PCOS Hair Loss vs. Androgenic Alopecia
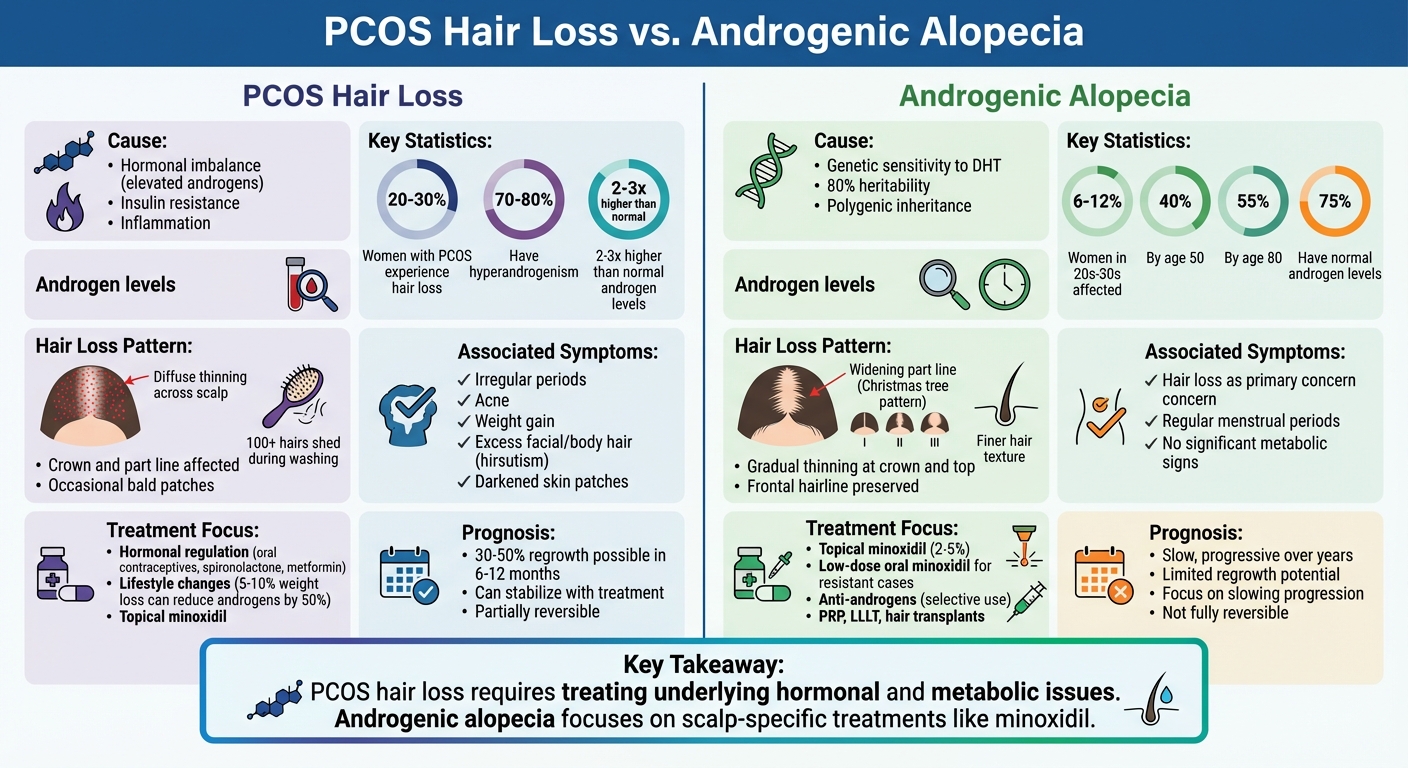
- PCOS Hair Loss: Caused by hormonal imbalances, like elevated androgens and insulin resistance. Often linked to irregular periods, acne, and weight changes. Hair thinning is diffuse, especially at the crown, and may come with excess body hair (hirsutism).
- Androgenic Alopecia: A genetic condition where hair follicles shrink due to sensitivity to DHT. Thinning is gradual, with a widening part line but no frontal hairline loss. Hormone levels are usually normal.
Key takeaway: PCOS-related hair loss requires treating underlying hormonal and metabolic issues, while androgenic alopecia focuses on scalp-specific treatments like minoxidil.
