Vitamin D for PCOS: Benefits and Dosage
Vitamin D plays a key role in managing PCOS by improving hormone balance, menstrual regularity, insulin sensitivity, and reducing inflammation. Between 67% and 85% of women with PCOS are vitamin D deficient, which worsens symptoms like irregular cycles, high androgen levels, and insulin resistance. Research suggests daily supplementation of 3,000–4,000 IU of vitamin D3 can help:
- Regulate hormones: Lower testosterone, increase SHBG, and balance AMH levels.
- Improve insulin function: Enhance insulin sensitivity and reduce HOMA-IR scores.
- Support fertility: Aid in egg development and follicle maturation.
- Reduce inflammation: Decrease markers like CRP and boost antioxidant capacity.
Start by testing your vitamin D levels, then supplement based on your needs. Higher doses (e.g., 4,000 IU daily) are often more effective for PCOS symptoms, though levels above this should only be taken with medical supervision. Consult a healthcare provider to create a tailored plan.
Why Women with PCOS Need Vitamin D
Vitamin D Deficiency in PCOS Patients
Women with PCOS are at a much higher risk of experiencing vitamin D deficiency compared to the general population. Among them, those who are obese tend to have even lower vitamin D levels than their leaner counterparts or individuals without PCOS.
This deficiency stems from two main factors: fat sequestration and genetic variations. Since vitamin D is fat-soluble, it often gets trapped in fat tissue, particularly in individuals with a higher body mass index. Moreover, specific genetic variations in the Vitamin D Receptor (VDR) gene - such as Apa-I, Taq-I, Cdx2, and Fok-I polymorphisms - can impact how vitamin D is processed and utilized in women with PCOS.
"Vitamin D deficiency is more prevalent among women with PCOS when compared to controls." – Mohamad Irani, MD, Center for Reproductive Medicine, Weill Cornell Medicine
The metabolic challenges that accompany PCOS, including insulin resistance and metabolic syndrome, further compound this deficiency. These issues not only reflect underlying metabolic dysfunction but also contribute to hormonal imbalances.
Vitamin D's Effect on Hormones
Vitamin D plays a critical role in regulating reproductive hormones by interacting with receptors in the ovaries, endometrium, and placenta. It directly influences the production of key hormones like progesterone, estrone, and estradiol, all of which are essential for maintaining regular menstrual cycles and supporting fertility.
One of vitamin D's key actions is increasing levels of Sex Hormone-Binding Globulin (SHBG). SHBG binds to testosterone, reducing the levels of free androgens that are responsible for symptoms like acne and unwanted facial hair. Additionally, vitamin D helps regulate Anti-Müllerian Hormone (AMH) levels, which are often elevated in PCOS and linked to disrupted follicle development.
A meta-analysis of 19 studies revealed that vitamin D supplementation significantly improved hormone levels, including DHEAS, SHBG, testosterone, LH, and the Free Androgen Index. In a clinical trial, half of the women with PCOS who had previously experienced irregular periods reported improved cycle regularity after 24 weeks of vitamin D supplementation. By restoring a healthier balance between LH and FSH, vitamin D also paves the way for better insulin response, which is explored further below.
Vitamin D and Insulin Function
Insulin resistance affects approximately 70% of women with PCOS, and the hormonal disruptions tied to PCOS often worsen this metabolic issue. Vitamin D, however, offers a way to interrupt this cycle.
Vitamin D enhances insulin secretion by promoting calcium influx into pancreatic β-cells, which are responsible for producing insulin. It also boosts the expression of insulin receptors, improving the body’s sensitivity to insulin.
"Vitamin D dramatically improves glucose metabolism by increasing insulin production, insulin receptor expression and reducing pro-inflammatory cytokines." – Anmol Mohan, MBBS, Karachi Medical & Dental College
Studies show that even a modest increase in vitamin D levels - about 10 nmol/L (roughly 4 ng/mL) - can lead to a measurable reduction in HOMA-IR values (a marker of insulin resistance) by approximately 0.27 in women with PCOS. In one trial, taking 2,000 IU of vitamin D daily for 12 weeks significantly lowered serum insulin levels and HOMA-IR, particularly in women who were obese or already insulin resistant.
Benefits of Vitamin D for PCOS
More Regular Periods
Research indicates that taking vitamin D supplements can improve menstrual regularity by up to 35% when doses exceed 4,000 IU daily for at least eight weeks. This effect is partially due to vitamin D's ability to lower luteinizing hormone (LH) levels and normalize anti-Müllerian hormone (AMH) levels. For example, one study revealed that women taking 4,000 IU daily experienced more consistent menstrual cycles and better LH levels compared to those taking just 1,000 IU daily. These improvements in cycle regulation also play a role in balancing androgen levels.
