FUE Hair Transplant for PCOS-Related Hair Loss
PCOS (Polycystic Ovary Syndrome) often leads to hair loss caused by hormonal imbalances, particularly increased DHT levels. FUE (Follicular Unit Extraction) is a surgical solution for restoring hair in women dealing with PCOS-related thinning. Here's what you need to know:
- PCOS and Hair Loss: Elevated androgens like DHT trigger hair follicle shrinkage, causing thinning and eventual hair loss. Insulin resistance in PCOS further worsens the issue.
- FUE Process: Hair follicles are extracted from the back of the scalp (DHT-resistant area) and transplanted to thinning regions. This method avoids large scars and ensures natural growth.
- Preparation: Hormonal stabilization (6–12 months) is crucial before surgery to prevent further hair loss. Medications like Spironolactone and Metformin can help.
- Recovery: Healing takes 3–5 days, with full hair growth visible after 12–18 months. Post-surgery care, including ongoing PCOS treatments, is key to maintaining results.
FUE offers a long-term option for addressing visible hair loss, but ongoing management of PCOS-related hormones is essential for preserving native hair and achieving the best outcome.
How FUE Hair Transplants Work for PCOS Hair Loss
The FUE Procedure Explained
FUE (Follicular Unit Extraction) offers a precise and minimally invasive way to address PCOS-related hair loss. This method involves extracting individual hair follicles from the occipital region - an area on the back of the scalp - using tiny punch tools (usually 0.7–0.9 mm in diameter). These follicles, which are genetically resistant to DHT (dihydrotestosterone), are then implanted into thinning areas, ensuring continued growth even in the presence of hormonal imbalances.
"Donor dominance is explained as the hair transplanted from the donor area of the scalp (occiput) will continue to grow in the recipient area as if it is in its original site." – Amit S Kerure, Consultant Dermatologist and Hair Transplant Surgeon
The mid-occipital region, often referred to as the "safe donor zone", typically contains 65 to 85 follicular units per square centimeter. For optimal results, areas with densities above 80 units/cm² are preferred, while regions below 40 units/cm² may not provide sufficient grafts. This technical precision is what makes FUE particularly effective for individuals with PCOS-related hair thinning.
Benefits of FUE for Women with PCOS
Women with PCOS often experience unique patterns of hair thinning, and FUE offers a tailored solution to address these challenges. Unlike the traditional strip surgery method (FUT), FUE eliminates the need for a linear incision, leaving behind only small circular scars that are nearly invisible. This allows for more versatile styling options. Additionally, the recovery process is quicker, with minimal discomfort and a faster return to daily life.
FUE is especially effective in restoring density in areas affected by PCOS-related thinning, such as the "Christmas tree" pattern or temple recession. By carefully selecting follicular units based on their size and hair diameter, surgeons can create a natural, fuller appearance in thinning areas. The transplanted follicles, being resistant to androgens, continue to grow and thrive, providing a long-term solution for hair loss.
| Feature | Follicular Unit Extraction (FUE) | Follicular Unit Transplantation (FUT) |
|---|---|---|
| Scarring | Small circular scars, nearly invisible | Linear scar at the back of the head |
| Recovery Time | Faster healing with less downtime | Longer recovery due to sutures |
| Shaving Required | Typically requires shaving the donor area | Usually does not require shaving |
| Pain Level | Minimal postoperative discomfort | Possible discomfort or tension at the incision site |
Preparing for FUE Hair Transplant as a PCOS Patient
Why Hormonal Stabilization Matters
Before scheduling an FUE hair transplant, it’s crucial to address hormonal imbalances. Without achieving stability, hair thinning can persist - not just in existing hair but also in the transplanted follicles.
"In PCOS, controlling the androgen overproduction of male hormones and stabilizing the disease is an essential first step prior to the use of these drugs for androgen effects on the hair follicle." – Walter Futterweit, MD, FACE, FACP
It’s recommended to wait 6–12 months after stabilizing your hormones before moving forward with a transplant. Medical treatments aimed at slowing hair loss often take 4–7 months to show noticeable effects, and visible stabilization usually requires an additional 3–6 months of consistent care. This process is essential to ensure that native hair doesn’t continue thinning, which could lead to a patchy look post-surgery.
Medications like Spironolactone (150–200 mg daily) are effective in blocking the effects of dihydrotestosterone (DHT) on hair follicles, while Metformin can help manage insulin resistance and reduce androgen production from the ovaries. These steps are key to setting the stage for successful FUE outcomes.
Pre-Surgery Preparation Steps
Once your hormones are under control, taking the right steps before surgery can greatly improve your results. Start by running a full hormone panel (including testosterone, DHT, and LH/FSH ratio), thyroid screenings, and nutrient tests for zinc, ferritin, and vitamin D. These tests help confirm that PCOS is the root cause of your hair loss and rule out other potential factors.