Quick Comparison:
| Factor | PCOS Hair Loss | Androgenic Alopecia |
|---|---|---|
| Cause | Hormonal imbalance (e.g., high DHT) | Genetic sensitivity to DHT |
| Symptoms | Diffuse thinning, irregular periods | Gradual thinning, widening part |
| Treatment Focus | Hormones + lifestyle + hair therapy | Scalp-specific treatments |
| Progression | Can stabilize with treatment | Slow, progressive over years |
Addressing hair loss starts with the right diagnosis. Keep reading for treatments and how to differentiate these conditions.
PCOS Hair Loss vs Androgenic Alopecia Comparison Chart
PCOS Facial Hair and Hair Loss | Causes, Treatments, & Natural Ways to Reduce Hirsutism & Hair Loss
What Is PCOS Hair Loss?
PCOS hair loss refers to hair thinning caused by the hormonal imbalance associated with polycystic ovary syndrome (PCOS). This condition is tied to elevated levels of androgens - hormones such as testosterone and DHT (dihydrotestosterone) - produced by the ovaries and, in some cases, the adrenal glands.
Causes of PCOS Hair Loss
The main culprit behind hair loss in PCOS is an excess of androgens. These hormones interfere with the natural hair cycle by shortening the growth phase (anagen) and prolonging the shedding phase (telogen), resulting in finer, more fragile hair that falls out more easily.
The connection between PCOS and hair loss is complex. Insulin resistance, a common feature of PCOS, boosts androgen production and contributes to chronic low-grade inflammation. This inflammation damages hair follicles, worsening thinning. Research shows that women with PCOS typically have 2–3 times higher androgen levels compared to those without the condition.
Genetics also play a role. Women with a genetic predisposition may have hair follicles that are particularly sensitive to even slight increases in androgens, making them more likely to experience hair loss.
Common Symptoms and Patterns
PCOS-related hair loss usually presents as diffuse thinning across the scalp, with noticeable changes at the crown and along the part line. Many women observe a wider part and a more visible scalp, giving the top of the head a "see-through" look. Increased hair shedding during brushing, washing, or showering is also common. In more severe cases, bald patches can develop.
A unique aspect of PCOS hair loss is its "mixed" nature. While scalp hair thins, other areas of the body may experience hirsutism - excessive hair growth on the face, chest, or abdomen - due to the way androgens affect different hair follicles. Additional symptoms often include acne, irregular menstrual cycles, weight gain, and difficulty losing weight. Studies indicate that 20–30% of women with PCOS experience hair thinning or loss, with hyperandrogenism present in 70–80% of cases.
This distinct thinning pattern makes PCOS hair loss different from typical androgenic alopecia.
What Is Androgenic Alopecia in Women?
Androgenic alopecia, also known as female pattern hair loss (FPHL), is a hereditary condition where hair follicles gradually shrink due to sensitivity to a hormone called DHT (dihydrotestosterone). Over time, this leads to thinner and shorter hair strands until hair growth eventually stops.
FPHL is the most common cause of hair loss in women. Research shows that around 6–12% of women in their 20s and 30s experience some level of hair thinning. By the age of 50, about 40% of women are affected, and this number can climb to 55% by the age of 80. Below, we’ll explore the genetic and biochemical factors behind this condition.
Causes and Risk Factors
The main cause of FPHL is linked to genetics, specifically polygenic inheritance, where multiple genes make hair follicles more sensitive to androgens. Family history plays a major role, with heritability estimated at around 80% in women who experience FPHL. This genetic predisposition causes affected follicles to convert testosterone into DHT through an enzyme called 5-alpha reductase. This process shortens the hair growth phase. Interestingly, about 75% of women with FPHL have normal androgen levels in their blood.
While FPHL can occur alongside conditions like PCOS (polycystic ovary syndrome), it is primarily a distinct genetic condition. Other contributing factors include aging - especially post-menopause, when estrogen levels drop - as well as iron deficiency, thyroid issues, and certain medications.
Symptoms and Patterns
FPHL typically results in gradual thinning hair across the crown and central scalp, often with a noticeable widening of the midline part. Unlike male pattern baldness, women usually retain their frontal hairline. Other signs include finer hair texture and increased scalp visibility.
To assess the severity of FPHL, dermatologists often use the Ludwig scale:
- Ludwig I: Slight widening of the part line.
- Ludwig II: More pronounced thinning around the crown.
- Ludwig III: Significant scalp exposure, though complete baldness is rare.
A closer examination with a dermoscope often reveals variations in hair shaft diameter - if more than 20% of the hair shafts in the mid-scalp vary in thickness, it supports a diagnosis of androgenic alopecia. These distinct patterns help differentiate FPHL from other types of hair loss, such as those related to PCOS.
