Cortisol and PCOS: Impact on Insulin Resistance
Cortisol plays a major role in insulin resistance for women with PCOS. This stress hormone disrupts glucose absorption, worsens inflammation, and promotes visceral fat accumulation, all of which aggravate metabolic issues. Women with PCOS often experience higher cortisol levels due to an exaggerated stress response, creating a harmful cycle of hormonal imbalance and insulin resistance.
Key Points:
- PCOS and Insulin Resistance: Affects 35–80% of women with PCOS, increasing the risk of Type 2 diabetes by 5–10 times.
- Cortisol's Role: Chronic stress elevates cortisol, leading to higher blood sugar, disrupted insulin signaling, and abdominal fat buildup.
- Treatment Options: Medications like Metformin, GLP-1 receptor agonists, and Pioglitazone can help. Lifestyle changes, including stress management, dietary adjustments, and moderate exercise, are equally important.
Breaking this cycle requires addressing both cortisol imbalance and insulin resistance through targeted medications, stress reduction, and personalized care.
Cortisol and PCOS Connection
How High Cortisol Worsens Insulin Resistance in PCOS
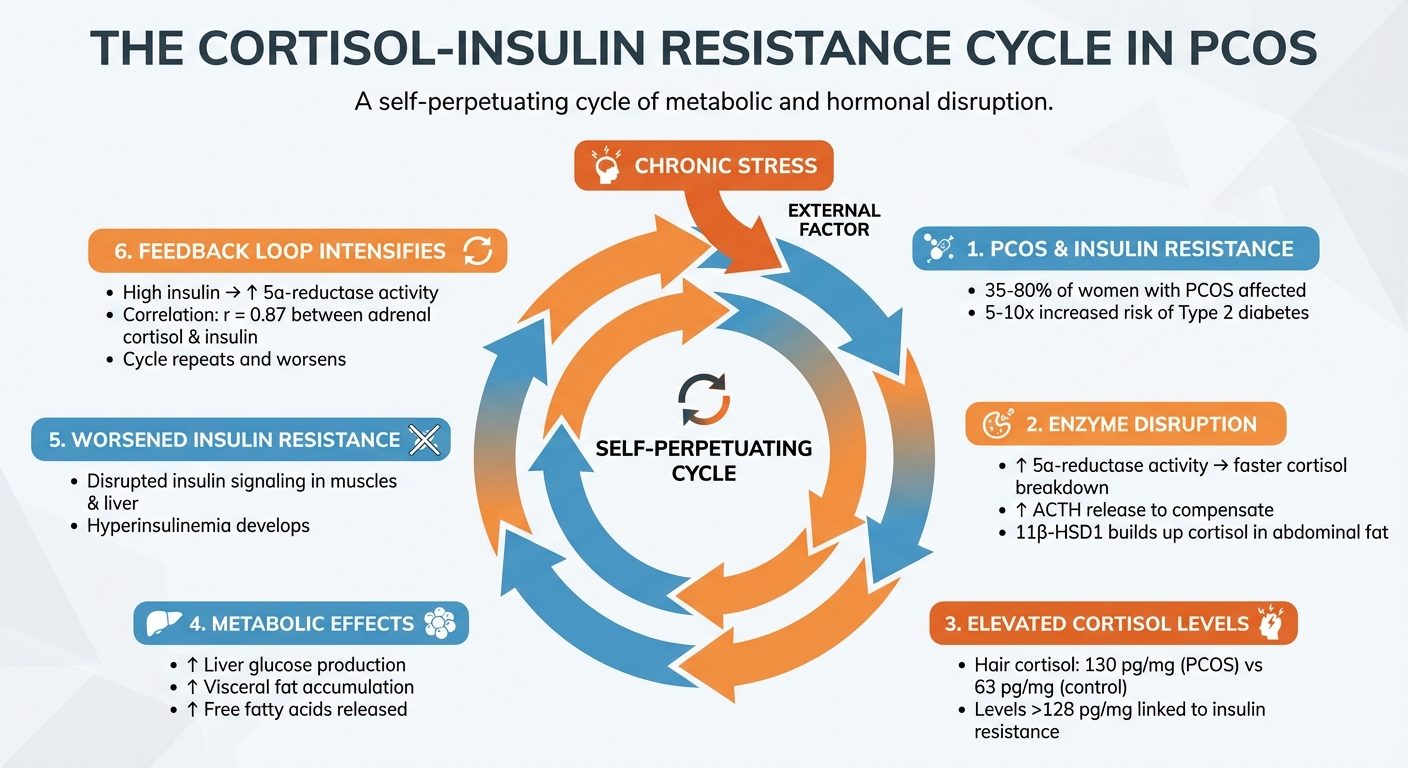
The Cortisol-Insulin Resistance Cycle in PCOS
Enzyme Problems in Cortisol Production
For women with PCOS, enzyme irregularities can significantly disrupt cortisol metabolism. One key issue is an increase in 5α‐reductase activity, which speeds up cortisol breakdown. To compensate, the body releases more ACTH (adrenocorticotropic hormone) to maintain cortisol levels. This overcompensation can lead to excessive production of both cortisol and adrenal androgens. Additionally, altered activity of the enzyme 11β‐HSD1 causes cortisol to build up locally in abdominal fat, further decreasing insulin sensitivity. These enzyme-related disruptions play a direct role in the hormonal imbalances often seen in PCOS, creating a cycle that feeds into itself and exacerbates the condition.
