Latest Research on Personalized PCOS Care
Polycystic Ovary Syndrome (PCOS) affects 5–6 million women in the U.S., with symptoms ranging from weight gain and infertility to insulin resistance. New research has identified four PCOS subtypes - Hyperandrogenic (HA-PCOS), Obesity-related (OB-PCOS), High-SHBG (SHBG-PCOS), and High-LH-AMH (LH-PCOS) - each requiring tailored treatments. Tools like PcosX now classify patients using clinical markers, enabling more precise care. Genetic testing and AI are also advancing diagnosis and treatment, while combination therapies and lifestyle changes improve outcomes. Telehealth platforms are making these personalized treatments more accessible, offering medications and real-time care adjustments. This approach is reshaping how PCOS is managed, improving both health outcomes and quality of life.
Updates on PCOS: Insights from a new review article
New Research on PCOS Subtypes
Four PCOS Subtypes: Risk Profiles and Treatment Approaches
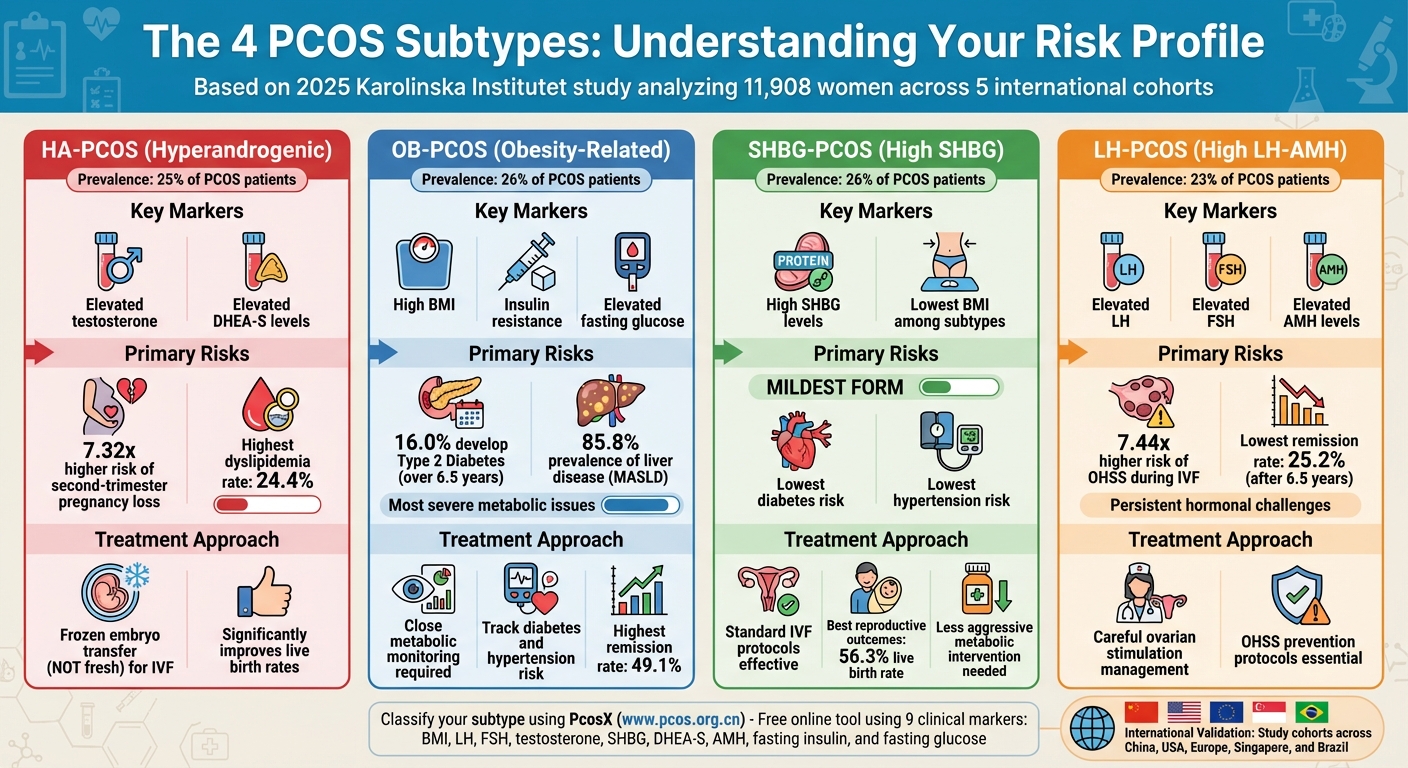
Recent studies have made significant strides in understanding and classifying Polycystic Ovary Syndrome (PCOS). A groundbreaking 2025 study from Karolinska Institutet, published in Nature Medicine, introduced a refined classification system for PCOS. By analyzing data from 11,908 women and focusing on nine clinical markers - BMI, luteinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, sex hormone-binding globulin (SHBG), DHEA-S, anti-Müllerian hormone (AMH), fasting insulin, and fasting glucose - researchers identified four distinct PCOS subtypes. To ensure the classification's reliability, it was validated across five international cohorts, spanning China, the USA, Europe, Singapore, and Brazil, confirming its applicability across diverse ethnic groups.