Key Differences Between PCOS Hair Loss and Androgenic Alopecia
While both conditions can lead to hair thinning, PCOS hair loss stems from a broader hormonal imbalance, whereas androgenic alopecia is primarily a genetic condition affecting hair follicles. Recognizing these differences is crucial for accurate diagnosis and treatment.
Comparison Table
| Factor | PCOS Hair Loss | Androgenic Alopecia |
|---|---|---|
| Primary Cause | Hormonal imbalances from PCOS, including elevated androgens, insulin resistance, and inflammation | Genetic sensitivity of hair follicles to DHT, often with a family history |
| Hormonal Profile | High testosterone, elevated LH levels, insulin resistance; free androgen index 2–3 times higher than in isolated FPHL | Normal to slightly elevated androgens; heightened follicle sensitivity to DHT without broader metabolic issues |
| Hair Loss Pattern | Diffuse thinning over the crown, increased shedding (100+ hairs during washing), visible scalp, occasional bald patches | Gradual thinning at the crown and top, widening part line, and preserved frontal hairline (Christmas tree pattern) |
| Associated Symptoms | Irregular periods, acne, weight gain, excess facial/body hair, and darkened skin patches | Hair loss as the primary concern; regular periods and no significant metabolic signs |
| Progression | Rapid and widespread if untreated; can stabilize or improve with hormone management, with 30–50% regrowth possible in 6–12 months | Slow, patterned progression over years; limited regrowth potential, with treatments aimed at slowing further loss |
| Treatment Focus | Systemic treatments addressing hormone imbalances and metabolism (e.g., weight loss, insulin resistance, androgen control) combined with hair therapies | Topical treatments like minoxidil and anti-androgens to slow hair follicle miniaturization and encourage regrowth |
Understanding these distinctions is key to tailoring the right diagnostic and treatment strategies.
Why Differentiating Matters
Getting the correct diagnosis ensures you receive the most effective treatment for your condition. For PCOS-related hair loss, focusing solely on scalp treatments overlooks the hormonal and metabolic issues causing the problem. In fact, targeted PCOS therapies can improve hair regrowth by up to 40% compared to generic treatments.
On the other hand, if your hair loss is due to androgenic alopecia without PCOS, undergoing extensive hormonal testing or systemic treatments may be unnecessary and could delay effective scalp-specific therapies. Women with PCOS need a combination of systemic hormone management and hair treatments, while those with androgenic alopecia typically benefit from localized scalp therapies alone.
For women experiencing hair loss alongside symptoms like irregular periods, acne, or excess facial hair, it's important to explore the possibility of PCOS. Oana Health offers telehealth services tailored to PCOS and hormonal treatments, providing personalized care for hair loss, insulin resistance, and other symptoms - all from the comfort of your home. Properly distinguishing between these conditions sets the stage for precise diagnostic and treatment approaches, which will be covered in the next section.
sbb-itb-6dba428
Diagnosing PCOS Hair Loss vs. Androgenic Alopecia
Getting a clear diagnosis starts with a detailed medical history, a thorough physical exam, and specific lab tests. Doctors rely on these tools to tease apart the differences between hair loss caused by PCOS and androgenic alopecia. This method helps separate the broader effects of PCOS from the localized hair follicle changes seen in androgenic alopecia.
Medical History and Physical Exam
Your doctor will ask about key symptoms such as irregular menstrual cycles, sudden or gradual hair thinning, weight changes, acne, and unusual hair growth patterns. These are all common indicators of PCOS. Questions about family history - whether anyone else has PCOS or experienced baldness - are also part of the process. Women with PCOS often report irregular or missed periods, which can be a telling clue.
During the physical exam, the doctor will examine your scalp for specific patterns of hair loss. Hair thinning from PCOS tends to be more diffuse, affecting the crown area, while androgenic alopecia usually causes a widening part line but leaves the frontal hairline intact. The exam may also reveal other signs of PCOS, like acne, excess facial or body hair, and obesity - symptoms that are less likely in cases of purely genetic hair loss.
Laboratory Tests and Imaging
If PCOS is suspected, your doctor will likely order a hormone panel to measure testosterone levels, the free androgen index, and the LH/FSH ratio (which is often higher than 2:1 in PCOS). Tests for fasting glucose and insulin can help identify insulin resistance, while thyroid and iron level checks rule out other causes of hair loss. A pelvic ultrasound is another key diagnostic tool, as it can reveal polycystic ovaries - characterized by 12 or more small follicles per ovary or an ovarian volume over 10 mL.