The Feedback Loop Between Cortisol and Insulin Resistance
In PCOS, insulin resistance and cortisol imbalance fuel each other in a damaging cycle. High insulin levels (hyperinsulinemia) can increase 5α‐reductase activity and intensify the adrenal response, which speeds up cortisol clearance and triggers excessive ACTH release. This feedback loop worsens both cortisol dysregulation and insulin resistance. Studies have shown a strong link between adrenal vein cortisol levels and insulin concentrations in obese, hyperandrogenic women (r = 0.87). Elevated cortisol also drives liver glucose production by activating enzymes like phosphoenolpyruvate carboxykinase and promotes fat breakdown in adipose tissue. This releases free fatty acids, which disrupt insulin signaling in both muscles and the liver. Chronic stress adds fuel to the fire, worsening these metabolic disturbances.
How Chronic Stress Raises Cortisol Levels
Chronic stress keeps the HPA (hypothalamic-pituitary-adrenal) axis in overdrive, leading to persistently high cortisol levels. Women with PCOS often have significantly higher hair cortisol levels - around 130 pg/mg compared to 63 pg/mg in those without PCOS. Notably, cortisol levels exceeding 128 pg/mg are strongly associated with insulin resistance. This prolonged cortisol elevation encourages visceral fat accumulation, as visceral fat contains more glucocorticoid receptors than subcutaneous fat, making it more responsive to cortisol's effects.
Cortisol's Effect on Inflammation and Metabolism
Inflammation and Reduced Cortisol Response
When cortisol levels stay high over a prolonged period, the body can develop glucocorticoid resistance. This means tissues stop responding to cortisol's natural ability to reduce inflammation. In women with PCOS, chronic inflammation leads to the production of an inactive receptor, GRβ, which blocks the function of the active GRα receptor. Kristen Farrell from the University of Miami explains:
"In this state [glucocorticoid resistance], glucocorticoids are no longer able to suppress the production of pro-inflammatory markers."
As a result, cortisol loses its ability to control inflammation, creating a persistent low-grade inflammatory state. This ongoing inflammation not only worsens insulin resistance but also heightens the metabolic risks tied to visceral fat buildup.
Belly Fat, Inflammation, and Cortisol
Cortisol plays a pivotal role in fat distribution, particularly in promoting abdominal fat accumulation. Visceral fat, which surrounds internal organs, has significantly more glucocorticoid receptors than subcutaneous fat (the fat just beneath the skin). This makes visceral fat highly responsive to cortisol's actions. Unfortunately, this type of fat releases inflammatory molecules like IL-6 and TNF-α, which further aggravate insulin resistance across the body.
