Anti-Androgen Medications for Acne: Options
Struggling with hormonal acne? Anti-androgen treatments target the root cause - hormones like testosterone and DHT that overstimulate oil glands. These treatments can reduce oil production, unclog pores, and calm inflammation. Here’s a quick guide to four options:
- Oral Spironolactone: Blocks androgen receptors and reduces sebum production. Effective for adult women with hormonal acne. Side effects may include menstrual changes and mild headaches. Not suitable during pregnancy.
- Combined Oral Contraceptives (COCs): FDA-approved for acne. Regulate hormones and reduce androgen activity. Best for women needing contraception. Risks include increased chances of blood clots.
- Topical Clascoterone: A cream that blocks DHT at the skin level. Works for both men and women with minimal side effects. Results may take 3 months.
- Topical Spironolactone: Localized treatment for reducing oil production. Fewer systemic effects but not FDA-approved.
Each option has unique benefits and limitations. Your choice depends on your acne severity, hormonal profile, and personal preferences. Always consult a healthcare provider to find the best fit for you.
1. Spironolactone (Oral)
Mechanism of Action
Oral spironolactone tackles hormonal acne through four key pathways. First, it blocks androgen receptors, stopping DHT and testosterone from binding to receptors in the skin. Second, it reduces the activity of 5-alpha reductase by helping the liver clear testosterone more effectively. Third, it increases levels of steroid hormone-binding globulin (SHBG), a protein that binds to free testosterone in the bloodstream, making it unavailable to stimulate oil glands. Lastly, it inhibits androgen-stimulated sebocyte proliferation, which reduces sebum production - a major contributor to acne. By targeting hormonal triggers, spironolactone directly addresses the root causes of sebum overproduction and inflammation, which explains its success in clinical studies.
Efficacy
In a 2023 SAFA phase 3 trial, 82% of women taking spironolactone reported improvement after 24 weeks, compared to 63% in the placebo group. By week 12, 19% of participants on spironolactone achieved clear or nearly clear skin, compared to just 6% of those on placebo. Another retrospective study of 110 patients found that 85% experienced improvement in acne severity, with 55% achieving complete clearance. Across multiple studies, women treated with spironolactone showed acne lesion reductions ranging from 50% to 100%.
"Spironolactone improved outcomes compared with placebo, with greater differences at week 24 than week 12. Spironolactone is a useful alternative to oral antibiotics for women with acne." - BMJ 2023 (SAFA Trial Investigators)
Typical starting doses range from 25mg to 50mg daily, with gradual increases to 100mg–200mg for optimal results. Initial improvements are usually noticeable within 6–8 weeks, but full therapeutic effects often take 3 to 6 months. One study also noted a 37.5% improvement in body acne for women taking 75–150mg daily, alongside facial acne improvements.
Safety and Side Effects
Clinical studies report that 29% of patients experienced increased urination, 22% had menstrual irregularities, 17% noted breast tenderness, 14% reported headaches, and 12% experienced dizziness. In the SAFA trial, headaches were more frequent with spironolactone (20% vs 12% for placebo). While 46% of patients in one retrospective study reported side effects, only 5% discontinued treatment due to bothersome symptoms.
The risk of hyperkalemia (high potassium) is low, particularly for healthy women under 45, where the risk is less than 1%. However, it increases to 16.7% in women aged 46–65. Routine potassium monitoring may not be necessary for younger, healthy women but is recommended for older patients or those with kidney or heart conditions. Patients should avoid potassium-enriched salt substitutes and limit high-potassium foods like bananas, avocados, and spinach.
Spironolactone is contraindicated during pregnancy due to the risk of feminization in male fetuses, so reliable contraception is essential. While the FDA includes a warning about tumor risks based on high-dose animal studies, large human studies have not found a strong link between spironolactone and breast cancer. These safety considerations help identify the patients most likely to benefit from this treatment.
Target Patient Groups
Spironolactone is especially effective for adult women (typically over 25) who experience hormonal acne, including perimenstrual flares or acne that hasn’t responded to antibiotics or isotretinoin. Studies indicate that 79% to 82% of post-adolescent women with acne fail conventional treatments, making spironolactone a key option for persistent hormonal acne. While traditionally prescribed for adult women, its use among adolescent females with hormonal acne is growing.