On the other hand, diagnosing androgenic alopecia usually doesn’t require extensive hormonal testing or imaging unless there are signs of elevated androgens. In most cases, the diagnosis is based on the pattern of hair loss and family history.
If the initial findings are unclear, further evaluation by a specialist can provide more answers.
Specialist Referrals and Scalp Biopsy
When symptoms overlap or remain difficult to interpret, your doctor may refer you to a specialist. An endocrinologist or gynecologist can help with PCOS evaluation, while a dermatologist can offer a more detailed assessment of hair loss. In some cases, a scalp biopsy may be necessary. Though both PCOS-related hair loss and androgenic alopecia can show similar biopsy results - like an increase in fine, vellus hairs - the broader clinical picture usually clarifies the diagnosis.
For women dealing with hair loss combined with irregular periods or other PCOS symptoms, services like Oana Health offer convenient telehealth consultations. They provide hormone testing, imaging, and tailored treatment plans, all delivered to your home with free shipping.
Treatment Options for PCOS Hair Loss vs. Androgenic Alopecia
Once a diagnosis is confirmed, the treatment approach varies: PCOS hair loss calls for a broader hormonal and metabolic strategy, while androgenic alopecia focuses on localized follicle therapy. Knowing these distinctions helps you and your doctor create an effective plan.
PCOS Hair Loss Treatments
Treating hair loss associated with PCOS requires addressing both hormonal imbalances and hair follicle health. Elevated androgens and insulin resistance are key targets, alongside therapies that directly stimulate hair growth.
Oral contraceptives are commonly prescribed to reduce ovarian androgen production and increase sex hormone-binding globulin (SHBG), which binds excess testosterone. However, birth control pills alone usually yield modest results for hair loss, so they’re often paired with additional treatments.
Spironolactone, an anti-androgen, works by blocking androgen receptors in the scalp. Research shows it can reduce hair loss in 40–70% of women with elevated androgen levels, with visible improvements typically appearing within 3–6 months when used alongside other therapies. Metformin, known for improving insulin sensitivity, indirectly lowers androgen levels and is particularly beneficial for those with insulin resistance or prediabetes. For direct follicle stimulation, topical minoxidil (2–5% solution) has shown improvement in 60–80% of women within 6–12 months.
Lifestyle changes are a cornerstone of PCOS management. Losing just 5–10% of body weight can reduce androgen levels by up to 50% and improve hair density. Regular exercise - aiming for at least 150 minutes of moderate activity weekly - combined with a balanced diet, stress management (like yoga or mindfulness), and quality sleep can help restore hormonal balance. These steps not only support hair regrowth but are essential for managing PCOS overall. Services like Oana Health offer telehealth consultations and prescription treatments, including oral metformin ($22/month), spironolactone ($14/month), a metformin and spironolactone pack ($32/month), and oral minoxidil ($25/month), all delivered to your home with free shipping.
Next, let’s explore scalp-focused therapies for androgenic alopecia.
Androgenic Alopecia Treatments
For androgenic alopecia, treatments focus on stimulating and preserving hair follicles. The first-line option is topical minoxidil (2–5% solution), which extends the growth phase of hair and thickens the strands. If results are insufficient after 6–12 months, dermatologists may prescribe low-dose oral minoxidil as an off-label option for more resistant cases. For individuals with signs of androgen excess, spironolactone may also be added to counteract the effects of DHT on hair follicles.
Additional therapies, such as low-level laser therapy (LLLT), platelet-rich plasma (PRP) injections, or hair transplant surgery, may be considered for advanced cases. The primary goal is to slow follicle miniaturization and improve hair density over time, focusing less on systemic metabolic factors.
