Collagen and PCOS: Benefits for Skin and Hormonal Balance
Struggling with PCOS-related skin issues or hormonal imbalances? Collagen might help. While not a cure, collagen supports skin repair, improves hydration, and may indirectly aid in managing PCOS symptoms like acne and insulin resistance.
Key Takeaways:
- PCOS often causes hormonal acne, oily skin, and inflammation.
- Collagen helps repair skin, boosts elasticity, and reduces scarring.
- Glycine in collagen supports liver health and hormone metabolism.
- Consistent use (8–12 weeks) of hydrolyzed collagen (2.5–10g daily) shows results.
- Best paired with a low-glycemic diet, exercise, and medical treatments for deeper hormonal issues.
Collagen is one piece of a larger PCOS management plan. Combine it with lifestyle changes and professional care for the best results.
PCOS and Its Effects on Skin and Hormones
What PCOS Does to Your Hormones
PCOS, or polycystic ovary syndrome, disrupts the body's hormonal balance. It affects between 5% and 26% of women of reproductive age globally, making it the most common endocrine condition in this group.
At the heart of PCOS is an excess of androgens - hormones like testosterone and androstenedione. In women with PCOS, the ovaries and adrenal glands produce unusually high levels of these hormones. In fact, up to 80% of women with hyperandrogenism are eventually diagnosed with PCOS. This hormonal imbalance interferes with the development of ovarian follicles, often leading to irregular or absent ovulation.
Another major issue is insulin resistance, which affects about 70% of women with PCOS, regardless of their weight. When cells become resistant to insulin, the body compensates by producing more of it. High insulin levels, in turn, stimulate the production of androgens while reducing levels of Sex Hormone Binding Globulin (SHBG), which increases free testosterone levels. This creates a cycle that worsens insulin resistance.
The hormonal disruption also extends to the hypothalamic-pituitary-ovarian axis. Increased pulses of Gonadotropin-Releasing Hormone (GnRH) lead the pituitary gland to release more Luteinizing Hormone (LH) compared to Follicle-Stimulating Hormone (FSH). This imbalance further boosts androgen production. Additionally, chronic inflammation - often marked by elevated C-reactive protein (CRP) levels - adds another layer of metabolic challenges.
How PCOS Affects Your Skin
The hormonal imbalances caused by PCOS don’t just affect internal systems - they also have a noticeable impact on skin health. Elevated androgen levels enlarge sebaceous glands, leading to increased sebum production and changes in how skin cells shed. This combination often results in clogged pores and acne.
The acne linked to PCOS is typically deep, large, and slow to heal. It commonly appears along the lower face, including the jawline, chin, and upper neck, but it may also affect the chest and back. About 30% to 40% of women with PCOS experience this type of acne, and adolescents with severe or stubborn acne have a 40% likelihood of having undiagnosed PCOS.
"PCOS-related acne often flares on the lower face, including the jawline, chin, and upper neck... Women with PCOS may notice that acne lesions are deeper, larger, and slower to resolve." – Kristina Liu, MD, MHS, and Janelle Nassim, MD, Harvard Health Publishing
High insulin levels contribute to additional skin changes. For instance, they can lead to acanthosis nigricans - dark, thickened, velvety patches of skin that usually appear in body folds like the neck, armpits, and groin. Persistent inflammation tied to PCOS further exacerbates skin issues, making lesions harder to heal and prolonging the skin's recovery process.
How Collagen Works for PCOS
Collagen Types and How They Work
Collagen is the body's most abundant protein, forming the backbone of skin, muscles, bones, and connective tissues. Its unique structure plays a key role in maintaining these functions.
Among the various types, Type I collagen is particularly important for skin health. It accounts for about 90% of the body's collagen, contributing to structure, firmness, and elasticity, and making up roughly 80% of the skin's dry weight. Type III collagen supports muscles and organs, while Type V collagen is essential for maintaining healthy hair and skin layers.
These types of collagen set the stage for their well-documented benefits in improving skin repair and hydration.
"Hydrolyzed collagen (HC) is the most popular and promising skin anti-aging nutraceutical." – Szu-Yu Pu et al., Nutrients Journal
Collagen's Benefits for Skin
Studies show that collagen supplements can have a noticeable impact on skin health. A meta-analysis of 26 randomized controlled trials, involving 1,721 participants, found that hydrolyzed collagen significantly improves skin hydration and elasticity. For women with PCOS, who often deal with hormonal acne, collagen can support the skin’s natural repair process and help heal acne scars.
Results take time, though - consistent collagen use typically shows significant improvements in skin hydration and elasticity after 8 to 12 weeks. Among the available options, marine collagen stands out for its superior bioavailability.
But collagen's benefits don't stop at skin repair. Its effects extend to broader systems in the body that play a role in PCOS management.
Does Collagen Affect Hormone Levels?