The subtypes were almost evenly distributed: HA-PCOS (Hyperandrogenic) at 25%, OB-PCOS (Obesity) at 26%, SHBG-PCOS (High-sex hormone-binding globulin) at 26%, and LH-PCOS (High-luteinizing hormone–anti-Müllerian hormone) at 23%. Each subtype presents unique health challenges and responds differently to treatment. To assist clinicians, the researchers developed a free online tool, PcosX (www.pcos.org.cn), which uses the nine clinical measurements to generate a patient's specific risk profile.
The 4 PCOS Subtypes
HA-PCOS is marked by elevated testosterone and DHEA-S levels. Women in this group are at a 7.32 times higher risk of second-trimester pregnancy loss and have the highest rate of dyslipidemia, affecting 24.4% of patients.
OB-PCOS is associated with high BMI, insulin resistance, and elevated fasting glucose. This group faces the most severe metabolic issues, including a 16.0% cumulative incidence of Type 2 Diabetes over 6.5 years and an 85.8% prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD).
SHBG-PCOS, the mildest form, is characterized by high SHBG levels and the lowest BMI. Women in this category experience the best reproductive outcomes, with a 56.3% live birth rate during IVF - the highest among all subtypes. They also have the lowest risks of diabetes and hypertension.
LH-PCOS is defined by elevated LH, FSH, and AMH levels. This subtype has the highest risk of ovarian hyperstimulation syndrome (OHSS) during IVF, with a 7.44 times higher likelihood compared to other groups. Additionally, it has the lowest remission rate, with only 25.2% of women no longer meeting diagnostic criteria after 6.5 years.
These classifications are paving the way for more tailored treatment approaches.
How Subtypes Change Treatment Approaches
The detailed profiles of these PCOS subtypes allow for more personalized treatment strategies. For HA-PCOS, frozen embryo transfer is far more effective than fresh embryo transfer during IVF, significantly improving live birth rates.
Patients with OB-PCOS require close monitoring for metabolic complications, such as Type 2 Diabetes and hypertension, even if their reproductive issues improve over time.
Women with LH-PCOS need careful management during ovarian stimulation to minimize their high risk of OHSS. On the other hand, SHBG-PCOS patients often benefit from standard IVF protocols and typically require less aggressive intervention for metabolic issues.
Interestingly, the remission rates after 6.5 years vary significantly among subtypes. The OB-PCOS group showed the highest remission rate at 49.1%, while LH-PCOS had the lowest at 25.2%, highlighting the persistent hormonal challenges in this group.
"This international collaboration has provided robust evidence that could change how we diagnose, treat, and follow up on women with PCOS." - Elisabet Stener-Victorin, Professor of Reproductive Physiology, Karolinska Institutet
Genetic Testing and AI in PCOS Care
Genetic Testing and GWAS Studies
Genetic testing is reshaping the way PCOS is diagnosed, offering a more precise and personalized approach. Using genome-wide association studies (GWAS), researchers have pinpointed around 19 genetic loci linked to PCOS. This shift moves diagnosis from subjective expert opinions toward a more objective, biology-focused process. These studies have revealed two main biological subtypes of PCOS: the "reproductive" group, which is associated with elevated LH and SHBG levels, and the "metabolic" group, which is marked by higher BMI and insulin levels.
A particularly important discovery is the role of rare DENND1A variants, which appear as early markers in nearly 50% of PCOS-affected families. Research conducted at Mount Sinai between 2020 and 2025 found that genetic signals could increase the risk of PCOS by 3 to 6 times, depending on the subtype.
"The heterogeneity of PCOS is clinically obvious, but there have been limited attempts to specifically analyze it... we wanted to confirm that subtypes we identified were biologically important by demonstrating that they were associated with different genetic signals."