Comparison of Treatment Goals
| Aspect | PCOS Hair Loss | Androgenic Alopecia (without PCOS) |
|---|---|---|
| Primary Focus | Hormonal and metabolic regulation (insulin resistance, androgen excess) alongside follicle support | Follicle-specific therapies like minoxidil, PRP, LLLT, or transplants |
| Core Systemic Treatments | Oral contraceptives, spironolactone, metformin, lifestyle changes | Rarely systemic; anti-androgens used selectively |
| First-Line Hair Therapy | Topical minoxidil 2–5% | Topical minoxidil 2–5%; oral minoxidil for resistant cases |
| Treatment Goal | Balance hormones and metabolic health; hair improvement as part of broader PCOS care | Halt follicle miniaturization and boost density; less focus on systemic health |
| Reversibility | Partially reversible with early intervention targeting androgens and insulin resistance | Primarily aims to stop progression rather than achieve full regrowth |
The key difference lies in treatment priorities: PCOS hair loss calls for a comprehensive approach that addresses overall health, while androgenic alopecia focuses on preserving and stimulating existing follicles. Early treatment is crucial in both cases to slow progression and maintain hair density. While regrowth may be gradual, stabilizing hair loss is often the first and most achievable goal.
Conclusion
Understanding the difference between PCOS-related hair loss and androgenic alopecia is crucial for effective treatment. Hair loss caused by PCOS stems from hormonal imbalances - elevated androgens, insulin resistance, and inflammation - and is often accompanied by symptoms like irregular periods, acne, excess facial hair, and metabolic challenges. On the other hand, androgenic alopecia is a genetic condition where hair follicles are overly sensitive to androgens, even if hormone levels are normal. While both conditions result in thinning at the crown and a widening part, PCOS-related hair loss can often be addressed and improved with early intervention targeting hormonal and metabolic factors. In contrast, androgenic alopecia typically requires ongoing treatments focused on maintaining follicle health to slow progression.
An accurate diagnosis does more than guide hair restoration - it can also highlight broader health concerns, such as risks for cardiovascular disease, diabetes, and infertility. A comprehensive evaluation, including medical history, physical exams, hormone testing (androgens and insulin markers), and sometimes a scalp biopsy, ensures a personalized treatment plan rather than a generic approach. For PCOS, treatment often combines systemic therapies - like oral contraceptives, metformin, or spironolactone - with lifestyle adjustments and hair-specific solutions like minoxidil. For androgenic alopecia without PCOS, the focus shifts to direct follicle support through topical or oral minoxidil, anti-androgens when suitable, and advanced options like PRP therapy or low-level laser treatments.
Starting treatment early and staying consistent is essential since delayed action can lead to irreversible follicle damage, making regrowth more challenging.
Telehealth offers a convenient way to access tailored care for these conditions. Oana Health specializes in personalized telehealth services for PCOS-related hair loss and androgenic alopecia. With a simple online consultation, you can connect with licensed professionals who prescribe science-backed treatments. Options include oral minoxidil ($25/month), spironolactone ($14/month), oral metformin ($22/month), and combination packs like metformin and spironolactone ($32/month). Treatments are delivered directly to your home with free shipping, offering a seamless and comprehensive approach to managing both conditions from diagnosis to care.
FAQs
How can I tell if my hair loss is caused by PCOS or androgenic alopecia?
Distinguishing between PCOS-related hair loss and androgenic alopecia requires a closer look at their symptoms and causes. PCOS-related hair loss often comes with other signs of hormonal imbalance, such as irregular menstrual cycles, acne, weight fluctuations, and excess hair growth on the face or body. The hair thinning in this case is usually diffuse, affecting the scalp more evenly.
In contrast, androgenic alopecia, also known as female-pattern hair loss, typically shows up as gradual thinning around the crown and temples. Unlike PCOS, it doesn’t come with other hormonal symptoms. To pinpoint the exact cause, it’s best to consult a healthcare provider. They can perform hormonal tests and examine your scalp to identify the issue and suggest the right treatment.
What are the best treatments for hair loss caused by PCOS?
Managing hair loss caused by PCOS usually starts with tackling the hormonal imbalances at its root. Common treatments include topical metformin, which helps improve insulin sensitivity, and prescription options like Eflornithine, metformin-based lotions, and azelaic acid to reduce unwanted hair growth. These treatments are customized based on individual needs and must be prescribed by qualified healthcare professionals.
Since addressing PCOS-related hair loss often involves a mix of medical treatments and lifestyle changes, consulting a healthcare provider is essential to find the right plan for your unique situation.
Can hair lost from androgenic alopecia grow back completely?
While completely regrowing hair lost to androgenic alopecia isn’t achievable with today’s treatments, there are ways to manage the condition. For instance, minoxidil is a common medication that can help slow down hair loss and, in some cases, even encourage partial regrowth.
Acting quickly and sticking to a regular treatment routine can make a noticeable difference. However, for more advanced or permanent hair loss, procedures like hair transplants might be necessary to regain fullness.
