Hair Transplants for Androgenic Alopecia in Women
Hair transplants are a promising solution for women with androgenic alopecia, especially for those who haven't seen results from medical treatments like minoxidil. This condition, affecting millions of women, leads to thinning hair primarily on the crown and top of the scalp. The procedure involves relocating hair follicles from the back of the scalp to thinning areas, with satisfaction rates exceeding 88%. However, success depends on factors like donor hair quality, medical management, and addressing underlying hormonal issues. Techniques such as FUT, FUE, and DHI offer different benefits, with costs ranging from $8,000 to $20,000 in the U.S.
Key Points:
- Who benefits: Women with stable thinning patterns and healthy donor areas.
- Results timeline: New hair growth starts at 3–4 months, with full results in 12–15 months.
- Risks: Temporary shedding, scarring, and the need for ongoing medical treatments to maintain results.
- Medical support: Treatments like minoxidil and spironolactone are essential for preserving native hair.
Hair transplants can restore confidence and improve quality of life, but they require careful planning, realistic expectations, and a commitment to follow-up care.
How Effective Are Hair Transplants in Women?
Graft Survival Rates and Results
Hair transplants work by relocating androgen-resistant follicles from the back of the scalp to areas where hair is thinning. These transplanted hairs maintain their natural resistance to balding, even after being moved to a new location. The success of the procedure largely depends on the density of the donor area. For instance, donor zones with more than 80 follicular units per square centimeter are ideal, while those with less than 40 units per square centimeter tend to produce less favorable outcomes.
The process of seeing results takes time. Initially, the transplanted hairs shed within the first few weeks - a completely normal part of the healing process. New growth typically begins around 3 to 4 months after the procedure, with the full results becoming apparent between 12 to 15 months. The mid-occipital region, often used as the donor area, generally provides a reliable density of 65–85 follicular units per square centimeter. This consistency in graft quality often translates to high satisfaction rates among patients.
Patient Satisfaction and Quality of Life
Hair transplants often have a profound emotional and psychological impact on women. Studies show that 88.2% of women who underwent the procedure reported satisfaction levels of 75% or higher. Dr. Ross Kopelman, a hair restoration surgeon, shared a touching insight:
"I've had patients tear up in the mirror six months later, just from being able to wear a ponytail again".
For many women, the benefits go beyond physical appearance. Successful transplants can restore confidence, femininity, and a sense of control over their lives.
The popularity of hair transplants among women is growing. Between 2021 and 2024, the number of women opting for the procedure rose by more than 16%. Many patients describe the experience as transformative. However, it’s important to note that about 45.1% of women experience temporary shedding of their existing hair at the recipient site - a condition known as telogen effluvium. Fortunately, this condition usually resolves on its own. Despite the promising outcomes, hormonal factors can still influence the long-term success of the procedure.
How Hormonal Factors Affect Long-Term Results
While the transplanted follicles are resistant to androgens, the surrounding native hair remains susceptible to hormonal changes and miniaturization. This is why a thorough hormonal evaluation is essential before surgery. Women are typically advised to test for testosterone, DHEAS, iron/ferritin levels, and thyroid-stimulating hormone (TSH) to identify any underlying conditions. Issues like PCOS, thyroid dysfunction, and hyperandrogenism can all impact the longevity of the results.
"Hair transplantation in women requires a tailored approach focusing on diffuse density restoration, donor area preservation, and adjunct medical management." - Dawn Queen, MD, and Marc R. Avram, MD
Hair transplants can effectively address thinning areas, but they don’t stop the underlying progression of hair loss. For women experiencing rapid thinning, it’s recommended to stabilize their hair loss with medical treatments for 6 to 12 months before surgery. This helps to avoid "shock loss" and improve long-term outcomes. Dr. Greg Williams, a plastic surgeon and hair transplant expert, explains:
"When I speak to women with female genetic hair loss about having a hair transplant, it's about buying time rather than being a long-lasting solution".
My Hair Transplant Results After 1 Year! | Would I do it again?!
Who Is a Good Candidate and What Techniques Are Used?
Hair Transplant Techniques for Women: FUT vs FUE vs DHI Comparison
Who Qualifies for Hair Transplant Surgery?
Hair transplant success depends heavily on selecting the right candidates. Women with a stable and predictable thinning pattern are typically considered. However, those with diffuse unpatterned alopecia (DUPA) - a condition where donor areas also show thinning - are generally not eligible because they lack healthy, DHT-resistant follicles.
