specific conditions, such as during pregnancy or for cardiovascular health. It’s worth noting, though, that taking ibuprofen alongside aspirin can reduce the protective benefits of aspirin. These nuances are important when considering how pain relievers may interact with PCOS treatments.
How Pain Relievers Interact With PCOS Medications
Understanding how pain relievers interact with medications commonly prescribed for PCOS is essential for managing symptoms effectively. Below, we’ll explore how these interactions play out with insulin sensitizers, hormonal therapies, and other treatments.
Metformin and Other Insulin Sensitizers
When using pain relievers alongside metformin, kidney function plays a critical role. Metformin, often associated with gastrointestinal side effects like nausea and diarrhea, can increase the risk of severe GI issues. Research shows that compared to oral contraceptives, metformin significantly raises the odds of severe GI events, with rates climbing from 0.3% (for birth control pills) to as high as 4.5%. Since metformin is cleared entirely through the kidneys, any reduction in kidney function - such as that caused by NSAIDs, which block COX enzymes and reduce renal blood flow - can lead to drug buildup and, in rare cases, lactic acidosis.
Acetaminophen is often a better choice for pain relief in this scenario. It’s less likely to upset the stomach or impact kidney function. Angela Grassi, MS, RDN, LDN, from the PCOS Nutrition Center, advises:
Metformin should be taken with food to minimize side effects. Slowly increasing the dose of metformin over several weeks is recommended for best results.
If you’re managing your metformin treatment through Oana Health, their providers can guide you in choosing the safest pain reliever based on your kidney health and overall condition.
Birth Control Pills and Hormonal Contraceptives
Hormonal contraceptives, particularly those containing estrogen, increase prostacyclin production - a compound that helps prevent blood clots. On the other hand, NSAIDs inhibit COX-2, which reduces prostacyclin levels. The Public Library of Science explains:
Inhibition of COX-2 prevents production of prostacyclin, which has a role in preventing blood clotting. As estrogen acts to increase production of prostacyclin, it is possible that the effect of hormone replacement therapy on the heart is counteracted by these NSAIDs.
While NSAIDs don’t interfere with the contraceptive effectiveness of birth control pills, they may pose cardiovascular risks if you have clotting risk factors such as smoking or obesity. In such cases, acetaminophen is a safer alternative for pain relief. Aligning your choice of pain reliever with your hormonal therapy ensures that your PCOS treatment remains effective.
Spironolactone, Topical Spironolactone, and Eflornithine
Oral spironolactone can increase the risk of hyperkalemia, especially when combined with NSAIDs, which may also promote potassium retention. This combination raises the likelihood of hyperkalemia and gastrointestinal bleeding. Nicholas Moore from the Université de Bordeaux notes:
Aldosterone antagonists (eg, spironolactone) are associated with an increased risk of GI bleeding and possibly impaired healing of gastric or duodenal erosions. Thus, risk of GI bleeding in patients taking these agents may be further increased when NSAIDs are used concomitantly.
Topical spironolactone, however, is absorbed minimally into the bloodstream and poses little concern for interactions. If you’re using topical spironolactone from Oana Health for hair loss, occasional NSAID or acetaminophen use is generally safe. Similarly, eflornithine cream, used for reducing facial hair, does not significantly interact with pain relievers. For regular pain relief, acetaminophen remains the safest choice.
GLP-1 Medications and Weight Management Drugs
GLP-1 medications like semaglutide, available through Oana Health's weight loss program, often cause gastrointestinal side effects such as nausea and indigestion, especially during dose adjustments. NSAIDs can exacerbate these GI symptoms, making acetaminophen a better option for pain relief. While there’s no direct interaction that reduces the efficacy of either treatment, the combined GI discomfort could disrupt consistent medication use.
Taking acetaminophen with a small amount of food can help reduce stomach upset. For those using orlistat, a fat-absorption blocker, it’s best to separate the timing of orlistat and pain relievers by at least two hours, as orlistat may interfere with the absorption of fat-soluble vitamins.
Bupropion and Mental Health Medications
Bupropion, often prescribed for PCOS-related depression and weight management, has specific considerations when combined with pain relievers. NSAIDs can increase the risk of bleeding when used with certain antidepressants. While bupropion is not an SSRI, caution is advised if you’re taking multiple mental health medications or low-dose aspirin for heart health.
