How Endocrine Disruptors Affect Hormonal Health
Endocrine-disrupting chemicals (EDCs) can interfere with your hormones, affecting critical functions like your menstrual cycle and metabolism. Found in everyday items like plastics, cosmetics, and food packaging, these chemicals mimic or block hormones, disrupting your body’s balance. Women, especially those with conditions like PCOS, are particularly vulnerable due to the impact on reproductive and metabolic health.
Key Takeaways:
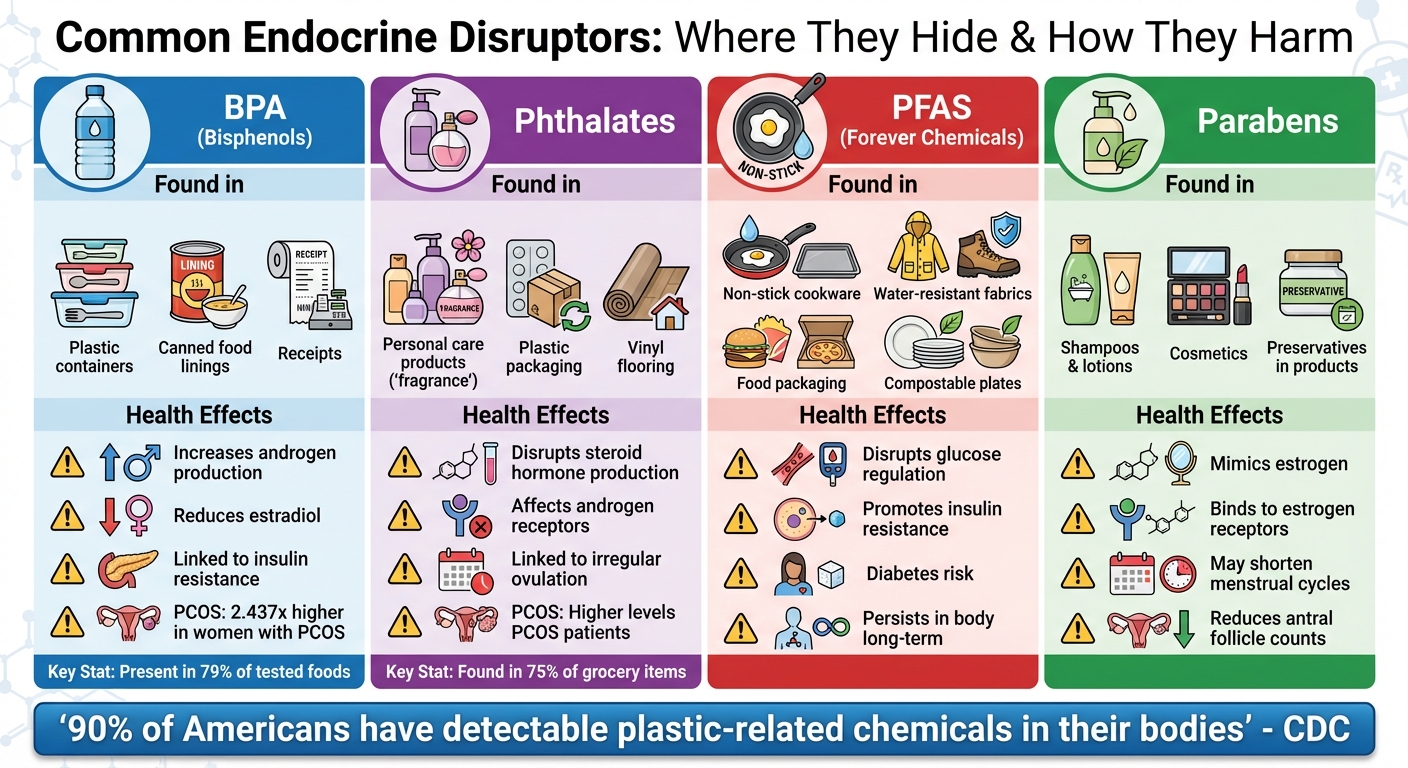
- What are EDCs? Chemicals that disrupt hormone production, transport, or function. Examples include BPA, phthalates, PFAS, and parabens.
