GLP-1 vs. Metformin: Adherence in PCOS Treatment
Struggling to stick with your PCOS treatment? You’re not alone.
When comparing GLP-1 receptor agonists (like Ozempic) and how they work in PCOS and Metformin for PCOS management, adherence rates are low for both. Here’s why:
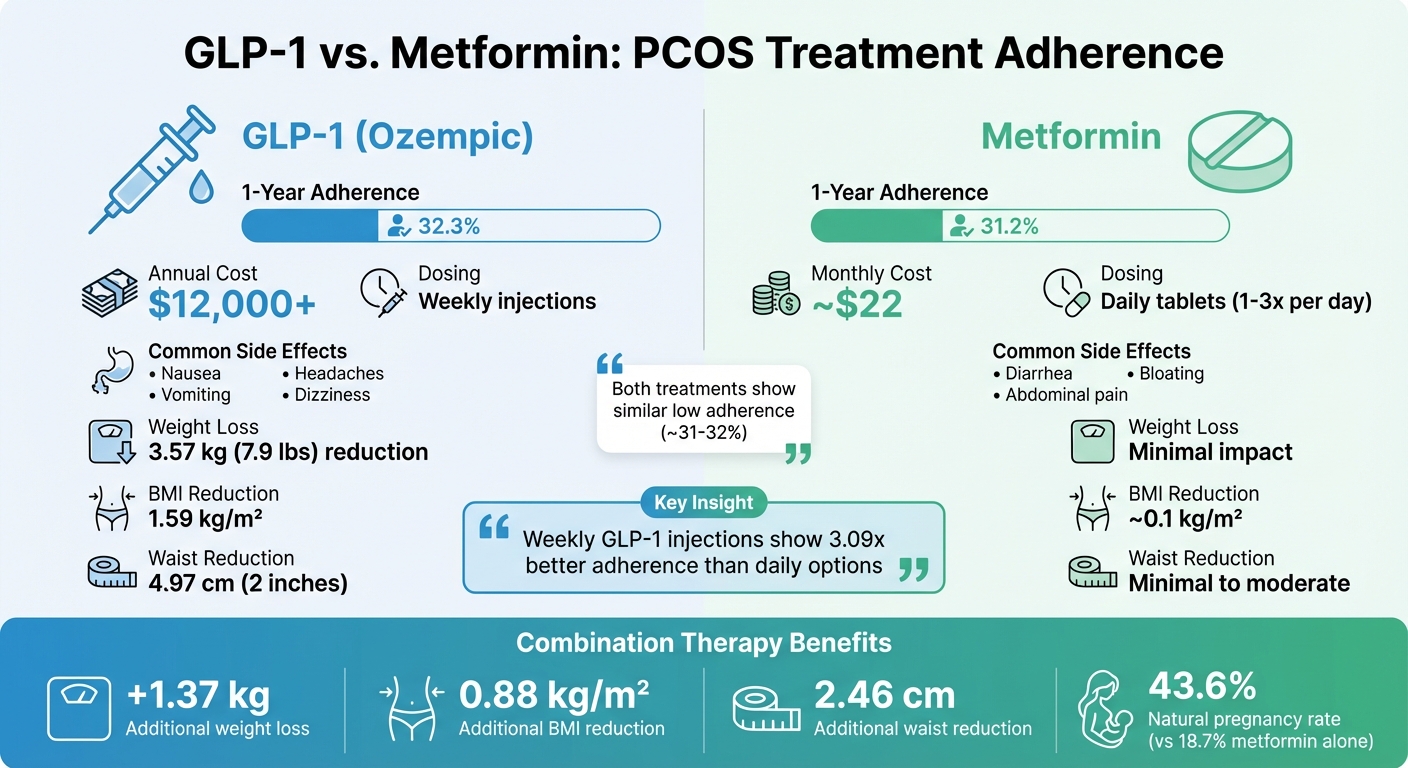
- Adherence Rates: Only 32.3% of GLP-1 users and 31.2% of Metformin users stick to their treatment after one year.
