Checklist for Starting Metformin and Spironolactone
Starting metformin and spironolactone can help address insulin resistance and hormonal imbalances, especially for conditions like PCOS. Metformin improves insulin sensitivity, while spironolactone lowers androgen levels, helping with symptoms like acne, unwanted hair growth, and hair loss. To begin this treatment safely, follow these steps:
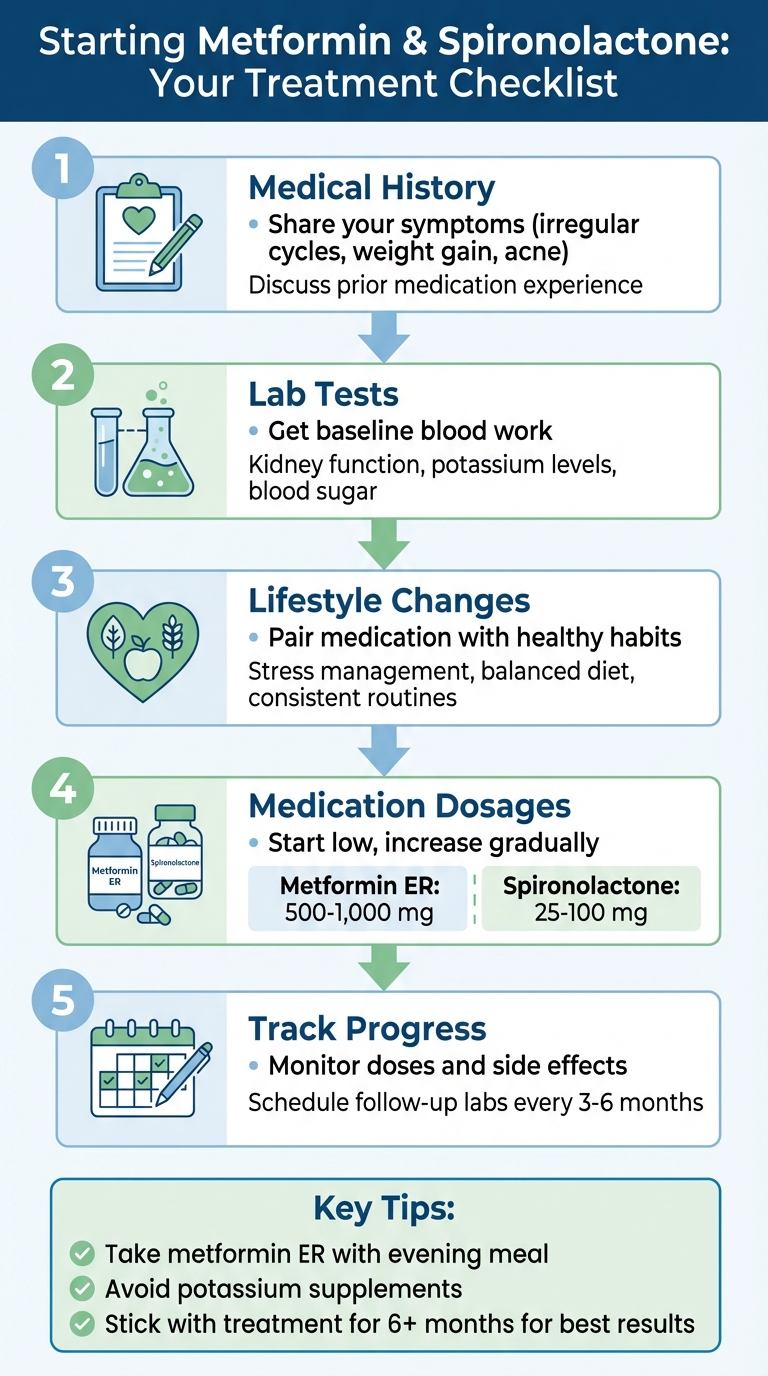
- Medical History: Share symptoms (e.g., irregular cycles, weight gain, acne) and any prior experience with these medications.
- Lab Tests: Check kidney function, potassium levels, and blood sugar to ensure treatment is safe.
- Lifestyle Changes: Pair medication with stress management, a balanced diet, and consistent routines.