- Where are they found? Plastics, canned foods, cosmetics, non-stick cookware, and pesticides.
- Health effects: EDCs can worsen hormonal imbalances, particularly in women with PCOS, by raising androgen levels and promoting insulin resistance.
- Reducing exposure: Avoid microwaving food in plastic, use glass or stainless steel storage, choose fragrance-free and paraben-free personal care products, and filter drinking water.
By reducing daily exposure and combining this with medical treatments if needed, you can better manage hormonal health challenges.
Common Endocrine Disruptors: Sources and Health Effects
How Endocrine Disruptors Affect Female Hormones
How Endocrine Disruption Works
Endocrine-disrupting chemicals (EDCs) interfere with hormones in several ways. They can bind to nuclear hormone receptors, acting like natural hormones, partially activating them, or outright blocking their function. Some EDCs inhibit aromatase (CYP19), the enzyme responsible for converting testosterone into estrogen. Others bind to membrane receptors like GPER1, triggering rapid, non-genomic cellular responses.
Early exposure to EDCs can also leave lasting marks on our DNA by altering methylation patterns or histone modifications. These changes can permanently affect how genes are expressed, potentially influencing not just the individual but also future generations. These molecular disruptions create a ripple effect, upsetting the delicate balance of hormonal regulation.
Effects on the Hypothalamic-Pituitary-Ovarian (HPO) Axis
The HPO axis, which regulates reproductive hormones, is particularly vulnerable to disruption by EDCs. In the hypothalamus, these chemicals can interfere with the kisspeptin system, a key player in controlling the release of Gonadotropin-Releasing Hormone (GnRH). When GnRH signaling falters, the pituitary gland’s hormone production becomes unbalanced, often resulting in increased Luteinizing Hormone (LH) levels and decreased Follicle-Stimulating Hormone (FSH) levels.
This imbalance has a direct impact on ovarian function. Higher LH levels push theca cells to produce excess androgens, while lower FSH levels hinder the conversion of these androgens into estrogens via aromatase. This disruption can lead to premature luteinization and impaired follicle development, ultimately affecting ovulation.
"Deviations from appropriate hormone levels can permanently affect a developing organism in a manner that may set a trajectory for a lifetime of function or dysfunction." - Andrea Gore, Professor and Vacek Chair in Pharmacology
By destabilizing the HPO axis, EDCs not only disrupt ovulation but also contribute to broader issues, including metabolic health challenges.
Connection to Insulin Resistance and Metabolic Problems
Certain EDCs, often referred to as obesogens, can upset energy balance, promoting insulin resistance and metabolic syndrome. This creates a harmful cycle: insulin resistance leads to elevated insulin levels, which then stimulate the ovaries to produce more androgens, worsening symptoms of Polycystic Ovary Syndrome (PCOS).
For women with PCOS, the stakes are high. Around 70% experience insulin resistance, and more than 50% are at risk of developing type 2 diabetes or prediabetes by their early 40s. Persistent organic pollutants (POPs), such as PCBs and DDT, add to the problem. These chemicals, stored in fat tissue, can re-enter the bloodstream during weight loss, further disrupting metabolic processes.
Endocrine Disruptors and PCOS: What Research Shows
Bisphenols (BPA and Related Compounds)
The connection between BPA and PCOS is well-documented. A meta-analysis of nine studies, involving 493 women with PCOS, revealed that these individuals had significantly higher BPA levels compared to those without the condition (standardized mean difference: 2.437). Elevated BPA concentrations have been detected in serum, urine, and even follicular fluid.
BPA interferes with hormone production in several ways. It boosts androgen synthesis in ovarian theca-interstitial cells, reduces estradiol production in granulosa cells, and displaces sex steroids from Sex Hormone Binding Globulin (SHBG). This leads to an increase in free testosterone levels.