Adopting a low-glycemic diet filled with whole grains, leafy greens, and fatty fish can help stabilize blood sugar levels and reduce androgen spikes. Research shows that even losing 5% of your body weight can significantly lower androgen levels. Additionally, aim for 7–8 hours of quality sleep and maintain a regular exercise routine to improve insulin sensitivity.
For scalp health, avoid tight hairstyles that could lead to traction alopecia, use wide-toothed combs to minimize breakage, and try gentle scalp massages to boost circulation. If needed, consider adding supplements like zinc and biotin to your routine.
For more personalized PCOS management, Oana Health offers telehealth consultations with licensed professionals. Their science-backed treatments include Topical Spironolactone for $43 per month and Oral Minoxidil for $25 per month.
"Early treatment is more likely to render positive results than waiting until the hair loss is severe." – Nicole Galan, RN
Taking these steps now ensures you’re fully prepared for a smooth FUE procedure and a successful recovery.
What to Expect During and After the FUE Procedure
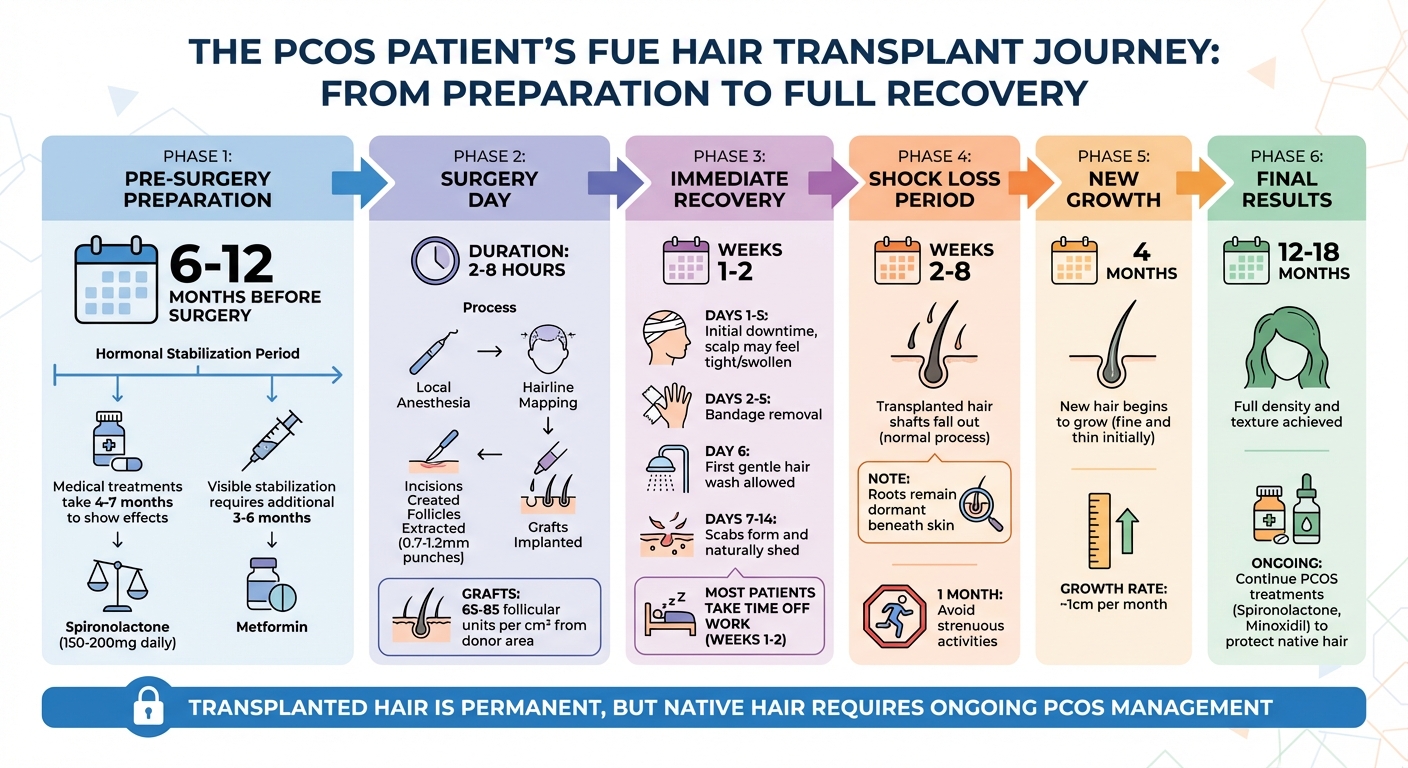
FUE Hair Transplant Timeline for PCOS Patients: Pre-Surgery to Full Results
The FUE Procedure: Step-by-Step
The FUE procedure starts with your surgeon carefully mapping out the donor and recipient areas. This includes designing a natural-looking hairline that aligns with your hair loss pattern and ensures a balanced appearance. To keep you comfortable, local anesthesia is applied using a dilute tumescent technique, which provides long-lasting numbing with minimal risks. In some cases, oral or IV sedation may also be offered for added relaxation.