- Andrea Dunaif, MD, Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Icahn School of Medicine at Mount Sinai
In addition to these findings, emerging "omics" studies are uncovering new biomarkers such as HDDC3, SDC2, MAP1LC3A, and OVGP1, which could further refine diagnosis and risk assessment. Tools like custom exome panels and AI algorithms (e.g., PolyPhen2, SIFT) have identified mutations in genes like MAPK14 and RUNX2, opening the door to potential targeted therapies. These discoveries lay the foundation for integrating AI into PCOS diagnostics.
AI Tools for PCOS Diagnosis and Treatment
AI is revolutionizing how PCOS is diagnosed and managed, turning genetic and clinical data into actionable insights. For instance, Convolutional Neural Networks (CNNs) analyzing ovarian ultrasound images have achieved diagnostic accuracies between 95% and 99%, far outpacing traditional manual methods. A review of 25 years' worth of data found that AI and machine learning tools can detect PCOS with an accuracy of 80% to 90%.
AI-driven platforms like PcosX are also making strides. These tools classify PCOS subtypes with impressive accuracy (AUC 0.82–0.95) across various ethnic groups. For patients in the HA-PCOS subtype, PcosX can guide clinicians to choose frozen embryo transfer over fresh transfer, significantly improving live birth outcomes.
"The effectiveness of AI and machine learning in detecting PCOS was even more impressive than we had thought."
- Janet Hall, M.D., Senior Investigator and Endocrinologist, National Institute of Environmental Health Sciences (NIEHS)
To make AI more accessible and trustworthy for clinicians, researchers are turning to Explainable AI (XAI) techniques like SHAP and LIME. These methods provide transparency by highlighting which factors - such as BMI, AMH levels, or follicle count - inform specific treatment recommendations. Although only about 25% of current AI studies in PCOS incorporate XAI methods, this number is expected to grow as AI transitions from research settings to everyday clinical use.
sbb-itb-6dba428
New Treatment Options and Combined Approaches
Combination Drug Treatments
When it comes to treating PCOS, combination therapies have proven to be more effective than single-drug approaches. For instance, pairing GLP-1 receptor agonists with metformin has shown better results than metformin alone. This combination not only reduces weight by 1.37 kg and BMI by 0.88 kg/m² but also boosts SHBG levels by 10.04 nmol/L.
Newer dual agonists, like tirzepatide, are also making waves. These drugs target both GIP and GLP-1 receptors simultaneously, leading to impressive weight loss results. Depending on the dosage, patients can lose between 9 kg (5 mg dose) and 12 kg (15 mg dose) over six months. For comparison, semaglutide 2.4 mg results in weight loss ranging from 11.5 kg to 12.5 kg.
"Combination of GLP1RAs and metformin provides superior benefits over metformin alone in reducing body weight, improving insulin sensitivity, and regulating hormonal imbalances in women with PCOS." - Dr. Li Jiang, Renmin Hospital of Wuhan University
The COMET-PCOS trial compared the effects of low-dose COCPs, metformin (2,000 mg), and their combination. Interestingly, the prevalence of metabolic syndrome was similar across the groups: 26.2% for metformin, 28.6% for the combination therapy, and 28.8% for COCPs alone.
"Low‐dose COCPs effectively managed PCOS symptoms without increasing prevalence of MetS. Our findings challenge the current practice of using metformin alone or with COCPs for lowering cardiometabolic risk." - Dr. Anuja Dokras
However, patients should be mindful of potential side effects. Over 64% of those on metformin-containing treatments report diarrhea, which can impact adherence. Similarly, GLP-1 agents may cause nausea, vomiting, and dizziness, particularly in the early stages. To reduce gastrointestinal discomfort, doctors often recommend starting metformin at a lower dose (500 mg) and gradually increasing it to 2,000 mg.
These pharmacological advancements work best when combined with tailored lifestyle changes, creating a more comprehensive approach to managing PCOS.
Customized Lifestyle Changes
Medical treatments are most effective when paired with lifestyle modifications designed to meet the specific needs of PCOS subtypes. Studies show that even a modest weight loss of 5% to 10% can significantly improve insulin resistance, hormone levels, and ovulation rates in individuals with PCOS who are overweight. The key is to align lifestyle changes with individual metabolic profiles rather than relying on one-size-fits-all recommendations.
One example highlights the power of this approach. At Obesity Week 2023, Dr. Donna Ryan shared telehealth data from 2,643 patients using GLP-1 medications alongside intensive lifestyle coaching. After 12 months, participants who consistently tracked their weight achieved an average loss of 15.6%. Among the 706 participants with prediabetes or diabetes, 81% experienced improvements in their condition, with an average reduction of 5.95 inches in waist circumference.