"The majority of women who present with late-onset or post-teen persistent AV, even with classic hormonal-pattern AV, do not exhibit an increase in serum androgen levels. Regardless, this latter subset still benefits substantially from oral spironolactone." - James Q. Del Rosso, DO
If you're struggling with persistent hormonal acne and are considering spironolactone, Oana Health offers telehealth consultations with licensed professionals who can assess your situation and provide treatment, delivered straight to your door with free shipping.
2. Combined Oral Contraceptives
Mechanism of Action
Combined oral contraceptives (COCs) take a systemic approach to managing hormone-driven acne. They work by increasing sex hormone-binding globulin (SHBG), which binds free testosterone, while also suppressing luteinizing hormone (LH) and follicle-stimulating hormone (FSH) to reduce ovarian androgen production. Additionally, they inhibit 5α-reductase activity in sebaceous glands, preventing the conversion of testosterone into dihydrotestosterone (DHT). Some progestins, like drospirenone and cyproterone acetate, directly block androgen receptors, and COCs also lower adrenal androgen production by reducing adrenocorticotropic hormone (ACTH) levels.
"Drospirenone is the only FDA-approved progestin with direct androgen receptor–blocking properties." - Arrington EA et al., Cutis
Efficacy
The FDA has approved three specific COC formulations for acne treatment: Ortho Tri-Cyclen (norgestimate/ethinyl estradiol), Estrostep (norethindrone acetate/ethinyl estradiol), and Yaz (drospirenone/ethinyl estradiol). Research shows that most COCs are effective for treating acne, with no single formulation consistently outperforming the others.
In a 2008 randomized, double-blind trial by Koltun et al., patients using Yaz (3 mg drospirenone/20 mcg ethinyl estradiol) were 4.3 times more likely to achieve clear or nearly clear skin compared to those on a placebo. Similarly, a 2013 study by Palli et al. reported significant improvements in both inflammatory and non-inflammatory acne lesions. Noticeable results often appear within 3 to 6 months of consistent use. While antibiotics may deliver faster results within three months, COCs match their efficacy at six months, typically reducing acne lesions by about 55%. Another study found that treatment with cyproterone acetate (2 mg) and ethinyl estradiol (0.35 mg) resulted in 83% of patients reporting subjective improvement in hirsutism and 40% showing visible acne improvement after three months.
Safety and Side Effects
Common side effects of COCs include intermenstrual spotting (10.5%), headaches (8.6%), nausea (6.4%), breast tenderness, and mood changes. The most serious risk is an increased likelihood of venous thromboembolism (VTE). COC users face a threefold increase in VTE risk, with an incidence of about 3.4 events per 10,000 woman-years compared to 1 event per 10,000 in non-users. However, this risk is still lower than during pregnancy, where VTE rates range from 5 to 12 events per 10,000 woman-years.
Drospirenone-containing COCs carry a 1.5- to 2.0-fold higher VTE risk compared to those with levonorgestrel. On the other hand, formulations with natural estrogens like estradiol or estetrol have about a 33% lower VTE risk than those containing ethinyl estradiol. COCs are contraindicated for women over 35 who smoke heavily (15 or more cigarettes daily) and those with a history of migraine with aura, blood clots, or uncontrolled hypertension. Blood pressure should be checked before starting COCs and monitored during follow-ups. On the upside, COCs provide long-term protection against endometrial and ovarian cancer, with benefits lasting up to 20 years after discontinuation.
Target Patient Groups
COCs are ideal for postmenarcheal to premenopausal women who need contraception or are not planning a pregnancy. They are especially effective for women with late-onset acne (over 25 years old), particularly those experiencing jawline acne, menstrual flares, or signs of hyperandrogenism like hirsutism. Since 70% to 80% of individuals with polycystic ovary syndrome (PCOS) experience acne, COCs can be highly beneficial for this group. FDA approval for acne treatment generally applies to females aged 15 and older (or 14 and older for Yaz) who have reached menarche. Additionally, COCs can act as a preparatory step for women who may later require isotretinoin, as they meet the requirement for effective contraception.
If you're exploring COCs for hormonal acne and need contraception, Oana Health offers telehealth consultations with licensed professionals who can help evaluate your needs and create a personalized treatment plan.
3. Clascoterone (Topical)
Mechanism of Action
Clascoterone is a topical androgen receptor inhibitor designed to block DHT (dihydrotestosterone) from binding in the pilosebaceous unit. This action helps reduce both sebum production and inflammation. Once applied, it is rapidly metabolized into an inactive form, cortexolone, which minimizes systemic effects.
