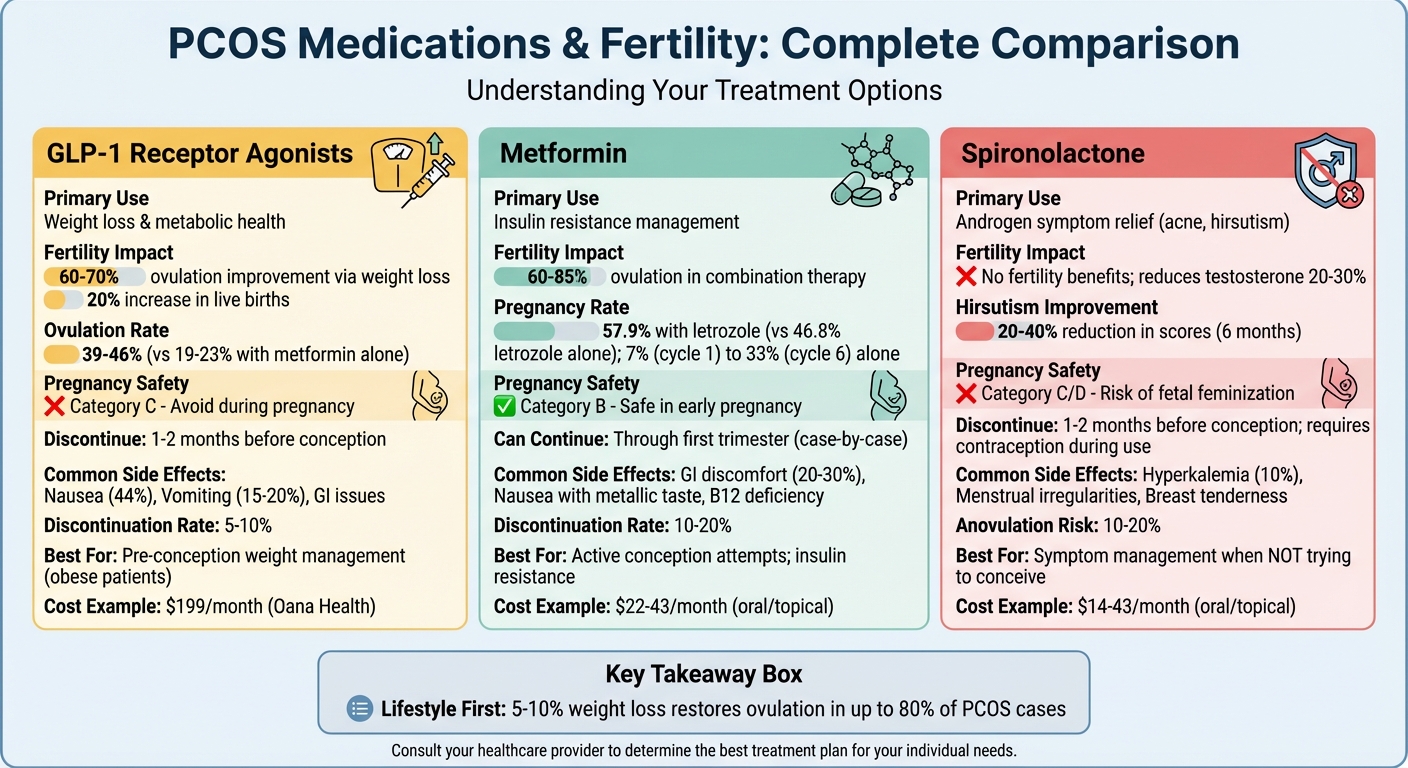
Polycystic Ovary Syndrome (PCOS) affects millions of women of reproductive age in the U.S., with fertility challenges being a common concern. Three medications often used to manage PCOS and its impact on fertility are GLP-1 receptor agonists, Metformin, and Spironolactone. Each serves a unique purpose:
- GLP-1 receptor agonists (e.g., semaglutide): Aid in weight loss, which may indirectly improve ovulation. Not safe for pregnancy and typically discontinued before conception.