- Medication Dosages: Start with low doses (e.g., 500–1,000 mg metformin ER, 25–100 mg spironolactone) and increase gradually under medical guidance.
- Track Progress: Use a tracker for doses and side effects, and schedule follow-up labs regularly to monitor your response.
Key Tips:
- Take metformin ER with your evening meal to reduce stomach discomfort.
- Avoid potassium supplements unless directed by your doctor.
- Report serious side effects like muscle weakness, irregular heartbeat, or severe vomiting immediately.
Stick to the plan for at least six months to see the best results, including improved cycles, reduced hair growth, and better metabolic health. Regular follow-ups ensure your treatment stays on track.
5-Step Checklist for Starting Metformin and Spironolactone Treatment
A Magic Pill for Acne, PCOS, Female Hair Loss, Hirsutism and HS
Before You Start Treatment
Preparing properly before starting metformin and spironolactone can make your treatment safer and more effective. Sharing a full picture of your health with your healthcare provider is key to determining if this combination is right for you.
Review Your Medical History
Have an open conversation with your provider about your medical history. Highlight any key PCOS symptoms you’ve experienced, such as irregular cycles, weight gain, hair loss, excessive hair growth, or acne. If you have a history of insulin resistance or have taken metformin before, be sure to mention it. Especially bring up any side effects, like nausea or an upset stomach, as this could lead your provider to consider alternatives, like topical metformin. If using a telehealth service, be thorough when completing the intake form so your physician can review your case accurately.
Get Baseline Lab Tests
Baseline blood tests are essential to ensure the safe use of these medications. Your provider will likely check kidney function (serum creatinine, eGFR), electrolytes (like potassium and urea), fasting blood glucose, and HbA1c to assess your insulin sensitivity. If your potassium levels exceed 5.0 mEq/L or your creatinine level is above 2.5 mg/dL, treatment may not be recommended. These tests are also repeated during follow-ups to monitor how your body is responding to the medications.
Plan Your Lifestyle Changes
For the best results, pair these medications with healthy lifestyle habits. Stress management is crucial, as high cortisol levels can worsen insulin resistance, promote weight gain, and increase inflammation. Use a calorie calculator to create a tailored eating plan and steer clear of dietary triggers. Adding foods rich in phytoestrogens - like soy and flaxseed - may help support hormonal balance. Take your medication consistently, as initial improvements often appear within 3–4 weeks, with more noticeable changes over several months. With these steps in place, you’ll be ready to begin your treatment journey.
How to Start Your Medications
Start Low and Increase Gradually
When beginning treatment, start with 500–1,000 mg of metformin ER once daily and 25–100 mg of spironolactone daily. This gradual approach helps your body adjust, reducing the likelihood of side effects. For metformin, your dose is usually increased by 500 mg each week, with a maximum daily dose of 2,000 mg. This slow increase can help minimize common gastrointestinal issues like diarrhea and stomach discomfort. On the other hand, your spironolactone dosage will be tailored to your specific response by your healthcare provider.
Timing and Proper Use of Your Medications
Once your dosage is set, follow these tips for taking your medications effectively:
- Metformin ER: Take it with your evening meal to ease stomach upset. Swallow the tablet whole with water - don’t crush, chew, or break it, as this could interfere with its extended-release mechanism.
- Spironolactone: Take it at the same time every day. You can take it with or without food, but consistency is key. As Mayo Clinic explains:
"You may take this medicine [spironolactone] with or without food, but it should be taken the same way (with or without food) each day." – Mayo Clinic
Keep Track of Your Doses
To stay on top of your medications, consider using a tracker app or a calendar to log your daily doses and monitor any side effects. If you miss a dose of metformin, simply skip it and continue with your regular schedule - don’t take extra to make up for it. For spironolactone, take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed dose and return to your usual routine. Always avoid doubling up on doses.
sbb-itb-6dba428
Tracking Your Progress
Schedule Follow-Up Lab Work
Your healthcare provider will keep a close eye on how your body adjusts to metformin and spironolactone through regular blood tests. About a week after starting or adjusting your dose, you'll undergo lab work to check key indicators like serum creatinine, eGFR (a measure of kidney function), urea, electrolytes, and your blood pressure. Once your treatment stabilizes, these tests typically occur every three to six months.
| Monitoring Phase | Frequency | Required Tests |
|---|---|---|
| Initial Start/Dose Change | After 1 week | Serum creatinine, eGFR, Urea, Electrolytes, Blood Pressure |
| First 3 Months | Monthly | Serum creatinine, eGFR, Urea, Electrolytes |
| Ongoing (Stable) | Every 3–6 months | Serum creatinine, eGFR, Urea, Electrolytes |
By sticking to this schedule, you can stay informed about how your body is responding to the treatment. Pay attention to your symptoms and progress as part of this ongoing monitoring.