"Serum BPA may be positively associated with women with PCOS and BPA might be involved in the insulin-resistance and hyperandrogenism of PCOS." – PubMed, National Library of Medicine
Additionally, studies have found a negative link between BPA levels and ovarian reserve markers, such as Antral Follicle Count (AFC) and Anti-Müllerian Hormone (AMH). Even BPA alternatives like Bisphenol S (BPS) and Bisphenol F (BPF), often marketed in "BPA-free" products, show similar hormonal activity and risks.
Phthalates and Parabens
Beyond BPA, other chemicals like phthalates and parabens also play a role in disrupting hormonal balance in PCOS.
Research shows that women and adolescents with PCOS tend to have higher urinary phthalate levels compared to healthy controls. These chemicals interfere with steroid hormone production and androgen receptors, contributing to symptoms like excessive hair growth and irregular ovulation. Adolescent girls, in particular, are at risk, with studies finding a positive correlation between urinary phthalate levels and polycystic ovary morphology observed on ultrasounds.
Parabens, commonly used as preservatives in personal care products, mimic estrogen by binding to estrogen receptors. While their estrogenic effects are weaker, chronic exposure through everyday items like shampoos and lotions may still disrupt endocrine function. Some studies suggest a link between parabens and shorter menstrual cycles or reduced antral follicle counts. However, their direct connection to PCOS remains less consistent compared to phthalates.
PFAS and Persistent Pollutants
Persistent pollutants add another layer of complexity to the metabolic challenges associated with PCOS, particularly regarding glucose regulation.
Persistent organic pollutants (POPs), such as PCBs, PBDEs, and DDT/DDE, accumulate in white adipose tissue and can enter the bloodstream during weight loss. These substances disrupt metabolic regulation by interfering with the IRS-1/PI3K/Akt signaling pathways, which are critical for maintaining glucose balance and beta-cell function.
Exposure to chemicals like DDT and its metabolite DDE has been linked to a higher risk of type 2 diabetes. These pollutants also promote inflammation in adipose tissue by increasing cytokines (such as IL-6 and TNF-α) while reducing adiponectin levels. For women with PCOS, who already face insulin resistance, this creates a harmful cycle: elevated insulin levels stimulate more androgen production, worsening both hormonal and metabolic issues.
What You Need to Know About Endocrine Disruptors and Your Fertility - Dr Lora Shahine
sbb-itb-6dba428
How to Reduce EDC Exposure in Daily Life
Protecting your hormonal health doesn’t stop at medical treatments - it also involves making conscious choices to reduce exposure to endocrine-disrupting chemicals (EDCs). Research has clearly linked EDCs to hormonal imbalances, and since many of these chemicals break down quickly in the body, cutting back on exposure can lead to noticeable improvements. According to the CDC, over 90% of Americans carry detectable levels of plastic-related chemicals in their bodies, highlighting the need for action.
Safer Food and Beverage Practices
Your kitchen is a great place to start. Avoid microwaving food in plastic containers; always transfer it to glass, ceramic, or stainless steel instead.
"Never microwave food in plastic – rather, transfer to a ceramic, glass or similar container."
A 2024 Consumer Reports study found that bisphenols (like BPA, BPS, and BPF) were present in 79% of the foods tested, while phthalates showed up in about 75% of grocery store items. Alarmingly, pregnant women consuming 10% more calories from ultra-processed foods had 13% higher levels of the phthalate DEHP in their urine.
To minimize exposure, store leftovers in glass or stainless steel containers, especially acidic or oily foods like tomato sauce or salad dressings. Opt for fresh or frozen produce instead of canned goods, as most cans are lined with BPA or BPS. For drinking water, invest in a high-quality filter that removes contaminants like arsenic, lead, and perchlorate, and use refillable glass or stainless steel bottles instead of single-use plastic.
Take a closer look at your cookware, too. Non-stick pans often contain PFAS, so replace them with cast iron, stainless steel, or glass options. Be cautious with black plastic utensils, which may come from recycled electronic waste and contain flame retardants. Even compostable plates and cutlery can be a concern, as they often include PFAS for grease resistance.