Once the anesthesia takes effect, the surgeon creates precise incisions in the thinning areas where the transplanted hair will be placed. These incisions determine the angle and direction of the new hair, ensuring it looks natural [23, 25]. Then, individual follicular units - each containing 1 to 4 hairs - are extracted from the "safe donor area" using micro-punches that range between 0.7 and 1.2 mm in size [23, 24].
"The skill in harvesting follicular units really relies on the mastery and experience on the part of the hair transplant surgeon, as the procedure requires a delicate touch, stamina, and judgment." – ISHRS
After extraction, the grafts are carefully placed into the prepared recipient sites using either forceps or specialized implanter tools [23, 27]. For women with PCOS, surgeons often use single-hair grafts in the front rows to create a soft, natural hairline. Once all the grafts are positioned, the scalp is cleaned, and a protective bandage may be applied. The entire procedure can last anywhere from 2 to 8 hours, depending on the number of grafts required.
It's worth noting that FUE typically involves shaving part of the donor area, which can be a concern for some women. However, "no-shave" options are available for those willing to pay a higher cost. After the procedure, the recovery process begins, focusing on promoting graft survival and encouraging healthy hair growth.
Recovery Timeline and Post-Procedure Care
Recovery kicks off with an initial downtime of about 3 to 5 days. Bandages are usually removed within 2 to 5 days, during which the scalp may feel tight, sore, or slightly swollen. It's crucial to avoid touching or washing the grafts during this early phase, as they need time to anchor securely. By day 6, you can gently wash your hair by hand using an unscented shampoo.
Between 7 and 14 days after surgery, scabs will form around the graft sites. These scabs will naturally shed on their own or with gentle rubbing [23, 28]. Many patients take 1 to 2 weeks off work during this period to focus on healing. Strenuous activities, including exercise, should be avoided for at least a month to prevent tension on the scalp and ensure proper healing.
During weeks 2 to 8, you may notice the transplanted hair shafts falling out - a normal process called "shock loss." While the hair shafts fall, the roots remain dormant beneath the skin, ready to grow in time [23, 28].
Around the 4-month mark, new hair will begin to grow. Initially, these strands may appear fine and thin, but they will thicken as time goes on. Hair typically grows at a rate of about 1 cm per month, with the full results - showing complete density and texture - becoming visible between 12 and 18 months after the procedure [23, 28].
For women with PCOS, continuing treatments like minoxidil or spironolactone after surgery is critical to protect the native, non-transplanted hair from further thinning caused by DHT [3, 5].
Here’s a quick look at what the recovery process involves:
| Recovery Phase | Timeline | What to Expect |
|---|---|---|
| Bandage Removal | 2–5 Days | Scalp may feel tight or swollen |
| First Hair Wash | Day 6 | Gentle hand washing only |
| Scab Shedding | 7–14 Days | Scabs naturally fall off [23, 28] |
| Shock Loss | 2–8 Weeks | Hair shafts fall out; roots remain [23, 28] |
| Initial Growth | 4 Months | Fine new hairs start to appear |
| Full Results | 12–18 Months | Final density and texture achieved [23, 28] |
During the first two weeks, it's especially important to avoid disturbing the transplanted area. Activities like wearing hats or anything that could disrupt the healing grafts should be avoided during this critical period. Proper care and patience will ensure the best possible outcome.
sbb-itb-6dba428
Maintaining Results After FUE for PCOS Patients
Expected Results and How Long They Last
Hair transplanted through FUE (Follicular Unit Extraction) is designed to be permanent. The follicles taken from the safe donor area - typically the back of the head - are naturally resistant to hormones like DHT (dihydrotestosterone). This means they retain their original properties even after being relocated to areas affected by thinning or hair loss.
"Because occipital hairs are resistant to androgens, transplanted hairs retain their donor characteristics, including caliber." – StatPearls
Although the transplanted hair will continue to grow for a lifetime, the native hair around it remains susceptible to the effects of PCOS (Polycystic Ovary Syndrome). Without proper management, these non-transplanted hairs can undergo miniaturization - a process where thick, healthy strands gradually shrink into finer, shorter hairs. Over time, this can lead to noticeable thinning in untreated areas. So, while the transplant itself is permanent, maintaining the surrounding hair requires ongoing effort.