Lower Androgen Levels
Vitamin D supplementation has been linked to a reduction in total testosterone and other androgens, which are responsible for symptoms like excessive facial hair and acne. A meta-analysis of 18 trials demonstrated that vitamin D effectively lowered total testosterone levels. In one trial, overweight women taking 50,000 IU of vitamin D3 weekly for 12 weeks saw decreases in both total testosterone and hirsutism scores.
"Vitamin D3 at a treatment dose of 50,000 IU per week improved 25(OH)D levels and decreased the hirsutism scores and androgen levels of overweight women with PCOS." – Clinical Nutrition Journal
Additionally, women taking 4,000 IU daily experienced a 2.81-point drop in hirsutism scores and a similar reduction in acne scores over 12 weeks, compared to a smaller 1.19-point improvement with lower doses.
Better Fertility Outcomes
Beyond regulating menstrual cycles, vitamin D plays a role in supporting fertility. It aids in egg development and may increase the chances of pregnancy for women with PCOS. By regulating calcium levels - crucial for egg maturation - and lowering elevated AMH levels, vitamin D helps restore proper follicle development. Its presence in ovarian receptors highlights its direct involvement in reproductive health.
"Vitamin D supplementation improved menstrual periods, increased folliculogenesis, and decreased blood testosterone levels in PCOS patients, all of which had a significant impact on the ability to procreate." – Anmol Mohan, MBBS
Vitamin D's role in improving insulin sensitivity is also key, as about 70% of women with PCOS face insulin resistance, which can interfere with ovulation. Some studies suggest that combining vitamin D with metformin may further enhance follicular development.
Less Inflammation and Oxidative Stress
Vitamin D can mitigate chronic inflammation and oxidative stress, both of which worsen PCOS symptoms. A study conducted at the Kosar Clinic in Iran involved 90 insulin-resistant women with PCOS who were given either 4,000 IU daily, 1,000 IU daily, or a placebo for 12 weeks. The group receiving 4,000 IU daily saw a reduction in hs-CRP levels by 0.7 mg/L and an increase in Total Antioxidant Capacity (TAC) by 130 mmol/L, while the placebo group experienced worsening inflammation and decreased antioxidant capacity.
A meta-analysis confirmed that vitamin D supplementation can lower hs-CRP levels and boost the body's antioxidant defenses. This is achieved through mechanisms such as inhibiting the NF-κB pathway, which reduces inflammation, and increasing glutathione levels to neutralize harmful free radicals. Moreover, a 2019 Egyptian study found that administering 42,000 IU of vitamin D weekly for 12 weeks reduced inflammatory markers while also improving androgen profiles in women with PCOS.