Before surgery, any underlying conditions must be managed. Surgeons often recommend trying medical treatments like Minoxidil for at least a year before considering a transplant. Age is another factor; most surgeons suggest waiting until at least 25 years old to ensure hair loss patterns have stabilized. Additionally, the scalp should be free of active inflammatory conditions like Alopecia Areata or Cicatricial Alopecia.
"A hair transplant is not advised in patients younger than 25." - Bernstein Medical Center
Most women achieve their desired results with one or two procedures. Surgery is generally recommended when more than 50% of native hair density in a specific area has been lost. Interestingly, only about 15% to 20% of women seeking treatment for thinning hair are deemed suitable candidates.
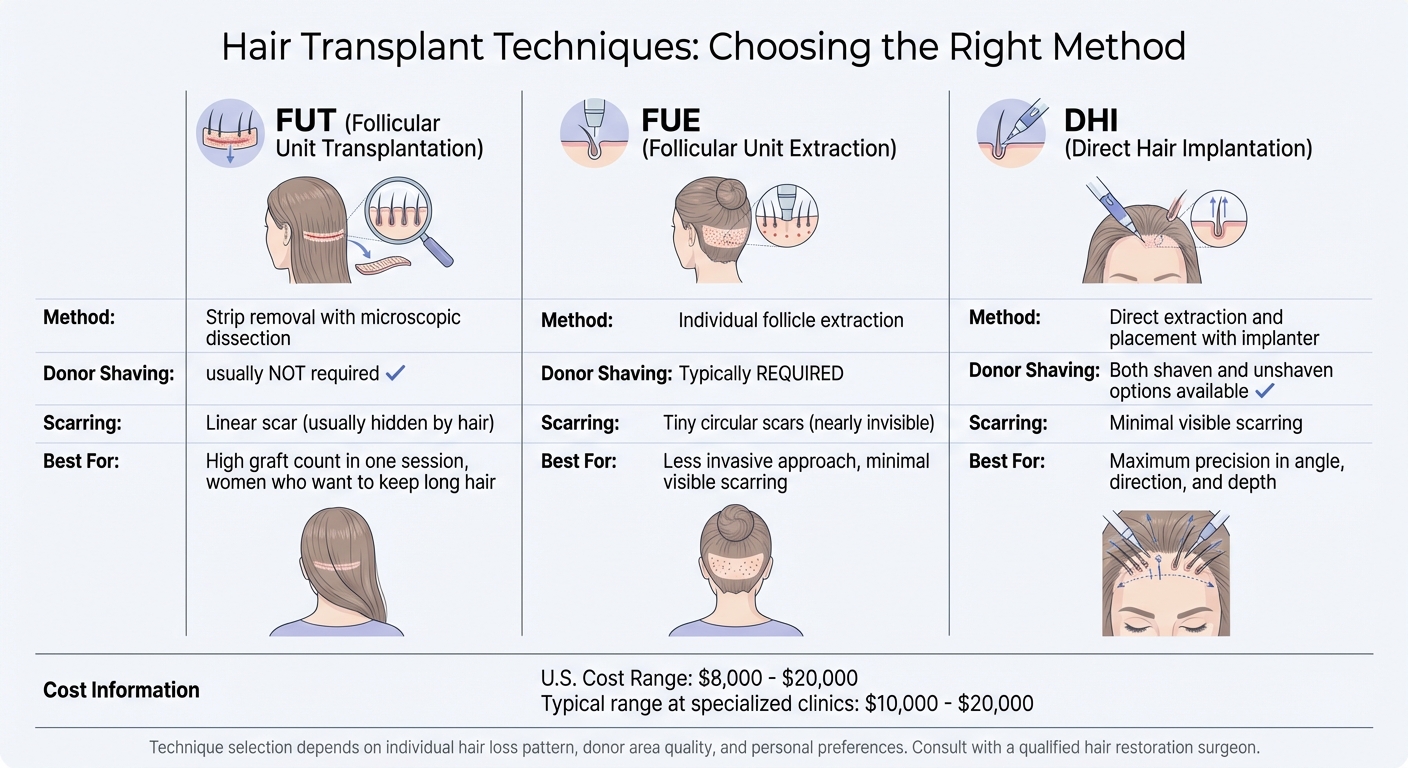
FUT, FUE, and DHI: Comparing Surgical Techniques
Once a candidate is approved, choosing the right surgical method becomes crucial.