What to Expect and When
You might notice improvements in insulin sensitivity within a few months, while visible changes like reduced hair growth typically take about three to six months. During this time, your menstrual cycles may also become more regular. Keeping a journal or using a tracking app can help you log these changes, making it easier to provide detailed updates during follow-ups.
Know What to Watch For
In addition to regular lab work, keep an eye on specific test results and notify your healthcare provider if anything seems off. For example:
- If your potassium level exceeds 5.5 mmol/L, your provider may lower your dose.
- If potassium levels rise above 6.0 mmol/L, stop the medication immediately and seek specialist advice.
- Be cautious if your eGFR drops below 30 mL/min/1.73m² or if your creatinine level climbs above 2.5 mg/dL (approximately 220 µmol/L), as these could require a dosage adjustment.
Also, report any severe diarrhea, vomiting, or signs of infection right away. These symptoms can affect kidney function and potassium levels, so quick action is essential. Regular communication with your provider ensures you stay on track while minimizing potential risks.
Handling Side Effects
As you track your progress, it's important to address and manage any side effects that may arise.
Common Side Effects and How to Manage Them
Many people experience mild, temporary side effects. For example, metformin can cause mild stomach issues, particularly at the start of treatment. To ease this, take metformin ER with your evening meal, as this can help reduce stomach discomfort. The extended-release version of the medication is often gentler on the stomach.
Spironolactone, on the other hand, may lead to symptoms like breast tenderness, changes in your menstrual cycle, headaches, or increased urination . To minimize nighttime trips to the bathroom, take spironolactone earlier in the day. You might also feel dizzy or lightheaded when standing up quickly - try sitting for a moment before standing to avoid fainting. If you’re unsure how the medication affects you, avoid driving until you feel confident. Staying hydrated is key, and unless your doctor advises otherwise, steer clear of potassium supplements since spironolactone can raise potassium levels . Be consistent with how and when you take your medication each day.
While these side effects are common, keep an eye out for more serious symptoms that might require immediate medical attention.
Warning Signs to Watch For
Safe treatment depends on recognizing potential problems early. Be alert for symptoms of hyperkalemia (high potassium levels), such as muscle weakness, irregular heartbeat, confusion, trouble breathing, or numbness and tingling in your hands or feet .
"Hyperkalemia (high potassium in the blood) may occur while you are using this medicine. Check with your doctor right away if you have the following symptoms: stomach pain, confusion, difficulty with breathing, irregular heartbeat, nausea or vomiting, nervousness, numbness or tingling in the hands, feet, or lips, or weakness or heaviness of the legs." - Mayo Clinic
Additionally, seek immediate medical help if you notice signs of internal bleeding or problems with your liver or kidneys. These warning signs include bloody or black, tarry stools; vomiting blood or material resembling coffee grounds; yellowing of your skin or eyes; dark urine; clay-colored stools; or a sharp decrease in urine output . Allergic reactions, such as hives, facial swelling, or difficulty breathing, also require urgent care .
When to Contact Your Provider
Reach out to your healthcare provider immediately if you experience severe or ongoing vomiting, diarrhea, fainting, or seizures .
For less urgent issues, like mild breast tenderness, minor headaches, or questions about your medication schedule, you can wait until regular office hours or your next follow-up appointment. If you’re unsure whether a symptom is serious, don’t hesitate to call your provider for guidance. Regular communication with your healthcare team ensures your treatment plan stays on track and adjustments are made when needed.
Next Steps
With your treatment plan underway, it's important to stay focused on the following steps to ensure progress and success.