"Weight loss was robust at year 1 (more than 15%) and sustained at 15 and 18 months, and was accompanied by expected improvements in cardiometabolic risk." - Dr. Donna Ryan
Certain dietary patterns, such as the Mediterranean, DASH, ketogenic, or low-carb diets, have demonstrated positive effects on metabolic and hormonal health in PCOS patients. These diets are often paired with targeted supplements like inositol, vitamin D, vitamin E, and folic acid, which can further enhance metabolic function and ovulation. For patients dealing with severe insulin resistance or obesity, doctors increasingly recommend combining GLP-1 agonists with metformin, alongside these lifestyle changes, for better outcomes.
Emerging research into the gut-PCOS connection is also influencing treatment strategies. Studies suggest that probiotics and prebiotics can help improve insulin sensitivity and reduce inflammation. Additionally, the growing field of precision medicine is using genetic and phenotypic profiles to tailor treatments to specific PCOS subtypes, such as hyperandrogenic forms, obesity-related cases, or those marked by high SHBG or LH levels.
Telehealth for Personalized PCOS Treatment
Why Telehealth Works for PCOS Patients
Telehealth is reshaping how women across the U.S. access care for polycystic ovary syndrome (PCOS). With an estimated 10 million women affected by PCOS, traditional in-person visits often mean long travel times to see specialists. Telehealth removes this hurdle by allowing patients to connect with licensed medical professionals from the comfort of their homes.
Privacy is another major benefit. Many women feel more at ease discussing sensitive symptoms in a private setting, leading to more open conversations and better treatment results [37,38]. In fact, medication adherence among PCOS patients using telehealth has been shown to improve by 45% compared to those relying on traditional care. Platforms like Oana Health support this model with regular digital check-ins and messaging, enabling providers to monitor key factors like blood sugar levels, menstrual cycles, and mood in real time. This allows for treatment adjustments in days instead of months. Telehealth also simplifies coordination among specialists, bringing collaborative care together on a single platform.
"We can pivot treatment plans within days, rather than waiting months." - Dr. Emily Lau, Women's Health Physician
This approach aligns perfectly with the growing focus on personalized PCOS therapies, ensuring patients receive tailored treatments without unnecessary delays. By breaking down barriers to access, telehealth makes personalized care more achievable than ever.
Personalized Treatment Options Available
Thanks to telehealth, platforms are now delivering science-backed, individualized treatments directly to patients. For example, Oana Health offers prescription-based solutions tailored to specific PCOS symptoms, with medications shipped to patients’ homes at no extra cost.
For managing insulin resistance and weight, patients can access oral Semaglutide combined with Metformin for $199/month or Metformin ER starting at $22/month. These medications work best when paired with lifestyle changes. It’s worth noting that 20–30% of patients may experience nausea or stomach upset when starting Semaglutide, but these side effects usually resolve as the dosage stabilizes.
For hormonal imbalances and acne, options include Spironolactone for $14/month or a topical version for $43/month for those wanting to avoid systemic side effects. Women dealing with hair loss can opt for oral Minoxidil at $25/month, while those managing unwanted facial hair might consider Eflornithine cream for $69/month.
Before scheduling a consultation, have your BMI, blood pressure, and current medication list ready. While Oana Health offers cash-pay options, you should check if your insurance requires prior authorization for medications like Semaglutide. GLP-1 treatments are typically approved for individuals with a BMI of ≥30, or ≥27 if weight-related conditions like prediabetes or high blood pressure are present.
"With telehealth, care is no longer optional - it's essential. For women with PCOS, it's the key to accessible, affordable, and effective treatment." - Dr. Sara Martinez, Board-Certified Endocrinologist
The Future of Personalized PCOS Care
Recent research has broken down PCOS into four distinct subtypes, using global data to fine-tune risk predictions and create more targeted treatment plans. Tools like PcosX (www.pcos.org.cn) are now available to help clinicians classify patients into these subtypes, making personalized care more accessible.
Artificial intelligence is also making waves in PCOS care. Machine learning tools are now capable of detecting PCOS with an accuracy rate of 80% to 90%. However, only about 25% of these studies have adopted Explainable AI (XAI) methods, such as SHAP or LIME, which help explain why an algorithm suggests a particular treatment. Dr. Andrea Dunaif, Chief of Endocrinology at the Icahn School of Medicine at Mount Sinai, highlights the potential of this technology:
"The heterogeneity of PCOS is clinically obvious... identifying these genuine subtypes requires analyzing data on a population scale".