Don’t Miss Out on the Power of Vitamin D for Your Fertility and Immune Health? Dr Lora Shahine
How Much Vitamin D to Take for PCOS
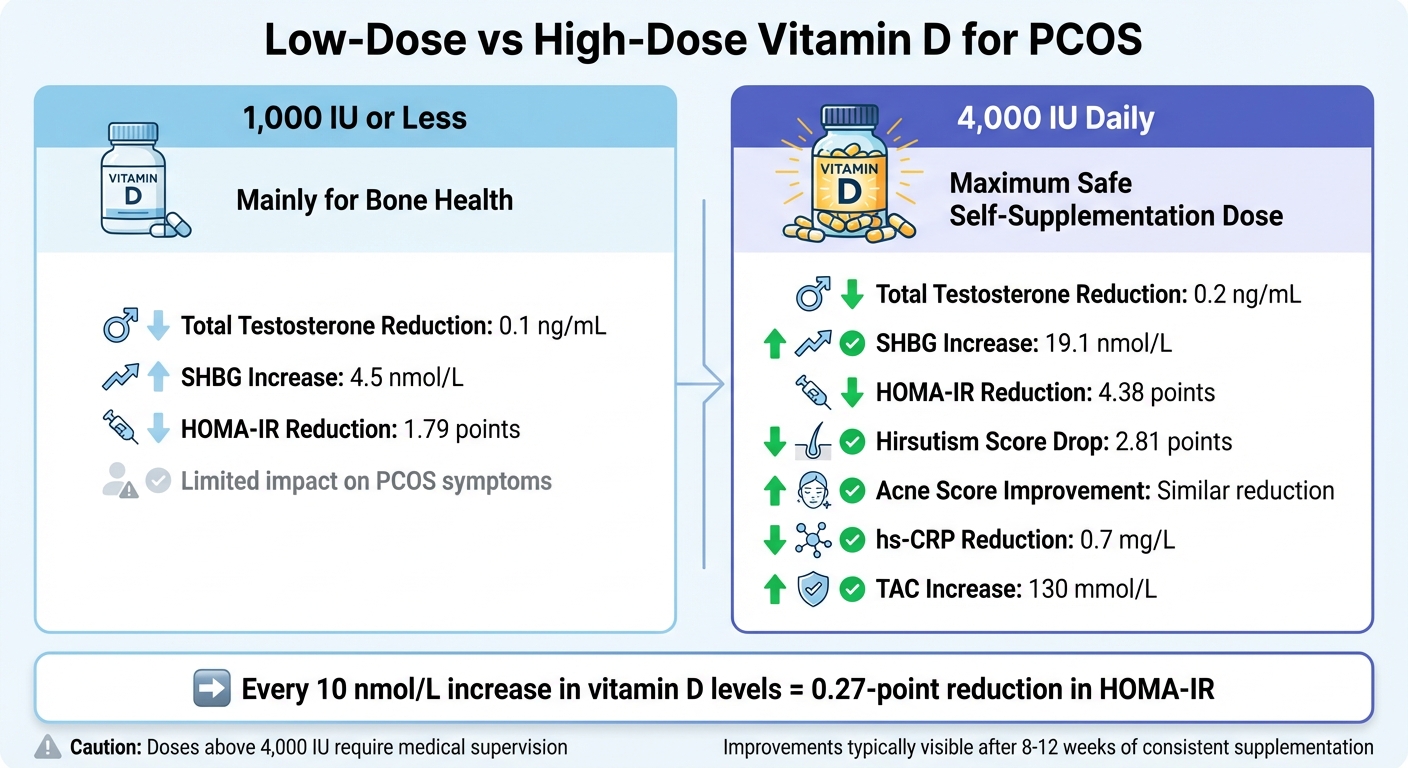
Vitamin D Dosage Comparison for PCOS: 1,000 IU vs 4,000 IU Daily Effects
Understanding the right amount of vitamin D to take is essential for managing PCOS effectively. Let’s dive into what research says about dosage and how it impacts symptoms.
Low-Dose vs. High-Dose Options
The effects of vitamin D on PCOS symptoms vary significantly depending on the dosage. Low doses - 1,000 IU or less per day - are mainly beneficial for bone health but fall short when it comes to addressing PCOS-specific concerns like insulin resistance or high testosterone levels. On the other hand, higher doses, such as 4,000 IU daily, have been shown to significantly lower testosterone, improve insulin sensitivity, and reduce hirsutism.
For instance, studies show that a daily dose of 4,000 IU reduces total testosterone by 0.2 ng/mL, compared to just 0.1 ng/mL with 1,000 IU. It also increases Sex Hormone-Binding Globulin (SHBG) by 19.1 nmol/L, whereas the lower dose only raises it by 4.5 nmol/L. In women with insulin resistance, the higher dose led to a more substantial drop in HOMA-IR scores - 4.38 points versus 1.79 points with the lower dose.
What Research Studies Recommend
Clinical trials back the use of 4,000 IU daily to help manage PCOS symptoms. According to the Food and Nutrition Board of the National Academy of Sciences, this dosage is the highest amount considered safe for daily self-supplementation, with no adverse effects reported.
For those looking for moderate improvements, doses between 2,000 and 3,000 IU daily have been linked to benefits such as reduced BMI and better lipid profiles, especially in women with obesity or insulin resistance. In cases of severe vitamin D deficiency, weekly doses of 50,000 IU are sometimes prescribed to quickly restore levels, but these should only be taken under medical supervision. Research also suggests that serum vitamin D levels increase most noticeably with daily doses up to 3,000 IU, with the effects tapering off between 3,000 and 5,000 IU.
"Vitamin D supplementation in dose of 4000 IU for 12 weeks to insulin-resistant women with PCOS had more beneficial effect on HOMA-IR, mFG score, global acne score, menstrual cycle regularity, BMI, LH levels... as compared to vitamin D supplementation in dose of 1000 IU daily." – Bahadur et al.
These findings emphasize the importance of tailoring your vitamin D intake to your individual needs.
Finding Your Right Dose
Choosing the right dose depends on several personal factors. Start by checking your baseline vitamin D levels. Studies show that 67% to 85% of women with PCOS are deficient, with levels often as low as 12 ng/mL. A simple blood test can help determine the amount of supplementation you need.