Reducing EDC exposure doesn’t stop with food - your personal care routine also plays a big role.
Choosing Safer Personal Care Products
Women tend to face higher EDC exposure due to frequent use of personal care products. Phthalates, for example, are often hidden under the vague label "fragrance" on ingredient lists.
To reduce risks, choose products labeled "fragrance-free" and "paraben-free". When it comes to sunscreen, go for mineral-based options containing zinc oxide or titanium dioxide rather than chemical UV filters, which can disrupt hormone function. Avoid antibacterial soaps containing triclosan, another known endocrine disruptor. Simplifying your routine by using fewer products with shorter ingredient lists can further cut down on chemical exposure.
Beyond personal care, household habits can also make a big difference.
Reducing Household and Environmental Sources
Start by washing produce thoroughly under tap water to remove pesticide residues. Whenever possible, choose organic produce to limit pesticide exposure. Reducing your intake of animal products like meat, milk, and eggs can also help, as fat-soluble dioxins tend to accumulate in animal tissue.
"The problem is, none of the plastics that we have right now are safe. That's not a very nice thing to hear, but that's what the data tell us."
With over 5,400 chemicals in plastics classified as "chemicals of concern" for human health, small, manageable changes in your daily routine can go a long way in reducing exposure.
What We Know and What We Don't: Current Research Status
Where the Evidence Is Strong
Research from countries like the UK, Greece, and Turkey consistently reveals a link between higher BPA levels and PCOS in women and adolescents. These studies highlight correlations with elevated testosterone levels and the presence of polycystic ovary morphology. A 2013 study in Italy also connected increased BPA levels to insulin resistance, fatty liver disease, and inflammation. Meanwhile, animal studies provide further support, showing that exposure to endocrine-disrupting chemicals (EDCs) can directly impact ovarian function.
While this evidence strongly suggests a connection between EDC exposure and PCOS, there’s still a lot we don’t fully understand.
Gaps in Current Research
Even with these findings, several obstacles make it challenging to draw clear conclusions. As Andrea Gore, a professor at the University of Texas at Austin, points out:
"It is difficult to prove a cause-and-effect link between exposure to a specific chemical and a negative health outcome."
In humans, much of the evidence remains correlational, while animal studies offer the clearest insights into causation.
One major challenge is BPA’s short half-life - just 4 to 5 hours in adults - which complicates efforts to link early-life exposures to long-term health effects. Additionally, persistent organic pollutants (POPs) stored in white adipose tissue can lead to underestimation of true exposure levels when using standard serum or urine tests.
With around 85,000 synthetic chemicals in use today - and over 1,000 suspected to disrupt endocrine function - research on BPA alternatives like BPS and BPF remains limited. Perhaps most concerning, humans are exposed to complex mixtures of chemicals daily, yet most studies focus on individual substances in isolation.
Conclusion: Combining Prevention with Medical Treatment
Endocrine-disrupting chemicals (EDCs) can disrupt hormone production, metabolism, and function by mimicking or blocking key hormones. While ongoing research continues to shed light on these effects, the link between EDC exposure and conditions like PCOS, insulin resistance, and hyperandrogenism is too substantial to overlook. This connection highlights the importance of reducing daily exposure to harmful chemicals.
Limiting contact with substances like BPA, phthalates, and PFAS can help lower the chemical buildup that worsens hormonal imbalances. Even small adjustments in your daily routine can have a meaningful impact. As the Endocrine Society emphasizes:
"Even if some health effects are not fully proven, taking precautions is wise. Become familiar with EDCs to which you and your family may be exposed. Try to avoid unnecessary, preventable exposure to EDC-containing consumer products."
However, prevention alone may not fully resolve symptoms like excessive facial hair, hair thinning, acne, or irregular periods. When lifestyle changes fall short, targeted medical treatments become necessary. Options such as Spironolactone for hirsutism, Oral Minoxidil for hair loss, or insulin sensitizers like Metformin can address the hormonal imbalances that lifestyle adjustments alone cannot completely manage.