"AI offers substantial opportunities to advance PCOS diagnosis and prediction by integrating multimodal data and reducing diagnostic subjectivity." - BMC Medical Informatics and Decision Making
Telehealth is also stepping up, incorporating real-time data to make treatment adjustments on the fly. Future telehealth systems aim to integrate lab results, body composition metrics, and menstrual cycle tracking to automatically refine treatment plans. The global PCOS treatment market is expected to hit $1,666.1 million by 2032, growing at an annual rate of 4.86% starting in 2025. In June 2025, EsterCare, a digital health company, acquired Ovulai, a PCOS management app, to bring personalized digital tools into telemedicine. Companies like Oana Health are already ahead of the curve, offering tailored PCOS treatments that are science-driven and delivered directly to patients.
The future of PCOS care is heading toward a combination of precision biomarkers and behavioral health integration. For instance, new research into the gut microbiome suggests that imbalances in gut bacteria contribute to insulin resistance and inflammation in 44% to 70% of women with PCOS, paving the way for targeted dietary solutions. Additionally, mental health is becoming a core part of PCOS care, with platforms incorporating mental health screenings and Cognitive Behavioral Therapy (CBT)-informed modules into treatment pathways. These advancements are setting the stage for care plans that align with each woman’s unique genetic and metabolic needs.
FAQs
What are the four types of PCOS, and how are they different?
PCOS can be grouped into four key types, each with its own unique traits:
- Hyperandrogenic PCOS (HA-PCOS): This form is marked by elevated male hormone levels, which can heighten the risk of second-trimester miscarriages and lead to imbalances in cholesterol levels.
- Obesity-Related PCOS (OB-PCOS): This type is commonly linked to a higher BMI and insulin resistance, often resulting in more severe metabolic issues and reduced live birth rates.
- High-SHBG PCOS (SHBG-PCOS): A less severe form of PCOS, it tends to present fewer fertility challenges and carries a lower risk of conditions like diabetes and hypertension.
- High-LH/AMH PCOS (LH-PCOS): Defined by increased levels of luteinizing hormone and anti-Müllerian hormone, this type is associated with a greater likelihood of ovarian hyperstimulation syndrome and lower remission rates.
Recognizing these subtypes allows for more personalized treatment approaches, addressing specific health challenges and improving overall outcomes.
How are genetic testing and AI improving PCOS diagnosis and treatment?
Genetic testing and AI technology are changing the game when it comes to diagnosing and managing PCOS. Through genetic profiling, doctors can now pinpoint specific DNA variations tied to hormone production, insulin resistance, and inflammation. This means they can identify risks for conditions like diabetes, infertility, or heart disease earlier - and with far more precision. By stepping away from the one-size-fits-all approach of traditional criteria, treatment can now be tailored to match each person’s unique genetic makeup.
AI takes this a step further by digging deep into data from ultrasounds, lab results, and medical records. Machine learning tools can pick up on subtle ovarian patterns and combine them with hormone levels and other health markers to diagnose PCOS faster and more accurately. On top of that, AI can predict how someone might respond to treatments like insulin-sensitizing drugs or anti-androgens, helping doctors make smarter, more personalized decisions.
At Oana Health, these cutting-edge tools come together to create customized, science-driven treatment plans for PCOS. Whether it’s managing weight, balancing hormones, tackling acne, or supporting mental health, Oana makes comprehensive care accessible - delivering it straight to your doorstep.
How does telehealth improve personalized care for PCOS?
Telehealth is changing the game for women managing PCOS by offering care that's personalized, convenient, and grounded in science. With virtual visits, secure messaging, and home delivery of prescriptions, it removes hurdles like long travel times and endless clinic waits. This makes it much easier for women to access care tailored to their specific needs.
Research underscores the advantages of telehealth in PCOS management. It enables customized nutrition plans, supports better weight management, and boosts adherence to treatments. Features like virtual coaching and real-time data tracking - such as monitoring glucose levels or weight - allow healthcare providers to quickly adjust medications, offer lifestyle advice, and provide mental health support when needed.
A great example of this approach is Oana Health. They provide prescription-based therapies for PCOS-related issues like acne, insulin resistance, and mood changes. These treatments are managed by licensed clinicians and conveniently delivered straight to patients' homes. Telehealth doesn’t just make care more accessible - it ensures it’s continuously refined for the best possible outcomes.