- Metformin: Improves insulin resistance, supports ovulation, and is considered safe during early pregnancy. Often paired with fertility treatments for better results.
- Spironolactone: Reduces androgen-related symptoms like acne and hair growth but does not promote ovulation. Not recommended for those trying to conceive due to pregnancy risks.
Lifestyle changes remain the most impactful strategy, with a 5–10% weight loss restoring ovulation in up to 80% of cases. Below is a quick comparison of these medications.
Quick Comparison
| Medication | Fertility Impact | Pregnancy Use | Common Side Effects |
|---|---|---|---|
| GLP-1 Receptor Agonists | Supports ovulation via weight loss (60–70%) | Avoid during pregnancy | Nausea, vomiting, GI issues |
| Metformin | Boosts ovulation (60–85%) with combos | Safe in early pregnancy | GI discomfort, B12 deficiency |
| Spironolactone | No fertility benefits | Avoid during pregnancy | Menstrual irregularities, hyperkalemia |
Choosing the right treatment depends on your fertility goals and symptoms. For those trying to conceive, Metformin is often the best option, while GLP-1 receptor agonists are ideal for pre-conception weight management. Spironolactone is better suited for symptom relief when pregnancy isn't a priority.
PCOS Medications Comparison for Fertility: GLP-1, Metformin, and Spironolactone
1. GLP-1 Receptor Agonists
Mechanism of Action
GLP-1 receptor agonists, such as semaglutide, liraglutide, and tirzepatide, mimic the natural GLP-1 hormone. These medications work by slowing gastric emptying and increasing feelings of fullness, which can lead to a weight loss of 10–15%. For individuals with PCOS, these drugs help improve insulin secretion and reduce glucagon levels, addressing insulin resistance. This, in turn, can indirectly regulate androgen levels, restore menstrual cycles, and support ovulation. In the U.S., GLP-1 therapies are often prescribed through telehealth platforms like Oana Health, which focuses on weight management and PCOS care. Oana Health offers Dual Agonist GLP-1 Tablets for $199 per month.
Impact on Fertility
Although GLP-1 receptor agonists are not classified as fertility medications like letrozole or clomiphene, they can enhance fertility indirectly by improving metabolic health. Research indicates that these treatments can result in an average weight loss of 5–7 kg over 12–24 weeks, leading to better ovulation rates - 39–46% with exenatide compared to 19–23% with metformin. For women with obesity and anovulatory PCOS, significant weight loss has been linked to the return of regular menstrual cycles and, in some cases, spontaneous pregnancies. However, because these medications are not designed to directly induce ovulation, a "washout period" is typically recommended before attempting to conceive.
Safety and Pregnancy Considerations
Current data from animal studies and limited human research suggest that GLP-1 receptor agonists should not be used during pregnancy. Patients are generally advised to stop these medications 1–2 months before trying to conceive and to use reliable contraception while on treatment. For those undergoing assisted reproductive techniques, such as intrauterine insemination or in vitro fertilization, GLP-1 therapies are usually discontinued before ovarian stimulation to prevent any potential risks to the fetus. Healthcare providers often work closely with patients to transition from active weight-loss treatment to weight maintenance, sometimes in collaboration with telehealth services like Oana Health. Monitoring for safety and side effects is a key part of this process.
Side Effects
The most common side effects of GLP-1 receptor agonists include nausea, vomiting, diarrhea, constipation, and abdominal discomfort, especially during the initial dose escalation. Starting with a low dose and gradually increasing it, along with adjusting meal sizes, can help manage these symptoms. Less frequent but more serious risks include gallbladder problems and pancreatitis. These medications are typically avoided in patients with a history of pancreatitis or certain endocrine tumors, such as medullary thyroid carcinoma. On the positive side, sustained weight loss from these therapies often leads to better control of blood pressure, cholesterol, and blood sugar, potentially reducing pregnancy-related complications like gestational diabetes once the medication is stopped.