Body weight is another key consideration. Women with a BMI of 30 kg/m² or higher often require higher doses to achieve metabolic improvements. This is because obesity is closely tied to more severe vitamin D deficiency and insulin resistance in PCOS.
The severity of your symptoms also matters. If you’re dealing with significant insulin resistance, hirsutism, or irregular periods, research strongly supports a daily dose of 4,000 IU over smaller amounts. For example, every 10 nmol/L increase in serum vitamin D levels has been linked to a 0.27-point reduction in HOMA-IR. Improvements in menstrual regularity and acne are often noticeable after 8 to 12 weeks of consistent supplementation.
For personalized advice on how to incorporate vitamin D into your PCOS management plan, consider consulting a licensed healthcare provider through Oana Health (https://oanahealth.com).
sbb-itb-6dba428
How to Start Taking Vitamin D Safely
Starting vitamin D supplements involves understanding your current levels, choosing the right product, and keeping track of your progress. This personalized approach can help manage hormonal balance and ease PCOS symptoms.
Getting Your Vitamin D Levels Tested
Before diving into supplementation, it's important to know where you stand. A 25-hydroxyvitamin D [25(OH)D] test is the standard for measuring vitamin D levels. This test provides a clear picture of your vitamin D status and can be requested through your primary care doctor, an endocrinologist, or a PCOS-focused telehealth service like Oana Health (https://oanahealth.com).
The results will categorize your levels as deficient (below 20 ng/mL), insufficient (20 to 30 ng/mL), or within the normal range (30 to 50 ng/mL). This baseline is essential for determining how much vitamin D you need to start with.
If you're managing insulin resistance, it’s a good idea to test your HOMA-IR (Homeostasis Model Assessment of Insulin Resistance) simultaneously, as these markers are often interrelated.
Once you know your levels, the next step is finding the right supplement.
Picking a Quality Supplement
When choosing a vitamin D supplement, go for vitamin D3 (cholecalciferol) rather than D2. Vitamin D3 is better absorbed by the body and is the form most commonly used in PCOS-related clinical studies. Look for a supplement that provides 3,000–4,000 IU per day, as this dosage has been shown to improve insulin sensitivity, reduce hirsutism, and regulate menstrual cycles.
Consider a vitamin D3 supplement that also includes magnesium and calcium. These nutrients play a role in glucose regulation and follicular development. Women with PCOS are significantly more likely to have magnesium deficiencies, which makes this combination particularly helpful.
"We recommend at least 4,000 IU vitamin D daily if TTC [trying to conceive]." – Angela Grassi, MS, RDN, LDN, Founder of the PCOS Nutrition Center
If you’re taking metformin, vitamin D can potentially boost its metabolic effects. Be sure to discuss this combination with your healthcare provider.
After starting supplementation, it’s important to monitor your progress.
Tracking Progress and Adjusting Doses
After 12 weeks of consistent supplementation, retest your vitamin D levels to see if you’ve reached the target range of 30–50 ng/mL. Studies often track progress at intervals such as 4, 8, and 12 weeks.
Keep an eye on how your body responds by noting changes in your menstrual cycle, skin condition, and hair growth. These improvements often become noticeable within 8 to 12 weeks and align with normalized vitamin D levels, which can directly benefit PCOS management. You may also observe shifts in your weight as your metabolic health improves.
If your levels remain low after 12 weeks of taking 3,000–4,000 IU daily, consult your doctor. Research indicates that benefits tend to level off beyond 3,000 IU, and there’s limited data on doses above 5,000 IU. The 4,000 IU daily limit is considered the maximum safe amount for adults without medical supervision.
For more tailored advice on testing, supplements, and ongoing care, Oana Health (https://oanahealth.com) offers telehealth consultations with licensed professionals experienced in PCOS treatment.
Safety and Side Effects
Vitamin D is generally considered safe when taken within the recommended limits, but exceeding these limits can lead to complications. Understanding these risks ensures safer supplementation practices.
Side Effects of Excessive Intake
For adults, the Food and Nutrition Board of the National Academy of Sciences sets the safe upper limit for vitamin D at 4,000 IU per day. Going beyond this amount without medical supervision can result in vitamin D toxicity. This condition, marked by hypercalcemia (elevated calcium levels in the blood), can harm bones, teeth, and muscles. If higher doses are necessary, they must be taken under strict medical supervision and not self-administered. Additionally, large doses of vitamin D may interact with certain medications, such as corticosteroids and cholesterol-lowering drugs.