-
Follicular Unit Transplantation (FUT):
This technique involves removing a thin strip of scalp from the donor area, which is then divided into individual follicular units. FUT is a popular choice for women as it doesn’t require shaving, making the procedure more discreet. However, it does leave a linear scar, which is usually hidden by surrounding hair. -
Follicular Unit Extraction (FUE):
FUE extracts individual hair follicles using tiny punch tools, leaving behind small, nearly invisible circular scars. Unlike FUT, this method typically requires shaving. -
Direct Hair Implantation (DHI):
DHI uses a specialized implanter tool to extract and directly implant follicles. This approach offers both shaven and unshaven options, along with precise control over the angle, direction, and depth of each graft.
| Feature | FUT | FUE | DHI |
|---|---|---|---|
| Method | Strip removal; microscopic dissection | Individual follicle extraction | Direct extraction and placement |
| Donor Shaving | Usually not required | Typically required | Both options available |
| Scarring | Linear scar (usually hidden) | Tiny circular scars | Minimal visible scarring |
Each technique has its strengths. FUT is ideal for achieving a high number of grafts in one session, FUE offers a less invasive approach, and DHI provides unmatched precision in graft placement.
Many women prefer FUT since it allows them to maintain their long hair and conceal the procedure. In the U.S., the cost of female hair transplants typically ranges from $8,000 to $20,000, with clinics like Dr. Yates Hair Sciences reporting prices between $10,000 and $20,000.
Regardless of the chosen method, designing a natural-looking hairline is key to achieving satisfying results.
Creating a Natural Hairline for Women
Designing a natural hairline for women requires a unique approach compared to men. Women’s hairlines tend to have a softer, more rounded contour rather than the sharper, angular designs often preferred by male patients. Most women retain their original frontal hairline, focusing instead on restoring density in thinning areas.
"Female hairlines typically follow a softer, rounded contour, unlike the sharp, angular hairlines frequently desired by male patients. Sensitive hairline design is essential for natural results." - Dr. Linkov, ISHRS
To ensure the most natural look, surgeons use single-hair grafts for the first few rows of the hairline to avoid a "pluggy" appearance. They often select finer hairs from the lower occipital region to create a smooth transition. Careful attention is also given to reconstructing the natural directional split (or partline) and ensuring the grafts mimic the natural angle and direction of hair growth.
"It's about restoring strategic density and a natural frame to the face." - Ross Kopelman, DO
Surgeons often refer to old photographs to recreate a hairline that matches the patient’s original facial proportions. The goal is to design a hairline that looks natural not only immediately after surgery but also decades later. Instead of focusing solely on covering bald spots, priority is given to restoring density in thinning areas, ensuring a balanced and timeless result.
sbb-itb-6dba428
Risks, Limitations, and Maintaining Results
Possible Risks and Side Effects
Hair transplants, like any surgical procedure, come with potential risks. Common complications include infection, scarring, bleeding, and graft failure. The type of scarring depends on the technique used: FUT often leaves a linear scar in the donor area, while FUE results in smaller, circular scars.
Another concern is shock loss, a temporary shedding of hair in the recipient area, which occurs in 45.1% of women. However, in cases where follicles are highly miniaturized, this shedding could become permanent. Additionally, 15.4% of women experience postoperative scalp folliculitis, an inflammation of the hair follicles.
"A high degree of miniaturization puts the patient at risk for shock loss at the recipient site, which can be permanent." - Jennifer Goldin, Patrick M. Zito, and Blake S. Raggio
To reduce risks, surgeons often recommend specific pre- and post-surgery guidelines. These include stopping smoking 3 to 6 weeks before and after the procedure to improve healing and graft survival. Patients are also advised to discontinue minoxidil one week prior and avoid alcohol or recreational drugs for three days leading up to surgery.
Understanding these potential risks highlights the importance of careful patient selection and preoperative preparation.
When Hair Transplants May Not Work Well
Hair transplants are not suitable for everyone. Women with diffuse unpatterned alopecia (DUPA), where thinning occurs even in the donor areas, may not have the healthy, androgen-resistant follicles needed for a successful procedure. Generally, donor areas with fewer than 40 follicular units per square centimeter are considered inadequate for surgery.