By combining efforts to reduce EDC exposure with medical treatments, you can address both the root causes and the ongoing effects of hormonal imbalances. For those seeking personalized care, Oana Health offers telehealth solutions tailored to women managing PCOS and hormonal health challenges. Licensed healthcare providers review your health history, prescribe treatments suited to your symptoms - whether focused on insulin resistance, androgen levels, or weight management - and deliver them directly to your door with free shipping. This makes expert care both convenient and accessible.
The best results come from a combined strategy: actively reduce your exposure to EDCs while pursuing medical treatments that target your specific hormonal issues. This two-pronged approach tackles external triggers and internal imbalances, offering long-term relief and better overall outcomes.
FAQs
How can I avoid endocrine-disrupting chemicals in everyday products?
Endocrine-disrupting chemicals (EDCs) have a sneaky way of interfering with your hormones. They’re often lurking in everyday items like plastics, cosmetics, and even certain foods. Want to reduce your exposure? Start by reading labels carefully and steering clear of ingredients such as BPA, BPS, phthalates, parabens, and triclosan. Switching to glass or stainless-steel containers instead of plastic is another smart move, as is choosing BPA-free canned goods whenever possible.
When it comes to personal care products, go for options that are fragrance-free or labeled paraben-free. For your diet, consider buying organic produce when you can, or make sure to thoroughly wash fruits and vegetables to lower pesticide residues. In the kitchen, swap out non-stick cookware for stainless steel or cast iron alternatives. And don’t forget about your water - using a high-quality water filter can help remove trace chemicals from your drinking supply.
If you’re worried about how EDCs might be impacting your hormones, Oana Health provides telehealth consultations and tailored treatments for issues like PCOS, weight management, and other hormone-related concerns.
How do endocrine disruptors impact women with PCOS?
Endocrine-disrupting chemicals (EDCs) - like bisphenol A (BPA), phthalates, and parabens - can make hormonal imbalances and metabolic issues worse for women with PCOS. Studies have found that exposure to these chemicals is linked to higher testosterone levels, reduced sex hormone-binding globulin (SHBG), and an increased LH/FSH ratio. These changes can amplify common PCOS symptoms, including irregular periods, acne, and excessive hair growth.
EDCs also disrupt insulin signaling and lipid metabolism, which can worsen insulin resistance - a condition affecting up to 70% of women with PCOS. This often leads to issues like weight gain and increased abdominal fat. Since these chemicals are present in everyday products like food packaging, plastics, and personal care items, making small changes - such as using BPA-free containers, cutting back on processed foods, and switching to fragrance-free products - may help reduce exposure.
For a more targeted approach, Oana Health offers telehealth services designed specifically for women with PCOS. These treatments focus on hormonal balance, insulin resistance, and weight management, all delivered right to your home.
What are the long-term health risks of early exposure to endocrine disruptors?
Early exposure to endocrine-disrupting chemicals (EDCs) has been associated with a range of long-term health concerns. These chemicals can interfere with hormone signaling during critical life stages like fetal development and puberty. The potential outcomes? Issues such as reduced fertility, polycystic ovary syndrome (PCOS), endometriosis, early puberty, and even certain cancers. Beyond reproductive health, EDCs have also been linked to conditions like obesity, type 2 diabetes, and metabolic syndrome.
There’s more. Research indicates that EDCs may affect brain development, increasing the risk of behavioral and learning challenges, including ADHD. Some evidence suggests these exposures could even lead to lasting epigenetic changes, heightening the likelihood of chronic diseases later in life.
If early exposure to EDCs is a concern, addressing potential hormonal imbalances becomes essential. Oana Health offers telehealth services focused on female hormone health and PCOS treatments. Their personalized, science-based approach targets issues like weight management, insulin resistance, acne, and unwanted facial hair. By consulting a licensed medical professional through Oana Health, you can take meaningful steps toward improving your hormonal health.