2. Metformin
Mechanism of Action
Metformin plays a key role in managing insulin resistance, offering a different yet complementary approach to treatments like GLP-1 therapies. Originally approved for type 2 diabetes, it’s also widely used for PCOS because of its ability to lower insulin resistance. By reducing glucose production in the liver and improving how the body uses insulin, metformin helps decrease insulin levels in the bloodstream. This is important because elevated insulin can trigger the ovaries to produce too much testosterone and other androgens, which can interfere with regular ovulation and menstrual cycles. By addressing this underlying issue, metformin can help regulate cycles and improve the effectiveness of fertility treatments like ovulation-induction medications.
In the U.S., metformin is typically prescribed in doses ranging from 500 mg to 2,000 mg daily. For those who experience stomach upset with oral forms, Oana Health offers alternatives like Oral Metformin ER starting at $22 per month and Topical Metformin (20% HCL Lotion) for $43 per month. The topical option is especially useful for minimizing gastrointestinal discomfort while still delivering the metabolic benefits of the medication. This flexibility makes it easier for patients to stick with their treatment plan and achieve better outcomes.
Impact on Fertility
Metformin’s ability to lower insulin levels not only supports better metabolic health but also helps promote ovulation and improve fertility. While it’s not a primary fertility medication like letrozole or clomiphene, metformin works well alongside these drugs to enhance outcomes. Studies show that metformin alone isn’t as effective for inducing ovulation as dedicated fertility medications. However, when combined with ovulation-induction treatments, the results are much better - pregnancy rates can go up to 86%, compared to 64% with metformin alone. Among non-obese women with PCOS, pregnancy rates with metformin increased from 7% in the first cycle to 33% by the sixth cycle.
Metformin is particularly effective for individuals with insulin resistance, prediabetes, higher BMI, or visible signs of hyperinsulinemia. For patients using telehealth services like Oana Health, metformin is often part of a personalized plan that may also include GLP-1 medications, nutritional guidance, and collaboration with fertility specialists. This tailored approach helps maximize the chances of success.
Safety and Pregnancy Considerations
Metformin has been extensively studied in women with PCOS who are trying to conceive and is generally considered safe during this time. Many fertility specialists in the U.S. even recommend continuing metformin into early pregnancy, particularly for patients with diabetes or significant metabolic concerns. Research suggests that keeping metformin in the treatment plan through the first trimester may help lower the risk of early pregnancy loss and gestational diabetes. However, whether to continue or stop metformin after conception is a decision made on a case-by-case basis, often in consultation with an OB-GYN or reproductive endocrinologist. Factors like blood sugar control and a history of miscarriage play a role in this decision.
To ensure safety, kidney function is regularly monitored through tests like serum creatinine or eGFR, as there’s a rare but serious risk of lactic acidosis. Regular monitoring and adjustments help ensure that metformin’s benefits extend to both improved fertility and overall health outcomes.
Side Effects
The most common side effects of oral metformin are gastrointestinal issues, such as nausea, diarrhea, abdominal discomfort, and a reduced appetite. These symptoms are most noticeable when starting the medication or increasing the dose. To minimize these effects, doctors often recommend starting with a low dose and gradually increasing it, especially when using extended-release formulations. For those who continue to experience discomfort, topical metformin provides a helpful alternative, reducing stomach-related side effects while still offering the same benefits.
Managing side effects is essential for people seeking to improve fertility, as consistent use over several months is often necessary to regulate cycles and maximize the benefits of combining metformin with ovulation-induction medications. With the right approach, metformin can be a valuable part of a comprehensive fertility plan.
3. Spironolactone
Mechanism of Action
Spironolactone works differently from GLP-1s and metformin by targeting androgens. It acts as an anti-androgen, blocking receptors and reducing testosterone production from the ovaries and adrenal glands. While originally developed as a diuretic for managing blood pressure, it has found a new purpose in treating PCOS symptoms like unwanted facial hair, acne, and hair loss. Research shows that spironolactone can lower testosterone levels, leading to a 20–40% reduction in hirsutism scores after six months of treatment when taken at doses of 100–200 mg daily. This makes it a valuable option for addressing hyperandrogenic symptoms, though it doesn’t play a role in fertility enhancement.