Certain scalp conditions, like lichen planopilaris or alopecia areata, can also interfere with graft survival and must be treated before surgery. In cases of frontal fibrosing alopecia (FFA), graft survival rates drop significantly over time - from 87% after one year to just 41% after five years.
Women experiencing rapid or unstable hair loss should stabilize their condition with medical treatments for 6 to 12 months before considering a transplant. Surgery during an active shedding phase increases the chances of permanent shock loss. It’s also important to set realistic expectations - hair transplants offer an "illusion of density" rather than a complete restoration of hair volume.
Because of these challenges, ongoing medical treatments are critical to maintaining the results of a transplant.
Using Medical Treatments to Maintain Results
While transplanted hair is generally resistant to thinning, the surrounding native hair remains vulnerable to androgenic miniaturization. This makes consistent medical therapy essential for preserving overall hair density.
Topical minoxidil is one of the most commonly prescribed treatments. It promotes hair growth and slows the thinning of native hair, but it must be used indefinitely to maintain its benefits. For women with hormonal imbalances, oral antiandrogens like spironolactone are often recommended. These medications block hormones that contribute to follicular miniaturization, with fewer than 5% of users stopping due to side effects like menstrual irregularities or dizziness.
Telehealth platforms such as Oana Health provide personalized care for women managing hair loss. Through online consultations, licensed professionals can prescribe treatments like oral minoxidil, spironolactone, or topical spironolactone, all conveniently delivered to your doorstep. These services ensure ongoing support for maintaining hair density and addressing hormonal imbalances.
What Research Is Still Needed?
Gaps in Research on Women's Hair Transplants
Although female hair transplants have increased by 16% between 2021 and 2024, there’s still a noticeable lack of research focused on women’s hair restoration. Most studies to date have primarily centered on men, leaving critical questions unanswered about how factors like hormonal changes, pregnancy, stress, and nutrition uniquely influence transplant outcomes in women.
"We don't understand female hair loss." - Dr. Greg Williams, Plastic Surgeon and Hair Transplant Specialist
Another major issue is the limited representation of diverse hair types and ethnicities. Women with Afro-textured hair face specific challenges, as their C-shaped follicles are more prone to transection during transplantation. Additionally, clinical trials often fail to address the diffuse thinning patterns common in women or the hormonal influences that can make results less predictable compared to men. Larger, more inclusive studies are essential to establish protocols that reflect these nuances.
These gaps highlight the need for new, forward-thinking approaches to hair restoration.
New Approaches in Hair Restoration
Emerging technologies are pushing the boundaries of what’s possible in hair restoration. AI-powered robotic systems now analyze scalp density and donor graft availability to create highly personalized transplant plans. These tools enhance the precision of follicle placement, helping surgeons craft more natural-looking hairlines tailored specifically for women. Additionally, these systems are better equipped to address the diffuse thinning patterns that often reduce the effectiveness of traditional techniques for women.
Beyond surgical advancements, complementary therapies are gaining traction. Treatments like PRP (Platelet-Rich Plasma), low-level laser therapy, and exosome-based approaches are being used to improve graft survival and maintain native hair density. Researchers are also exploring regenerative medicine options, such as injecting adipose-derived stem cells into recipient areas during surgery. These methods aim to encourage tissue regeneration and extend the lifespan of transplanted follicles.
Perhaps the most exciting development lies in hair follicle cloning and bioengineering. These techniques could eventually provide an unlimited supply of donor hair, offering hope to women with diffuse unpatterned alopecia - a condition that currently excludes many from surgical options. Early research into mRNA-containing liposomes and hair follicle-activating peptides also shows promise in sustaining hair growth cycles post-transplant.
Combining these cutting-edge technologies with tailored medical care could revolutionize treatment outcomes.
How Telehealth Supports Hair Loss Treatment
While surgical innovations continue to evolve, addressing the underlying causes of hair loss is just as important for long-term success. For women dealing with conditions like PCOS, thyroid disorders, or post-menopausal hormonal changes, ongoing medical management is critical to prevent further thinning in untreated areas.
Telehealth platforms, such as Oana Health, are stepping in to bridge this gap. These platforms offer online consultations and prescription services, making hormonal management more accessible. By integrating advanced surgical techniques with consistent medical care, telehealth solutions help women achieve more stable and lasting results.
Conclusion
Hair transplantation has proven to be an effective option for women dealing with androgenic alopecia, with 88.2% of patients reporting satisfaction levels exceeding 75% after their procedures. However, achieving success hinges on several key factors: ensuring sufficient graft volume, carefully selecting candidates, and - most critically - pairing surgical procedures with ongoing medical treatment.