Acetaminophen is a safer alternative as it doesn’t affect bleeding risk and works well with bupropion. However, due to bupropion’s effect on the seizure threshold, it’s important to stick to recommended pain reliever doses and avoid combining multiple CNS-affecting medications.
sbb-itb-6dba428
Safe Pain Relief Strategies for PCOS Treatment
When managing PCOS, choosing the right pain reliever is crucial to ensure it complements your treatment plan without causing unwanted side effects. Here's how to make informed decisions.
Choosing Safe Pain Relievers for Your PCOS Medications
Acetaminophen is often the safest option for most individuals undergoing PCOS treatment. Unlike NSAIDs, it doesn't irritate the stomach and works well with medications like metformin, hormonal contraceptives, and mental health treatments. For those on metformin, acetaminophen is a reliable choice as it avoids worsening gastrointestinal discomfort or impacting kidney function.
If you're trying to conceive, steer clear of NSAIDs altogether. Studies indicate that a 3-week course of ibuprofen (400 mg, taken two to three times daily) can lower total testosterone by 21% and free testosterone by 28% in women with PCOS. While reduced testosterone might seem beneficial, NSAIDs can disrupt ovulation by interfering with the inflammatory processes necessary for egg release. During your fertility window, stick with acetaminophen as your go-to pain reliever.
| Your PCOS Medication | Safest Pain Reliever | Reason |
|---|---|---|
| Metformin | Acetaminophen | Doesn't worsen GI side effects or harm kidney function |
| Oral Spironolactone | Acetaminophen | Reduces risks of hyperkalemia and GI bleeding |
| Birth Control Pills | Acetaminophen | No cardiovascular interaction concerns |
| Bupropion | Acetaminophen | Avoids increased bleeding risk |
For those using topical spironolactone from Oana Health to treat hair loss, occasional NSAID use is generally fine. The topical form has minimal absorption into the bloodstream, making it a safer option.
When to Consult Your Doctor Before Taking Pain Relievers
Check with your doctor before taking NSAIDs if you have any of the following conditions: kidney disease, liver issues, unmanaged diabetes, high blood pressure, or if you require pain relief for more than 10 days or have a fever lasting over 3 days. These conditions heighten the risks of NSAID use, especially when combined with medications like metformin that depend on healthy kidney function.
If you're pregnant or planning to conceive, consult your healthcare provider immediately. NSAIDs are generally not recommended after 20 weeks of pregnancy due to potential risks to fetal kidney health and are strictly avoided after 30 weeks. Your doctor can guide you toward safer alternatives that align with both your pregnancy and PCOS management needs.
Additionally, those on blood pressure medications should exercise caution. NSAIDs can reduce the effectiveness of ACE inhibitors, ARBs, and diuretics, while also increasing the risk of kidney complications. Nicholas Moore from the Université de Bordeaux highlights the importance of careful NSAID use:
Health care providers can be instrumental in educating patients that using OTC NSAIDs at the lowest effective dose for the shortest required duration is vital to balancing efficacy and safety.
Monitoring Your Health While Using Pain Relievers
Pay attention to warning signs that could indicate serious issues. Seek immediate medical help if you experience black or tarry stools, vomit resembling coffee grounds, cloudy urine, difficulty urinating, or yellowing of the skin or eyes. These symptoms may signal gastrointestinal bleeding, kidney problems, or liver damage.
Keep a detailed list of all your medications, including PCOS treatments, over-the-counter pain relievers, vitamins, and supplements. Share this list with every healthcare provider you visit. Pharmacists can help identify potential interactions between prescriptions and OTC medications.
If you're on spironolactone, ask your doctor about regular monitoring of potassium and sodium levels, especially if you frequently use pain relievers. Elevated potassium levels can lead to heart rhythm issues, and combining spironolactone with NSAIDs increases this risk.