"Clascoterone targets androgen receptors at the site of application and is quickly metabolized to an inactive form, thus limiting systemic activity." - Hebert A, MD
Efficacy
In two Phase 3 clinical trials involving 1,440 patients aged 9 and older, clascoterone 1% cream demonstrated treatment success rates of 20.3% and 18.4%, compared to 6.5% and 9.0% for placebo after 12 weeks. Patients experienced an average reduction of around 19–20 inflammatory and non-inflammatory lesions. Remarkably, clascoterone is the first FDA-approved acne treatment with a new mechanism of action since isotretinoin's approval in 1982.
Safety and Side Effects
The most common side effects include mild local reactions such as redness, scaling, dryness, stinging, burning, and itching, reported in 52.6% to 55.3% of patients. Despite these reactions, the discontinuation rate was low, ranging from 0.5% to 0.8%. In Phase 2 trials, some adolescents experienced temporary suppression of the HPA (hypothalamic-pituitary-adrenal) axis, which resolved after stopping treatment.
Target Patient Groups
Clascoterone is FDA-approved for treating acne vulgaris in individuals aged 12 and older. It’s a promising choice for male patients who cannot use systemic hormonal therapies and for females who prefer to avoid oral medications or have not responded well to other topical treatments. Clinicians may recommend it as a first-line option for mild to moderate acne or combine it with oral antibiotics for moderate cases. Treatment outcomes are typically assessed after three months.
For tailored acne treatment plans, including options like topical anti-androgens, check out Oana Health for a telehealth consultation with a licensed professional.
How to treat hormonal acne with spironolactone in 2026: dermatologist and acne expert explains
sbb-itb-6dba428
4. Topical Spironolactone
Topical spironolactone offers a targeted way to address acne while avoiding the broader systemic effects of its oral version. By blocking androgen receptors directly in the skin, it prevents these hormones from stimulating the sebaceous glands in the pilosebaceous unit. This localized action reduces sebum production and, in turn, helps control the development of comedones and inflammatory lesions like pustules. Its focused mechanism makes it a promising option for reducing acne symptoms.
"Topical spironolactone is different from oral spironolactone, and it minimizes the side effects that are typically associated with oral spironolactone while still effectively combating acne." – Curology Team
Efficacy
Research shows that applying a 5% spironolactone cream twice daily can significantly reduce acne within just eight weeks. In fact, one study found it more effective than clindamycin at reducing pustules. A meta-analysis conducted in 2025, involving 643 participants, further confirmed its effectiveness. Both oral and topical spironolactone significantly lowered the Acne Severity Index, with a mean reduction of –6.53 (95% CI: –10.83 to –2.22, p = 0.003). However, to see full results, consistent use over several months may be necessary.
Safety and Side Effects
Topical spironolactone has shown a strong safety record, with side effects occurring at rates similar to placebo. Unlike the oral form, the topical version minimizes systemic side effects. The most common reactions are mild and localized, such as redness, dryness, or slight scaling of the skin. Importantly, the regular lab monitoring required for oral spironolactone - like potassium and kidney function checks - is generally unnecessary with topical use. This makes it a more convenient option for those seeking a targeted treatment with fewer systemic concerns.
Target Patient Groups
Thanks to its safety and effectiveness, topical spironolactone is a versatile choice for a wide range of patients. While oral spironolactone is typically reserved for women due to its potential hormonal effects on men, the topical form is suitable for both men and women. Its localized action provides the anti-androgenic benefits without significant hormonal side effects, making it an excellent alternative to systemic treatments. However, anyone who is pregnant or planning to become pregnant should consult a healthcare provider before using this medication.
For a tailored acne treatment plan, including the option of topical spironolactone, visit Oana Health to schedule a telehealth consultation with a licensed medical professional.