Stick with your treatment for at least six months. Studies show that the best metabolic improvements often appear after six months of consistent therapy. For example, in a study of 204 women, 82.8% (169 participants) who completed the full six-month treatment experienced better menstrual regularity, improved testosterone levels, and healthier metabolic markers.
Schedule regular follow-ups every three to six months to review lab results and fine-tune your treatment plan as needed. Regular check-ins are essential for effectively managing PCOS, as highlighted earlier. If in-person visits are difficult to arrange, telehealth services like Oana Health provide easy access to licensed professionals who specialize in PCOS care. They even offer 24/7 support via online or phone consultations.
If you've been keeping track of symptoms and side effects, continue sharing these details with your healthcare provider during each visit. This information is invaluable for evaluating how well your treatment is working and making any necessary adjustments to your medications.
To avoid gaps in your medication routine, consider using automatic refill services. Sticking to a consistent daily schedule is key to achieving the best possible results, as missed doses can hinder your progress. For instance, Oana Health's Metformin & Spironolactone pack starts at $32 per month, includes free shipping, and offers automatic refills - making it easier to stay on track.
Managing PCOS is a long-term journey. Continue practicing the lifestyle habits and medication routines you've developed, and don't hesitate to reach out to your healthcare team with any questions or concerns. By staying consistent with your medications, attending regular check-ups, and seeking ongoing support, you're paving the way for lasting improvements in your PCOS symptoms.
FAQs
How do metformin and spironolactone work together to manage PCOS symptoms?
Metformin and spironolactone are frequently prescribed together to target two major aspects of PCOS: insulin resistance and excess androgens. Using both medications offers a more well-rounded approach to symptom management.
Metformin helps your body handle insulin more efficiently, which lowers insulin levels and decreases the ovaries' production of male hormones like testosterone. This can lead to better hormone balance, more regular menstrual cycles, and even some support for modest weight loss. Meanwhile, spironolactone works by blocking male hormones from attaching to receptors, helping to reduce issues like acne, unwanted facial hair, and hair thinning.
When combined, these medications tackle both the underlying metabolic issue (insulin resistance) and the hormonal imbalances (androgens), making them more effective at improving PCOS symptoms than if used individually.
What lifestyle adjustments should I make when starting metformin and spironolactone?
When starting metformin and spironolactone, a few thoughtful lifestyle adjustments can go a long way in boosting the effectiveness of your treatment while promoting better overall health.
Start by focusing on a balanced diet. Incorporate whole grains, lean proteins, vegetables, and healthy fats into your meals. At the same time, try to cut back on processed carbs and refined sugars. This approach can help improve insulin sensitivity and reduce potential side effects from the medication.
Adding regular exercise to your routine is another key step. Aim for 150 minutes of moderate aerobic activity per week, like brisk walking or cycling, and include some strength training sessions. This combination not only supports weight management but also helps maintain hormonal balance.
Hydration is crucial too. Drink plenty of water throughout the day and try to limit alcohol consumption. This helps protect your kidneys and prevents fluctuations in blood sugar levels. To avoid stomach upset, take metformin with meals, and be sure to keep track of your blood glucose and potassium levels as advised by your healthcare provider.
Lastly, don’t underestimate the power of quality sleep and stress management. Both are essential for improving insulin sensitivity and maintaining hormonal health. By making these changes, you’ll not only enhance the benefits of your treatment but also support your overall well-being.
What symptoms should I watch for that may require immediate medical attention while taking metformin and spironolactone?
If you're taking metformin and spironolactone, it’s crucial to stay alert for symptoms that might require immediate medical attention.
For spironolactone, keep an eye out for:
- Severe muscle weakness
- Irregular heartbeat
- Numbness or tingling (which could indicate high potassium levels)
- Sudden swelling or reduced urine output
- Extreme fatigue (potential kidney issues)
Also, seek help right away if you notice rashes, swelling in the face, difficulty breathing (possible allergic reactions), blood in your urine, or sudden dizziness, fainting, or heart palpitations.
When it comes to metformin, while emergency signs might not always be clearly outlined, reach out to a healthcare provider or head to an emergency room if you experience:
- Unexplained muscle pain
- Difficulty breathing
- Intense stomach pain
- Sudden weakness
- Feeling unusually cold
If any of these symptoms occur, don’t hesitate - call 911 or go to the nearest emergency room immediately.