Adding to the issue, the enzyme 11β-HSD1 in abdominal fat converts inactive cortisone into active cortisol, intensifying local exposure. Even if blood cortisol levels seem normal, this localized conversion creates a concentrated cortisol effect in the abdominal area. Studies have found that cortisol production is strongly linked to intra-abdominal fat levels but not to subcutaneous fat. For women with PCOS, this visceral fat accumulation significantly raises the risk of progressing from impaired glucose tolerance to type 2 diabetes - by as much as 5 to 10 times compared to women without PCOS.
| Feature | Visceral Fat (Belly Fat) | Subcutaneous Fat |
|---|---|---|
| Cortisol Sensitivity | Higher expression of glucocorticoid receptors | Lower expression of glucocorticoid receptors |
| Inflammatory Impact | High; releases cytokines like IL-6 and TNF-α | Lower inflammatory activity |
| Metabolic Risk | Strongly linked to insulin resistance and liver fat | Moderate metabolic impact |
sbb-itb-6dba428
Treatment Options for Cortisol and Insulin Problems in PCOS
Medications for Insulin Sensitivity
When it comes to addressing insulin resistance in PCOS, Metformin is often the go-to medication. It helps improve menstrual cycles and reproductive outcomes while reducing high insulin levels. However, its impact on adrenal cortisol pathways has shown mixed results in various studies.
Pioglitazone, a thiazolidinedione, works differently by lowering circulating insulin levels and potentially improving adrenal steroidogenesis. Renato Pasquali, from the Division of Endocrinology at University Alma Mater Studiorum, explains:
"The decrease of circulating insulin may improve adrenal steroidogenesis, possibly through a regulation of peripheral cortisol metabolism, rather than affecting cortisol production rate from the adrenals."
This medication specifically influences the allotetrahydrocortisol/tetrahydrocortisol ratio.
For women dealing with severe insulin resistance and cortisol-related weight gain, GLP-1 receptor agonists, such as Semaglutide, offer a newer option. These medications target metabolic dysfunction and weight issues, which can worsen HPA axis imbalances. Clinical guidelines highlight that insulin-sensitizing medications should take priority in PCOS treatment, as antiandrogens do not address the root cause of insulin resistance.
| Medication | Primary Use in PCOS | Effect on Cortisol/Adrenal Pathways |
|---|---|---|
| Metformin | Insulin sensitivity, ovulation | Mixed results; some studies suggest no direct effect on adrenal enzymes |
| Pioglitazone | Insulin sensitivity | May support adrenal steroidogenesis via peripheral cortisol regulation |
| GLP-1 Agonists | Insulin sensitivity, weight control | Helps manage metabolic effects of high cortisol levels |
| Antiandrogens | Hyperandrogenism symptoms | Does not address insulin resistance |
In addition to medications, lifestyle changes play a key role in managing cortisol and insulin imbalances.
Lifestyle Changes and Stress Reduction
Dietary adjustments are essential for managing both insulin resistance and cortisol levels. Opt for low-glycemic foods like beans, berries, and non-starchy vegetables to keep blood sugar stable and ease the demand on insulin. Adding anti-inflammatory options - such as olive oil, leafy greens, and nuts - can help reduce chronic inflammation. Even a small weight loss of 5% of body weight can lead to noticeable improvements in PCOS symptoms.
Stress management techniques are equally important for lowering cortisol levels. Practices like deep breathing, mindfulness meditation, and yoga activate the body's relaxation response. Sleep is another critical factor since women with PCOS experience sleep disturbances twice as often as others. Aim for 7–9 hours of quality sleep and minimize screen time before bed.
When it comes to exercise, it's important to strike the right balance. Moderate-intensity activities such as walking, swimming, Pilates, and strength training can improve insulin sensitivity. On the other hand, overly intense cardio sessions may increase cortisol levels. Incorporating magnesium-rich foods like pumpkin seeds, spinach, and dark chocolate can also support stress management naturally.
Experts recommend starting with lifestyle counseling - focusing on weight loss, exercise, and reducing smoking or alcohol consumption - before turning to medications. This approach takes into account the heightened cortisol responses to stress often seen in women with PCOS, making stress reduction a critical part of treatment.
Oana Health's Personalized PCOS Treatment
Oana Health offers telehealth services that address the complex interplay between cortisol dysregulation and insulin resistance in PCOS. Their clinicians specialize in creating phenotype-based treatment plans tailored to each individual's hormonal profile. Using comprehensive lab tests, such as DHEAS and fasting insulin, they identify the most effective strategies for each patient.
Oana Health provides access to evidence-based medications, including:
- Metformin (starting at $22/month)
- GLP-1 receptor agonists like Semaglutide ($199/month)
- Spironolactone ($14/month)
- Metformin & Spironolactone combination pack ($32/month)
For patients with stress-related or adrenal-driven PCOS, hormonal contraceptives may be prescribed to help balance the feedback loop between cortisol and androgens. All prescriptions are provided by licensed medical professionals and shipped directly to patients' homes with free delivery.