Preserving Native Hair with PCOS Therapies
To protect native hair, consistent PCOS management is crucial. Anti-androgen treatments like Spironolactone (around $14/month) and Oral Minoxidil (approximately $25/month) can prolong the growth phase of hair. Additionally, products like the Hair Plus Plus formula (priced at $40/month) may encourage regrowth and improve density over time. Addressing insulin resistance with medications such as Metformin can also help reduce androgen levels, which play a key role in hair loss. However, these treatments often require patience, as noticeable improvements may take 6 to 12 months.
"Patients should continue therapy... following hair transplantation to avoid disease recurrence." – StatPearls
Without consistent therapy, the native hair may continue to thin, potentially impacting the overall results of the transplant. Even small lifestyle changes, such as modest weight loss, can positively affect hormonal balance and support hair health. By combining surgical hair restoration with ongoing medical treatments, patients can maximize their results and maintain a natural, fuller appearance for years to come.
Conclusion
FUE hair transplants can effectively restore visible hair density for women with PCOS, but they don't tackle the root issue: hormonal imbalance. While grafts taken from the back of the scalp are naturally resistant to DHT, the native hair remains susceptible to the effects of androgens, which underscores the importance of addressing the hormonal component.
It's recommended to achieve hormonal balance about 6–12 months before undergoing surgery. This helps create the best conditions for the transplant and minimizes the risk of shock loss. After the procedure, treatments like Spironolactone (starting at $14/month) or Oral Minoxidil (starting at $25/month) can help protect the native hair from further thinning. Combining these treatments with surgery ensures a more sustainable approach to hair health.
"In PCOS, controlling the androgen overproduction of male hormones and stabilizing the disease is an essential first step prior to the use of these drugs for androgen effects on the hair follicle." – Walter Futterweit, MD, FACE, FACP
For the best long-term results, a dual approach is key: surgical restoration to address visible thinning and hormonal therapy to tackle the underlying causes like androgen excess and insulin resistance. Together, these strategies can prevent ongoing hair loss and support healthier, fuller hair over time.
To ensure success, consult both a hormone specialist and a hair restoration surgeon. This comprehensive plan offers the most effective path to achieving and maintaining lasting hair health.
FAQs
What makes FUE different from other hair transplant methods for PCOS-related hair loss?
FUE, or Follicular Unit Extraction, is a hair transplant technique that removes individual hair follicles using a small punch tool, usually between 0.7 and 1 mm in size. Because it doesn’t involve cutting a strip of scalp, this method avoids leaving a linear scar and typically allows for a faster recovery compared to other approaches.
By comparison, FUT (Follicular Unit Transplantation) requires removing an entire strip of scalp, which results in a visible linear scar. Meanwhile, DHI (Direct Hair Implantation) also extracts individual follicles but uses a specialized pen to implant the grafts directly. FUE stands out for delivering natural-looking outcomes with minimal downtime, making it particularly appealing for women dealing with PCOS-related hair loss.
How can I prepare for an FUE hair transplant if I have PCOS?
Preparing for an FUE hair transplant when dealing with PCOS requires attention to both your hormonal health and the surgical process itself. The first step is consulting a healthcare provider to confirm your PCOS diagnosis and assess hormone levels like testosterone and insulin. This evaluation helps determine if FUE is a suitable option for your situation.
Addressing hormonal imbalances beforehand is crucial. Treatments such as anti-androgens or topical minoxidil - available through providers like Oana Health - can help improve the success of the transplant by minimizing hair shedding and supporting graft survival. It’s also important to review any medications or supplements you’re taking. Blood thinners, NSAIDs, or other substances that might interfere with healing or increase bleeding risks should be discussed with your surgeon, who will guide you on making any necessary adjustments.
In the days leading up to surgery, your surgeon will evaluate your scalp and donor area to plan the procedure. Be sure to follow all pre-op instructions, such as avoiding smoking, alcohol, and caffeine for 48 hours, washing your scalp the night before surgery, and arranging for transportation on the day of the procedure. These preparations are key to setting yourself up for a smooth transplant and recovery process.
How can I preserve the results of an FUE hair transplant while managing PCOS-related hair loss?
To keep the results of your FUE hair transplant intact, addressing PCOS-related hormonal imbalances is key. This might involve anti-androgen treatments, like topical spironolactone, which can help regulate hormone levels. Using daily minoxidil is another effective way to support the transplanted follicles and encourage healthy hair growth.
Equally important is sticking to your post-operative care plan. Following these instructions carefully ensures your scalp heals properly and the transplant thrives. Regular follow-ups with your healthcare provider are also crucial - they can track your progress, tweak treatments if needed, and help maintain both your hair health and overall well-being.