These potential side effects underscore the need for professional oversight when adjusting your vitamin D intake.
When to Consult a Doctor
Monitoring is key to ensuring safe vitamin D use. You should consult a doctor if you have health conditions that affect vitamin D metabolism, such as kidney or liver issues, uncontrolled thyroid disorders, or hyperprolactinemia - conditions that were excluded from safety trials. A doctor can perform a 25-hydroxyvitamin D blood test to assess your baseline levels and recommend an appropriate starting dose. It’s especially important to seek medical advice if you’re taking medications that influence vitamin D metabolism or are considering doses above 4,000 IU daily.
For tailored advice and ongoing monitoring, platforms like Oana Health (https://oanahealth.com) provide telehealth consultations with licensed professionals who specialize in PCOS treatment.
Conclusion
Vitamin D plays a key role in managing PCOS by influencing hormones, insulin levels, and inflammation. Studies show that supplementing with vitamin D can help balance hormones, improve insulin sensitivity, and reduce fasting insulin levels. It’s also linked to more regular menstrual cycles, improved follicle maturation, and lower inflammation markers like C-reactive protein.
For many women with PCOS, daily doses of 3,000–4,000 IU of vitamin D have proven helpful, though individual needs depend on factors like baseline vitamin D levels, BMI, and insulin resistance. With 67% to 85% of women with PCOS experiencing vitamin D deficiency, testing and tailoring supplementation to your specific needs is critical. This approach ensures vitamin D becomes an effective part of your PCOS treatment plan.
To get started, work with a healthcare provider to create a personalized supplementation strategy. Begin with a 25-hydroxyvitamin D blood test, and adjust your dose after 12 weeks of supplementation as needed. This is especially important since responses to vitamin D can vary - women with obesity or insulin resistance often see the most noticeable metabolic benefits.
For a comprehensive approach to PCOS management, Oana Health (https://oanahealth.com) offers access to licensed medical professionals who specialize in hormonal health. They provide personalized treatment plans, including vitamin D recommendations, delivered directly to your door with free shipping. By combining these services with the findings on vitamin D, you can take meaningful steps toward managing your PCOS symptoms.
While vitamin D is a valuable tool, it works best as part of a broader plan that includes professional guidance and regular monitoring.
FAQs
How does vitamin D support women with PCOS?
Vitamin D plays an important role in managing PCOS symptoms by boosting insulin sensitivity, which helps keep blood sugar levels in check and reduces insulin resistance. This, in turn, can address some of the underlying issues associated with PCOS. It also helps decrease excess androgens (male hormones), potentially improving menstrual cycles and easing symptoms like acne and unwanted hair growth.
Beyond that, vitamin D may contribute to maintaining a healthier BMI, lowering triglyceride levels, and supporting overall hormonal balance. For women dealing with PCOS, keeping vitamin D levels in the right range could be a straightforward yet impactful way to enhance their overall health.
Can taking too much vitamin D be harmful if I have PCOS?
Yes, overloading on vitamin D can be harmful, even for those managing PCOS. While vitamin D plays a key role in hormone balance and overall well-being, exceeding the recommended daily intake can lead to toxicity. This might bring on symptoms such as nausea, vomiting, kidney issues, or an excess of calcium in the blood (known as hypercalcemia).
For women with PCOS, it’s crucial to work with a healthcare provider to determine the correct dosage tailored to your specific needs. Following their advice ensures you reap the benefits of vitamin D without unnecessary risks.
What is the right vitamin D dosage for managing PCOS?
To figure out the right vitamin D dosage for managing PCOS, the first step is to get a 25-hydroxy-vitamin D blood test through your healthcare provider. This test will show whether your levels are deficient (<20 ng/mL), insufficient (20–30 ng/mL), or sufficient (>30 ng/mL). Once you have the results, your doctor can guide you on the proper dosage.
If your levels are deficient, the usual recommendation is 2,000–4,000 IU daily or 50,000 IU weekly, but this should always be done under medical supervision. For insufficient levels, 2,000 IU daily is often enough to improve levels. To maintain sufficient levels, a lower dose of 400–1,000 IU daily is generally adequate. For PCOS-specific concerns like insulin resistance or hormonal imbalances, research suggests that taking 4,000 IU daily for 12 weeks may offer benefits.
It's important to re-check your vitamin D levels after 8–12 weeks to see if adjustments are needed. For extra support, telehealth services like Oana Health can review your test results, recommend a tailored dosage, and even deliver supplements to your door. Just keep in mind, you should never exceed 10,000 IU daily unless directed by your doctor, as this could lead to toxicity.