Conclusion: Addressing Cortisol to Improve Insulin Resistance
Managing cortisol effectively plays a crucial role in breaking the cycle of insulin resistance in PCOS. Studies indicate that around 70% of women with PCOS are insulin resistant, and they face a 5- to 10-fold greater risk of developing Type 2 diabetes. The relationship between cortisol and insulin creates a feedback loop - elevated insulin levels stimulate androgen production and disrupt cortisol metabolism, which further impairs insulin function. Chronic exposure to cortisol contributes to visceral fat accumulation, increases glucose production in the liver, and inhibits insulin secretion. Research involving 1,071 participants revealed that even within normal physiological ranges, higher serum cortisol levels were strongly linked to reduced insulin secretion. This highlights the possibility that cortisol, even at typical levels, could suppress insulin activity, increasing the risk of diabetes. These findings emphasize the need for treatments that address both hormonal and metabolic disruptions.
Combining medications, lifestyle adjustments, and stress management strategies can help redistribute body fat, lower inflammation, and enhance metabolic health. As Eliza B. Geer, MD, from Mount Sinai Medical Center, explains:
"Cortisol normalization alters adipose tissue distribution, resulting in decreased visceral/total fat and visceral fat/skeletal muscle ratios."
Personalized interventions are key to breaking this cycle. These can range from insulin-sensitizing medications to tailored lifestyle changes and stress reduction techniques. Telehealth platforms like Oana Health offer comprehensive solutions that address both the hormonal and metabolic challenges of PCOS. By targeting HPA axis dysfunction, these approaches help restore hormonal balance and create a path toward long-term metabolic health.
FAQs
How does cortisol influence insulin resistance in women with PCOS?
Cortisol, often referred to as the "stress hormone", plays a significant role in worsening insulin resistance in women with PCOS. It disrupts how the body processes insulin by interfering with insulin signaling in fat tissue. This disruption promotes the breakdown of fat (a process known as lipolysis) and increases the release of free fatty acids into the bloodstream. These changes can intensify the metabolic imbalances frequently associated with PCOS.
High cortisol levels can also impact lipid metabolism, adding another layer of complexity to insulin resistance in women with PCOS. Addressing cortisol levels - whether through stress management, lifestyle adjustments, or medical treatments - can be an important step toward improving insulin sensitivity and supporting overall health.
How can lifestyle changes help manage cortisol and insulin resistance in PCOS?
Managing cortisol effectively can play a key role in addressing insulin resistance and other PCOS symptoms. Chronic stress often leads to elevated cortisol levels, so focusing on stress management, regular physical activity, quality sleep, and balanced eating habits can make a noticeable difference. Practices like mindfulness, meditation, yoga, or deep breathing are great tools to help lower stress hormones and promote hormonal balance. Additionally, aiming for 7–9 hours of restful sleep each night can help regulate cortisol and improve your body's ability to process glucose.
Incorporating moderate exercise into your routine - such as brisk walking, cycling, or strength training - three to five times a week can reduce cortisol spikes, improve insulin sensitivity, and aid in maintaining a healthy weight. Complement this with a nutrient-rich diet that includes whole grains, fiber, lean proteins, and low-glycemic foods. Limiting added sugars and caffeine can also help stabilize blood sugar levels and prevent cortisol from fluctuating.
For those seeking a personalized approach, Oana Health provides telehealth programs that integrate these lifestyle strategies with prescription-based treatments for PCOS, weight management, and hormonal balance - all conveniently delivered to your home. By focusing on stress reduction, sleep, exercise, and nutrition, you can better manage cortisol levels and support your overall metabolic health.
How does managing stress help women with PCOS?
Chronic stress has a way of putting the hypothalamic-pituitary-adrenal (HPA) axis into overdrive, which can throw cortisol levels out of balance. When this happens, it often leads to increased adrenal androgen production and worsens insulin resistance - two major contributors to the metabolic and psychological challenges of PCOS.
Effectively managing stress can play a big role in keeping cortisol levels in check. This, in turn, helps restore hormonal balance and may ease symptoms like weight gain, acne, and mood swings. Techniques such as mindfulness practices, staying active with regular exercise, and prioritizing quality sleep can go a long way in improving the overall well-being of women dealing with PCOS.