Collagen doesn’t directly regulate hormones like insulin or estrogen, but it plays a supportive role in systems that influence hormonal balance. One of its key components, glycine, helps boost glutathione production - a critical antioxidant. Glutathione deficiency has been linked to oxidative stress and elevated testosterone levels in PCOS.
Glycine also aids liver function, which is essential for metabolizing and clearing excess estrogen from the body. Additionally, collagen strengthens the lining of the digestive tract, promoting gut health - a crucial factor in hormone metabolism and reducing inflammation, a frequent issue in PCOS. Together, these effects support broader hormonal stability.
Emerging research also hints that hydrolyzed collagen might improve insulin sensitivity and help stabilize blood sugar levels. This could be especially beneficial for the estimated 44% to 70% of women with PCOS who face insulin resistance. However, it’s worth noting that these effects are indirect rather than a primary action of collagen.
Using Collagen Safely for PCOS and Acne
Dosage, Forms, and When to Take It
For women managing PCOS, taking 2.5 to 10 grams of hydrolyzed collagen daily has been shown to improve skin health. Clinical studies suggest these doses are safe for up to six months, with visible results typically appearing after at least three months of consistent use. Some recommendations suggest aiming for 8 grams of collagen for every 15 grams of total protein intake.
Hydrolyzed collagen, also called collagen peptides, is favored for its better absorption. When choosing a supplement, look for Type I and Type III collagen, as Type I makes up 80–90% of your skin's structure. Marine collagen, derived from fish, is particularly effective due to its superior absorption rate.
Quality matters. Opt for supplements that have been third-party tested by organizations like NSF International, USP, or ConsumerLab to ensure they are free from heavy metals and contaminants. Pairing collagen with vitamin C–rich foods - such as citrus fruits, berries, or bell peppers - can further enhance your body’s ability to synthesize collagen.
"Taking hydrolyzed collagen doses ranging from 2.5-15 grams (g) for up to 12 weeks may be safe and beneficial."
– Lindsey DeSoto, RD
Next, let’s look at situations where collagen use might not be suitable.
When to Avoid or Limit Collagen
If you have seafood allergies, be cautious with marine collagen, as it is derived from fish or shellfish. Similarly, avoid collagen sourced from bovine, chicken, or eggshells if you have sensitivities to these ingredients.
For those with kidney disease or who follow a protein-restricted diet, consult your doctor before adding collagen to your routine. Since collagen is a protein supplement, it could impact your dietary limits. Mild side effects like bloating, heartburn, or a lingering aftertaste are also possible for some individuals.
Pregnant or breastfeeding women should avoid collagen supplements due to insufficient safety data. Additionally, because PCOS involves complex hormonal changes, it’s essential to monitor any shifts in your menstrual cycle and discuss them with your healthcare provider.
Combining Collagen with Other PCOS Treatments
While collagen can support healthier skin, it works best when paired with appropriate medical care. For severe hormonal acne or insulin resistance, targeted treatments are key. For instance, Oana Health offers personalized telehealth services for PCOS, including prescription options like topical Spironolactone for hormonal acne (starting at $43.00/month) and insulin sensitizers (around $199.00/month). Their licensed professionals develop tailored treatment plans to address the root causes of PCOS symptoms, with medications delivered to your doorstep.
"There is no scientific evidence showing the benefits of collagen for PCOS hair loss or acne. While collagen plays a significant role in our skin, hair, and nails, taking supplements may not be the cure-all that some companies claim."
– Letisha Hodges, Registered Dietitian
Always consult your healthcare provider before starting collagen supplements, especially if you’re already taking medications like Metformin or Spironolactone, to ensure there are no interactions.
sbb-itb-6dba428
The Collagen Hack That Changed My PCOS Journey!
Creating a Complete Plan for Skin and Hormone Health
Collagen Benefits and Limitations for PCOS Skin Health
Other Treatments for Hormonal Acne
For women with PCOS, hormonal acne is a common challenge - 30–40% experience acne, while 70% deal with insulin resistance, which drives androgen excess. While collagen can aid skin health, it won’t solve these deeper hormonal issues on its own. A well-rounded approach is necessary to manage hormonal acne effectively, combining collagen with other strategies.
Dietary changes are a key starting point. A low-glycemic or Mediterranean diet can help stabilize blood sugar levels and reduce sebum production. Focus on including proteins, fiber, and healthy fats in your meals while cutting back on dairy, which can increase IGF-1 levels.
Targeted supplements can support these dietary adjustments. Myo-inositol improves insulin signaling, zinc helps regulate sebum and promotes healing, omega-3 fatty acids (2,000 mg daily) can reduce inflammation and acne, and spearmint tea has been shown to lower free testosterone levels.