In the U.S., spironolactone is commonly prescribed in daily doses ranging from 50 mg to 200 mg. Oana Health offers affordable options, including Oral Spironolactone starting at $14 per month and Topical Spironolactone for $43 per month. For those seeking a broader approach, a Metformin & Spironolactone pack is available for $32 per month, providing a way to tackle both insulin resistance and androgen-related symptoms at the same time.
Impact on Fertility
Spironolactone is effective for managing hyperandrogenic symptoms, but it doesn’t enhance ovulation or improve pregnancy outcomes. Its primary role is symptom relief - helping reduce acne, unwanted hair, and hair loss - but it won’t regulate menstrual cycles or support ovulation. In fact, spironolactone can cause menstrual irregularities, which can make tracking cycles more difficult.
For women actively trying to conceive, spironolactone is generally not recommended. Current PCOS treatment guidelines prioritize medications like letrozole and metformin for fertility support. Anti-androgens, including spironolactone, are better suited for symptom management in patients not pursuing pregnancy.
Safety and Pregnancy Considerations
Spironolactone is not safe for use during pregnancy due to its anti-androgenic effects, which can lead to fetal feminization and congenital abnormalities, particularly in male fetuses (e.g., ambiguous genitalia). Because of these risks, spironolactone is classified as a Category C/D drug for pregnancy. Women taking this medication must use reliable contraception, and doctors often prescribe it alongside birth control pills to minimize risks and enhance its effectiveness in reducing unwanted hair over a 6–12 month period.
If pregnancy is planned, spironolactone should be discontinued at least one month before trying to conceive. This transition should always be coordinated with a healthcare provider. Through telehealth platforms like Oana Health, patients can manage this change via virtual consultations. Often, they switch to fertility-supportive treatments like metformin while continuing to address other PCOS symptoms.
Side Effects
Spironolactone comes with its own set of potential side effects, which doctors monitor closely. Common issues include elevated potassium levels (hyperkalemia), menstrual irregularities, breast tenderness, dizziness, and gastrointestinal discomfort, affecting 10–30% of patients. Because it’s a potassium-sparing diuretic, regular potassium checks are essential, especially during the initial stages of treatment, with hyperkalemia occurring in up to 10% of users. Electrolyte levels are typically checked monthly at first, then less frequently once they stabilize.
For women focusing on fertility, the menstrual irregularities caused by spironolactone can make cycle tracking and ovulation prediction more challenging. However, for those managing PCOS symptoms while using contraception, these side effects are generally manageable with regular monitoring and adjustments. Pairing spironolactone with lifestyle changes or metformin can help optimize symptom control before transitioning to fertility-focused treatments.
sbb-itb-6dba428
Ovulation with PCOS: Is Clomid or Letrozole better? What Is Ovulation Induction?
Advantages and Disadvantages
When comparing medications for PCOS-related fertility, each option comes with its own set of benefits and risks, shaping how treatments are chosen. Understanding these differences highlights the importance of personalized approaches to managing PCOS and its effects on fertility.
GLP-1 Receptor Agonists indirectly support fertility through weight loss. These medications have been shown to improve ovulation rates (60–70%) and increase live birth outcomes by 20% in obese patients. However, they often cause side effects like nausea (up to 44%), vomiting (15–20%), and gastrointestinal discomfort, leading 5–10% of users to stop treatment. Another concern is the lack of long-term safety data regarding pregnancy, raising questions about potential risks to the fetus during early, undetected pregnancies.
Metformin, classified as a Category B drug, is a safe and effective option for enhancing fertility. It achieves ovulation in 60–85% of combination therapies and boosts pregnancy rates when paired with letrozole (57.9% versus 46.8% with letrozole alone). However, gastrointestinal side effects such as diarrhea (20–30%) and nausea with a metallic taste (10–20% dropout rate) are common. Long-term use may lead to vitamin B12 deficiency, requiring regular monitoring. For individuals who struggle with the side effects of oral metformin, an alternative exists: Oana Health's Metformin HCL Lotion 20%, available for $43 per month, significantly reduces gastrointestinal discomfort.