Surgery alone won’t stop the progression of androgenic alopecia. While transplanted hair can flourish, the surrounding natural hair may continue to thin without proper pharmaceutical support. For women experiencing rapid hair loss, stabilizing the condition with medical therapy for 6 to 12 months before surgery is vital to reduce the risk of shock loss. After surgery, treatments like minoxidil are essential for preserving hair density in non-transplanted areas, emphasizing the importance of addressing the underlying hormonal causes.
In addition, managing systemic hormonal issues - such as PCOS, thyroid imbalances, or iron deficiencies - is critical for long-term results. Telehealth platforms like Oana Health offer convenient solutions by providing consultations and access to medications like oral minoxidil and spironolactone. These services make it easier for women to tackle the hormonal factors that influence hair health, both before and after a transplant.
Ultimately, hair restoration works best as part of a comprehensive and ongoing plan. With advancements in surgical techniques and personalized medical care, sustainable results are more achievable than ever. Women should approach transplantation as one piece of a broader commitment to scalp health, combining surgical expertise with effective hormonal management for the best long-term outcomes.
FAQs
What affects the success of hair transplants for women with androgenic alopecia?
The success of hair transplants for women dealing with androgenic alopecia depends on a variety of factors. One of the first steps is evaluating the extent and pattern of hair thinning. Women often experience more diffuse thinning across the scalp, which means the approach needs to be carefully tailored to evenly restore density. The condition of the scalp also plays a big role - any underlying issues, like scarring or traction alopecia, should be addressed before moving forward with surgery.
Another crucial factor is the quality and availability of donor hair, usually sourced from the back or sides of the scalp. Techniques like follicular unit transplantation (FUT) are commonly used to preserve the donor area, while follicular unit extraction (FUE) can also provide natural-looking results. The choice between these methods often depends on factors like donor hair density, scalp flexibility, and the skill of the surgeon performing the procedure.
To improve results, complementary treatments can make a difference. For instance, addressing hormonal imbalances or using topical solutions like minoxidil can boost graft survival and enhance overall outcomes. Women who begin treatment earlier in their hair loss journey and maintain realistic expectations tend to see better results. For those exploring non-surgical options, Oana Health offers telehealth consultations and prescription-based therapies to support hair restoration efforts.
Can hormonal imbalances affect the results of hair transplants for women?
Yes, hormonal imbalances - like elevated androgens or shifts in estrogen and progesterone - can affect the long-term success of hair transplants. These imbalances might lead to continued hair thinning around the transplanted area, especially in women dealing with conditions such as androgenic alopecia, PCOS, or thyroid issues. If these underlying problems aren't addressed, both transplanted and natural hair could be impacted over time.
To enhance results, many specialists suggest combining hair transplants with medical treatments. Options include anti-androgen therapy, hormone-regulating plans, or topical treatments like minoxidil. These methods help create a more stable scalp environment and protect the transplanted grafts, improving long-term success.
If you suspect hormones are playing a role in your hair loss, Oana Health provides personalized, prescription-based treatments to target hormonal imbalances and support hair health - all conveniently from home.
What are the main differences between FUT, FUE, and DHI hair transplant techniques?
FUT (Follicular Unit Transplantation), FUE (Follicular Unit Extraction), and DHI (Direct Hair Implantation) are the three main approaches to hair transplants. They vary in how the hair follicles are harvested, the type of scarring left behind, and the way the follicles are implanted.
FUT involves taking a small strip of scalp from the back or sides of the head. This strip is then divided into individual hair follicles for transplantation. While this method allows for a larger number of grafts in a single session and helps maintain donor area density, it does leave a linear scar. This scar can be noticeable if you prefer shorter hairstyles.
FUE uses a different approach, where individual hair follicles are removed directly with a tiny punch tool. This technique avoids a linear scar, leaving only small, dot-like marks that are usually hard to see. The recovery time is shorter compared to FUT, but the number of grafts that can be harvested in one session is typically lower.
DHI builds on the FUE method by using a specialized implantation pen to place follicles directly into the scalp without the need for pre-made incisions. This technique offers precise control over hair placement and can enhance graft survival. However, it tends to take more time and requires specific tools.
Each method has its own advantages, and the right choice depends on your personal goals, hair loss pattern, and preferences.