For those taking metformin, schedule routine tests to monitor kidney function, liver enzymes, and vitamin B12 levels. Metformin relies on healthy kidney function, and adding NSAIDs can put additional strain on your renal system. Leigh Ann Anderson, PharmD, from Drugs.com advises:
If you think you may be experiencing a symptom or side effect due to a drug interaction, contact your healthcare provider right away for advice.
Monitor your blood pressure at home if you're using NSAIDs alongside blood pressure medications. NSAIDs can cause slight but consistent increases in blood pressure and may reduce the effectiveness of your blood pressure treatments. This is especially important for women with PCOS, who already face an elevated risk of cardiovascular issues.
Conclusion
When managing PCOS, choosing the right pain reliever is an essential part of the process. For many women with PCOS, acetaminophen stands out as a safe option since it doesn’t interfere with common treatments like metformin, hormonal contraceptives, or spironolactone. For more comprehensive pain relief, acetaminophen can be paired with ibuprofen, as they are processed by different organs - acetaminophen by the liver and ibuprofen by the kidneys. As Stacia Woodcock, PharmD from GoodRx, explains:
Acetaminophen and ibuprofen work differently in the body. They are also cleared from the body by different organs. This makes it safe to take them together for additional pain relief if one alone doesn't do the trick.
However, it’s important to avoid NSAIDs like ibuprofen during your fertility window, as they may negatively impact ovulation by lowering testosterone levels and interfering with the body’s natural inflammatory pathways. Beata Banaszewska from the Division of Infertility and Reproductive Endocrinology advises:
Since the process of ovulation involves the activation of inflammatory pathways, the administration of nonsteroidal anti-inflammatory drugs should be avoided in women desiring ovulation.
Proper dosing is just as important as product selection. The maximum daily dose of acetaminophen for adults is 4,000 mg, though many manufacturers recommend staying below 3,000 mg for added safety. For ibuprofen, the daily limit is 1,200 mg.
Before combining any pain relievers with your PCOS medications, especially if you have liver or kidney issues, consult your healthcare provider. For tailored advice, consider speaking with a professional at Oana Health. Taking these precautions ensures your treatment plan remains effective while protecting your overall well-being.
FAQs
Can pain relievers like ibuprofen affect kidney health in people with PCOS?
Non-steroidal anti-inflammatory drugs (NSAIDs) - like ibuprofen, aspirin, and naproxen - work by blocking prostaglandins, which are substances that not only cause pain but also help maintain proper blood flow to the kidneys. When prostaglandins are suppressed, blood flow to the kidneys can drop, potentially causing temporary kidney function changes or, in some cases, kidney damage with prolonged or frequent use. This risk is especially concerning for individuals with conditions such as high blood pressure, diabetes, or pre-existing kidney issues.
For women with PCOS, the situation becomes even more complex. Factors like insulin resistance, obesity, or hypertension can already place added stress on the kidneys. Adding NSAIDs into the mix may further increase the risk of kidney-related problems. To minimize these risks, stick to the lowest effective dose for the shortest possible time, ensure you stay well-hydrated, and keep an eye on your kidney health through regular monitoring. If you're unsure about which pain relief options are safest for you, Oana Health’s telehealth clinicians can offer tailored advice based on your specific PCOS-related health concerns.
Why is acetaminophen often recommended over NSAIDs for managing PCOS-related pain?
Acetaminophen is often suggested for managing PCOS-related pain because it’s less likely to interfere with ovulation or disrupt hormone balance. This makes it a safer option for women undergoing PCOS treatments or trying to conceive. On the other hand, NSAIDs like ibuprofen or aspirin might affect ovulation and could lead to heavier bleeding.
If you're dealing with PCOS and exploring pain relief options, it’s important to consult your healthcare provider. They can help you choose a solution that fits your treatment plan and overall health needs.
Can I take pain relievers while managing PCOS and trying to get pregnant?
When managing PCOS and trying to conceive, it's important to choose pain relievers wisely. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, might interfere with ovulation if taken around that time, potentially making conception more challenging. A safer alternative for pain relief during this period is acetaminophen (Tylenol).
If you're unsure about which pain relievers are best or how they might interact with your PCOS treatments or fertility plans, consulting a healthcare provider is a smart move. For tailored advice, platforms like Oana Health focus on PCOS care and can provide recommendations that align with your specific needs.