Medical treatments may be necessary for more severe cases. Topical retinoids can unclog pores, while benzoyl peroxide and salicylic acid help reduce inflammation. For hormonal acne that doesn’t respond to lifestyle changes, Oana Health offers telehealth consultations with licensed professionals. They can prescribe treatments like topical Spironolactone (starting at $43.00/month) or insulin-sensitizing medications such as oral Metformin ER ($22.00/month) and oral GLP-1 & Metformin ($199.00/month), delivered directly to your door.
"Acne and polycystic ovary syndrome are related to what's happening within your body, which is why a comprehensive approach to address the underlying imbalances... is the best approach."
– Dr. Jolene Brighten, NMD
Lifestyle adjustments also play a big role. Losing just 5% of body weight can help restore ovulation. Strength training and stress management techniques, like yoga or meditation, can further improve insulin sensitivity and reduce androgen levels.
By combining these interventions with collagen supplementation, you can create a more effective plan for improving both skin health and hormonal balance.
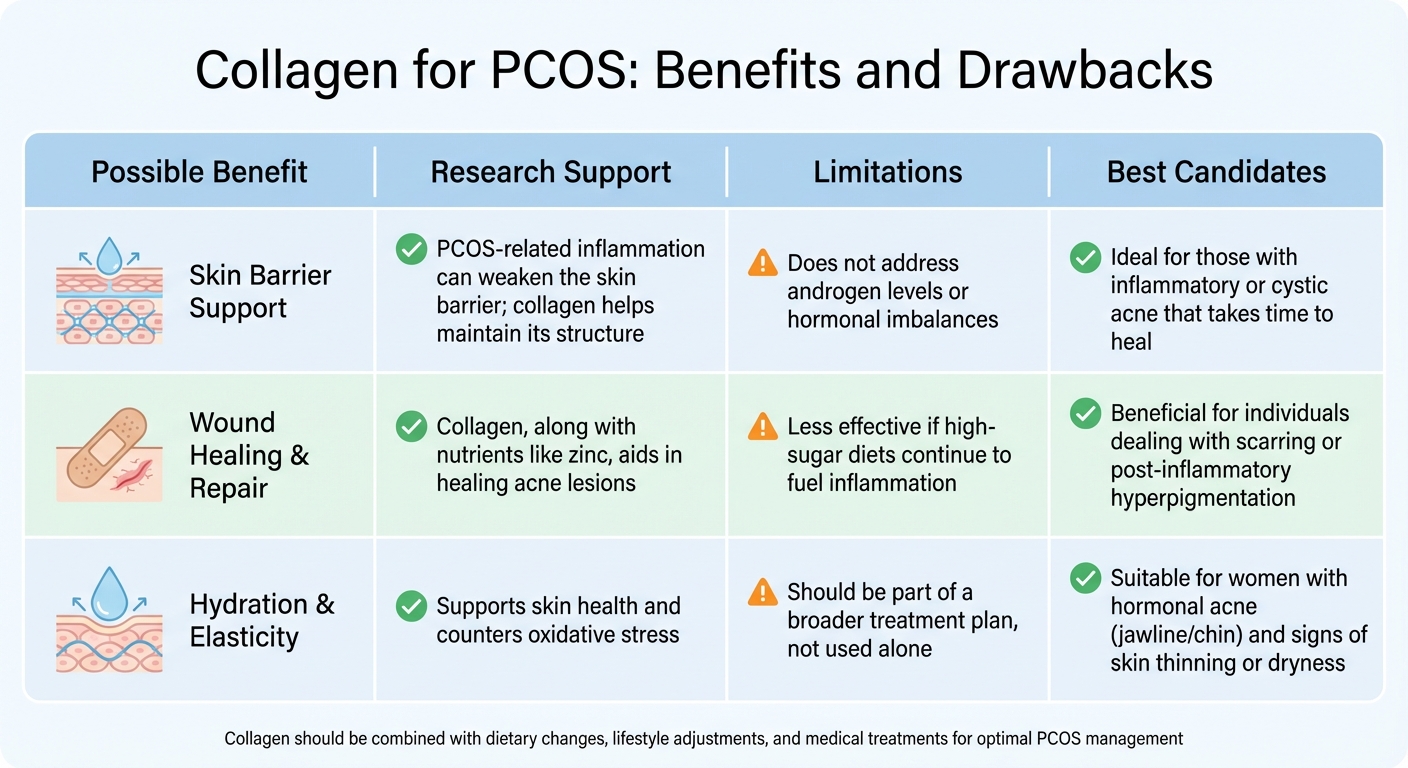
Collagen for PCOS: Benefits and Drawbacks
While collagen isn’t a direct solution for hormonal imbalances, it offers supportive benefits for skin health. Here’s how collagen stacks up against other interventions:
| Possible Benefit | Research Support | Limitations | Best Candidates |
|---|---|---|---|
| Skin Barrier Support | PCOS-related inflammation can weaken the skin barrier; collagen helps maintain its structure. | Does not address androgen levels or hormonal imbalances. | Ideal for those with inflammatory or cystic acne that takes time to heal. |
| Wound Healing & Repair | Collagen, along with nutrients like zinc, aids in healing acne lesions. | Less effective if high-sugar diets continue to fuel inflammation. | Beneficial for individuals dealing with scarring or post-inflammatory hyperpigmentation. |
| Hydration & Elasticity | Supports skin health and counters oxidative stress. | Should be part of a broader treatment plan, not used alone. | Suitable for women with hormonal acne (jawline/chin) and signs of skin thinning or dryness. |
"Understanding the pathophysiology of PCOS-related skin conditions is crucial for implementing a holistic, integrative treatment strategy that addresses the root causes of dysfunction rather than merely managing symptoms."