Advantages and Disadvantages
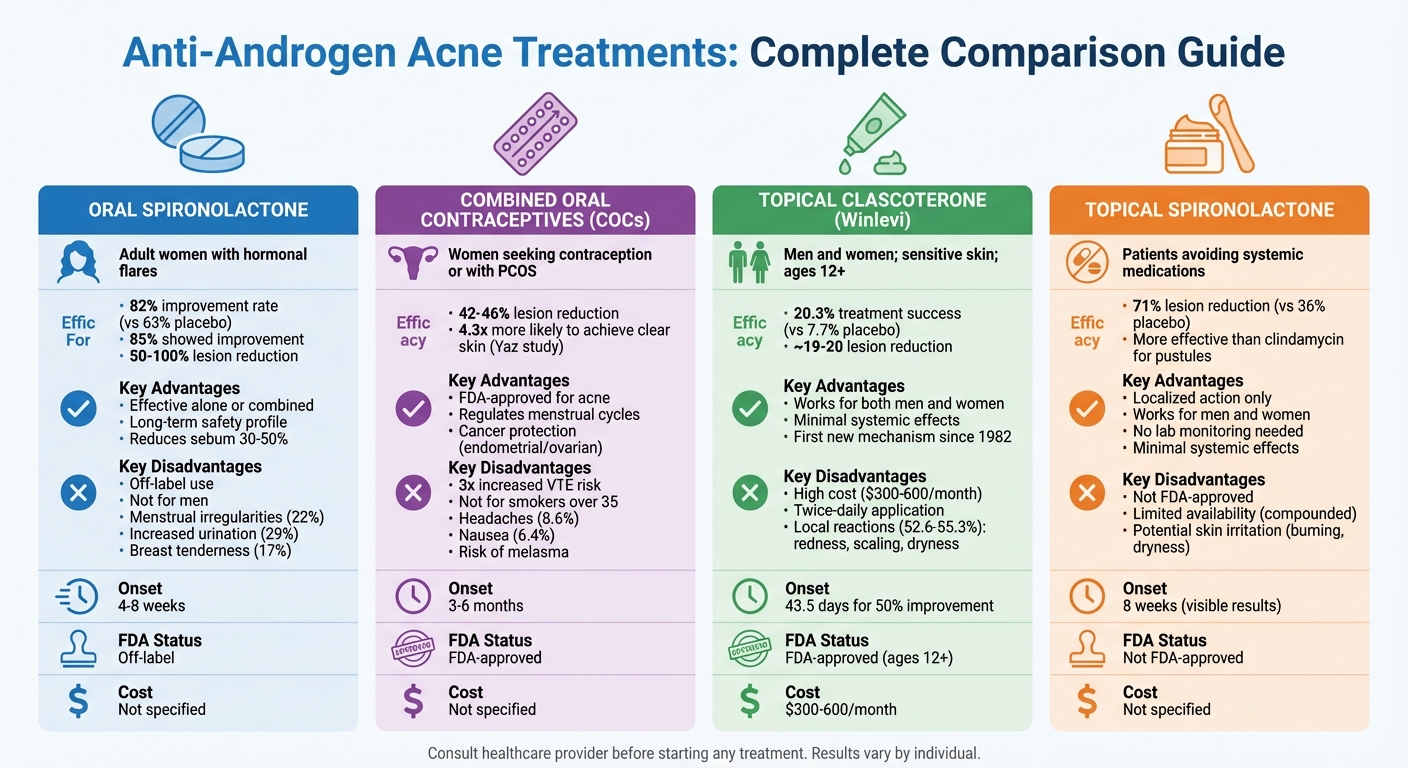
Comparison of Anti-Androgen Acne Treatments: Efficacy, Side Effects, and Best Candidates
Each acne treatment comes with its own set of benefits and challenges, making it essential to weigh the options carefully. Below is a breakdown of the key strengths and limitations of various therapies to help guide your decision.
Oral spironolactone is a reliable choice for addressing hormonal acne, particularly inflammatory papules along the jawline and neck. It also reduces sebum production by 30%–50%. This option is especially helpful for women who can't use oral contraceptives, such as smokers over 35 or those at risk for blood clots. However, it’s important to note that spironolactone is used off-label for acne, and potential side effects include diuretic effects (29% of patients), menstrual irregularities (22%), and breast tenderness (17%). Additionally, it carries a risk of feminizing male fetuses, making contraception a necessity for those using this treatment.
Combined oral contraceptives (COCs) are FDA-approved for acne treatment and can reduce lesion counts by 42%–46%. Beyond acne, they help regulate menstrual cycles and even offer some protection against certain cancers. However, they come with risks, including a threefold increase in the likelihood of venous thromboembolism (VTE). COCs are not suitable for smokers over 35, individuals with a history of blood clots, or those with certain migraine types. Another possible downside is the development of melasma in some users.
Topical clascoterone (Winlevi) is another FDA-approved option, suitable for patients aged 12 and older. It works for both men and women, with minimal systemic side effects. Clinical trials showed it achieved treatment success in 19.9% of patients compared to 7.7% for the placebo, and it delivered a 50% improvement in lesion counts faster than tretinoin 0.05% cream (43.5 days versus 57.0 days). The main drawback? Cost. A one-month supply typically ranges from $300 to $600.