Spironolactone is effective at lowering testosterone levels by 20–30% but does not promote ovulation. It must be discontinued 1–2 months before conception due to its Category C/D classification, which indicates potential risks to male fetuses, including feminization. Additionally, it may cause menstrual irregularities and anovulation in 10–20% of cases, complicating cycle tracking for those trying to conceive.
Here's a quick comparison of these medications:
| Medication | Fertility Impact | Pregnancy Use | Common Disadvantages |
|---|---|---|---|
| GLP-1 Receptor Agonists | Boosts ovulation (60–70%) via weight loss; increases live births by 20% | Category C; limited safety data, avoid during pregnancy | Nausea (44%), vomiting (15–20%), GI issues; 5–10% discontinuation |
| Metformin | 57.9% pregnancy rate with letrozole; 60–85% ovulation in combos | Category B; safe in the first trimester | GI issues (20–30%), nausea with metallic taste; 10–20% dropout; B12 deficiency |
| Spironolactone | Reduces testosterone by 20–30%; improves menstrual regularity (40–50%) | Category C/D; not safe due to fetal feminization risk | Menstrual irregularities; 10–20% anovulation risk |
For women actively trying to conceive, metformin is the most reliable choice due to its proven fertility benefits. Meanwhile, GLP-1 receptor agonists are ideal for weight management before conception, especially in obese patients. Spironolactone, on the other hand, is better suited for addressing PCOS symptoms when pregnancy isn't an immediate priority.
Conclusion
Selecting the right medication for PCOS largely depends on your fertility goals. For women actively trying to conceive, combining metformin with ovulation-inducing agents like letrozole is often recommended. In fact, one study found that this combination achieved a 57.9% pregnancy rate. Metformin is considered safe during early pregnancy, and for those dealing with digestive side effects, Oana Health's Metformin HCL Lotion 20% provides a gentler alternative with similar benefits.
Other medications play different roles. GLP-1 receptor agonists are commonly used for pre-conception weight management. Even modest weight loss - just 5–10% - in patients with obesity can help restore ovulation and improve fertility outcomes. However, these medications should be discontinued before pregnancy due to limited safety data.
For managing symptoms like hirsutism and acne, spironolactone is often prescribed. Keep in mind, spironolactone isn't intended to boost fertility and should be stopped 1–2 months before trying to conceive. During its use, reliable contraception is essential to avoid unintended exposure.
FAQs
How can losing weight help improve fertility for women with PCOS?
Losing weight can play a major role in improving fertility for women with PCOS by tackling key issues like insulin resistance and hormonal imbalances. These improvements can help bring back regular ovulation, a critical factor for conception.
In fact, shedding just 5-10% of body weight can have a meaningful impact on reproductive health, boosting the chances of pregnancy. Beyond that, weight loss can help regulate menstrual cycles and enhance overall hormonal balance, making it easier to conceive and sustain a healthy pregnancy.
Can Metformin be safely used during pregnancy?
Metformin is often regarded as safe for use during pregnancy, provided it is prescribed and closely monitored by a healthcare professional. It’s commonly recommended for managing conditions such as PCOS and insulin resistance, as it helps regulate blood sugar levels and can contribute to a healthier pregnancy.
That said, it’s crucial to stick to your doctor’s advice and attend regular check-ups to ensure the well-being of both you and your baby.
Why shouldn’t women trying to get pregnant use Spironolactone?
Spironolactone is not suitable for women who are trying to conceive, as it can pose risks to a developing fetus. It’s classified as a teratogen, which means it has the potential to cause birth defects or disrupt normal fetal development if taken during pregnancy.
If you’re planning to get pregnant, it’s crucial to talk to your healthcare provider about safer alternatives. This ensures both your well-being and the health of your future baby.
.webp)