– Galina Mironova, ND
While collagen can help repair the skin barrier and improve hydration, it doesn’t address the root causes of hormonal acne. To see real progress, collagen should be paired with dietary changes, lifestyle adjustments, and medical treatments that target insulin resistance and androgen excess. This combined approach ensures that your skin and hormones are supported from every angle.
Conclusion
Collagen supplements can play a helpful role for women with PCOS, particularly in supporting skin health. By strengthening the skin's moisture barrier, collagen helps improve hydration, while its ability to stimulate fibroblast activity aids in healing acne lesions and reducing scars. Many women dealing with hormonal acne may find that better hydration and skin repair lead to noticeable improvements in texture and reduced scarring.
That said, collagen is not a standalone solution for managing PCOS. While it might provide indirect benefits, such as potentially improving insulin sensitivity and lowering inflammation, it doesn’t directly address elevated androgen levels or insulin resistance. Instead, collagen should be seen as a complementary tool within a larger treatment plan. As Dr. Jolene Brighten, a Naturopathic Endocrinologist, explains:
"Skincare can be considered the finishing touch if you think of hormone balance as the foundation for your PCOS care".
To see visible results, consistent daily collagen intake - around 8 grams within a 15-gram protein serving - is recommended for 8–12 weeks. Pairing collagen with a low-glycemic diet, regular exercise, and nutrients like vitamin C and zinc can further enhance its benefits.
For more stubborn symptoms, consulting healthcare providers is key. If hormonal acne or other PCOS-related issues persist, professional guidance can help. Platforms like Oana Health offer telehealth consultations with licensed experts who can prescribe targeted treatments, such as topical Spironolactone (US$43/month) or oral Metformin ER (US$22/month), delivered to your doorstep.
FAQs
Can collagen help with acne caused by PCOS?
Collagen may play a role in improving acne linked to PCOS. By enhancing insulin sensitivity and helping to lower androgen levels - two common concerns for women with PCOS - it can address key factors that contribute to acne, such as excess oil production and inflammation.
On top of that, collagen supports skin elasticity and aids in repair, which can enhance the texture and overall look of your skin. Including collagen in your routine could work well alongside other treatments designed to manage PCOS symptoms.
Can collagen help with insulin resistance in women with PCOS?
Emerging studies indicate that collagen supplements might play a role in improving insulin sensitivity for women with PCOS. This improvement in blood sugar regulation could potentially help address insulin resistance, a frequent challenge for those living with PCOS.
Although further research is necessary to fully understand its impact, collagen's potential benefits for metabolic health make it an intriguing option to consider as part of a PCOS management plan. Be sure to consult a healthcare professional before introducing any new supplement to your routine.
What foods should I eat with collagen to help manage PCOS symptoms?
Pairing collagen with a well-rounded, PCOS-friendly diet can amplify its benefits for both hormonal balance and skin health. A Mediterranean-style eating plan is a great choice. It focuses on lean proteins, fiber, healthy fats, and antioxidant-packed fruits and vegetables. This combination not only supports collagen production but also helps lower inflammation and improves insulin sensitivity - an essential part of managing PCOS symptoms.
To get the most out of this approach, include collagen-rich foods like bone broth, fish, chicken, and eggs. Pair these with vitamin C-rich options such as citrus fruits, berries, or kiwi to help your body absorb collagen more effectively. On the flip side, try to limit refined carbs, sugary drinks, and excess dairy, as they can cause insulin spikes and potentially worsen symptoms. Aiming for a protein intake of about 1.2–1.5 grams per kilogram of body weight can further promote hormone balance.
Here are some practical tips: mix collagen powder into your morning coffee or a smoothie, fill half your plate with non-starchy vegetables, add a serving of lean protein, and round it out with healthy fats like olive oil or a handful of nuts. Staying hydrated and eating every 3–4 hours can also help stabilize blood sugar levels. For a more personalized approach to managing PCOS, Oana Health provides tailored telehealth solutions that can be accessed right from the comfort of your home.