Topical spironolactone provides localized treatment with minimal systemic impact. A 5% gel formulation reduced total lesion counts by 71% compared to 36% for the placebo. It’s an option for both men and women and doesn’t require routine lab monitoring. However, it isn’t FDA-approved, which means it’s often compounded by pharmacies, affecting availability. Some users report burning, dryness, or itching, though formulations with lipid carriers tend to be gentler on the skin.
| Treatment Option | Best For | Key Advantages | Key Disadvantages | Onset of Action |
|---|---|---|---|---|
| Oral Spironolactone | Adult women with hormonal flares | Effective; can be used alone; long-term safety | Off-label use; not suitable for men; menstrual irregularities | 4–8 weeks |
| Combined Oral Contraceptives | Women seeking contraception or with PCOS | FDA-approved; regulates cycles; cancer protection | Increased VTE risk; not for smokers >35 | ~3 months |
| Topical Clascoterone | Men and women; sensitive skin | Suitable for men; minimal systemic effects | High cost ($300–$600/month); twice-daily use | 43.5 days for 50% improvement |
| Topical Spironolactone | Patients avoiding systemic medications | Localized action; no lab monitoring needed | Not FDA-approved; potential skin irritation | Data pending |
Choosing the right treatment depends on your unique hormonal profile and acne needs. Consult a healthcare professional to develop a plan that works best for you. For a tailored approach, Oana Health offers telehealth consultations with licensed professionals who can recommend the most suitable anti-androgen therapy for your situation.
Conclusion
When it comes to choosing an anti-androgen treatment for acne, the right option depends on your specific needs and circumstances. Systemic treatments like oral spironolactone and combined oral contraceptives (COCs) provide broad hormonal regulation, while topical options such as clascoterone and topical spironolactone focus on localized effects with minimal impact on the rest of your body. Keep in mind that hormonal therapies often take about 3–6 months to show noticeable results. The choice ultimately comes down to balancing effectiveness, potential side effects, cost, and your overall health profile.
To make an informed decision, it’s essential to consider your hormonal patterns and acne severity. Telehealth platforms can make this process easier by connecting you with specialists from the comfort of your home. For instance, Oana Health offers personalized consultations with licensed medical professionals who focus on hormonal acne treatments. They provide prescription-based solutions, including oral spironolactone and topical spironolactone, shipped directly to your door with free delivery - making the journey to clearer skin more convenient than ever.
FAQs
What’s the difference between oral and topical anti-androgen treatments for acne?
Oral anti-androgen medications, such as spironolactone and certain oral contraceptives, work throughout the body to reduce androgen activity. By lowering androgen levels, these medications help decrease oil production on both the face and body. However, they may come with side effects, including changes in menstrual cycles, potassium imbalances, and elevated liver enzymes. It's also important to note that these medications are not safe to use during pregnancy.
On the other hand, topical anti-androgens like clascoterone (Winlevi) are applied directly to the skin. They target androgen receptors locally, which means they work at the application site with minimal absorption into the bloodstream. This makes them effective at reducing acne while avoiding many of the systemic side effects seen with oral treatments. That said, mild skin irritation can occur in some cases.
Oral anti-androgens are typically recommended for moderate to severe hormonal acne, as they can address issues across the entire body. Meanwhile, topical options are a newer alternative that focuses specifically on facial acne and offers comparable results with fewer risks. For a tailored approach to your acne treatment, Oana Health provides telehealth services to help you find the right prescription option for your needs.
How long does it take for anti-androgen treatments to improve acne?
Anti-androgen treatments for acne usually take about 3 to 6 months before you start seeing visible improvements. However, the exact timeline can differ based on factors like the type of medication, the dosage prescribed, and how your body responds to the treatment.
Sticking to the plan is crucial - make sure to follow your healthcare provider’s recommendations carefully and allow enough time for the treatment to take effect. If you're feeling unsure about your progress or have concerns, it's always a good idea to check in with your doctor for advice.
What are the potential side effects of oral spironolactone and combined oral contraceptives when treating acne?
Both oral spironolactone and combined oral contraceptives (COCs) are effective options for managing acne, but they come with their own sets of potential side effects.
Spironolactone might lead to side effects such as irregular menstrual cycles, breast tenderness, or elevated potassium levels. Meanwhile, COCs carry risks like blood clots, high blood pressure, and nausea.
Before deciding on a treatment plan, it’s essential to consult with a licensed healthcare provider. They can review your medical history and help you choose an option that best suits your health needs while minimizing potential risks.