- Side Effects: GLP-1 often causes nausea and headaches, while Metformin leads to diarrhea and bloating.
- Cost: GLP-1 treatments can cost over $12,000 annually, while Metformin is far more affordable.
- Convenience: Weekly GLP-1 injections (like Ozempic) have better adherence than daily options (like Saxenda).
Quick Comparison:
| Treatment | 1-Year Adherence | Cost | Side Effects | Dosing |
|---|---|---|---|---|
| GLP-1 (Ozempic) | 32.3% | $12,000+/year | Nausea, headaches | Weekly injections |
| Metformin | 31.2% | ~$22/month | Diarrhea, bloating | Daily tablets |
Key Takeaway: GLP-1 therapies may offer better weight loss and metabolic improvements, but side effects, cost, and access limit adherence. Metformin is more affordable but less effective for weight loss. Combining both treatments can improve outcomes, though managing side effects remains critical.
GLP-1 vs Metformin for PCOS: Adherence Rates, Costs, and Side Effects Comparison
Understanding Patient Adherence in PCOS Medication
What Adherence and Nonadherence Mean
Adherence refers to consistently following prescribed PCOS treatments, whether it’s taking daily tablets or sticking to scheduled GLP-1 injections. On the flip side, nonadherence occurs when patients miss doses, stop treatments prematurely, or fail to refill their prescriptions. It’s typically defined by therapy gaps of 60 days or more, or when the Proportion of Days Covered (PDC) falls below 80%.
In developed countries, adherence rates for chronic conditions hover around 50%, but for GLP-1 therapies in PCOS, they drop to a mere 27.2% after one year. Metformin, another common treatment, sees adherence rates decline from 57.7% at three months to just 31.2% by the end of 12 months.
How Adherence Affects PCOS Outcomes
Taking medications as prescribed is essential for improving PCOS-related health outcomes. Without adherence, even the most effective treatments fail to deliver their full benefits. As Parker M. and colleagues emphasize:
"Treatment regimens are of no use if a patient does not take the medication or engage in the recommended behavior."
For instance, patients who discontinue GLP-1 therapy for weight management often regain the weight they initially lost, undoing the metabolic progress they had made. This setback prevents them from achieving critical health improvements such as enhanced insulin sensitivity, weight loss, and a reduced risk of type 2 diabetes and cardiovascular disease.
Interestingly, while clinical trials often report persistence rates above 85%, real-world adherence paints a much bleaker picture, with rates plummeting to as low as 32.3% after one year. This stark contrast highlights the importance of addressing adherence challenges.
These issues provide a foundation for examining GLP-1 agonists vs metformin for PCOS and how patients experience these treatments.
Adherence Rates: GLP-1 Receptor Agonists vs. Metformin
Comparing Adherence Data
Prime Therapeutics conducted an analysis of 4,066 commercially insured obese, non-diabetic members between January and December 2021. The study found that only 32.3% of patients remained on GLP-1 therapy after one year. For Metformin, commonly prescribed for PCOS, persistence dropped from 57.7% at three months to just 31.2% at the one-year mark.
The data also highlights notable differences between specific GLP-1 products. Weekly semaglutide (Ozempic) had a one-year persistence rate of 47.1%, significantly outperforming daily liraglutide (Saxenda), which showed a persistence rate of just 19.2%. Additionally, the median time to discontinuation was 279 days for Ozempic, compared to only 120 days for Saxenda.
| Treatment | 1-Year Persistence Rate | 1-Year Adherence (PDC ≥80%) | Median Time to Discontinuation |
|---|---|---|---|
| Semaglutide (Ozempic) | 47.1% | 40.1% | 279 days |
| Semaglutide (Wegovy) | 36.0% | 31.5% | N/A |
| Liraglutide (Saxenda) | 19.2% | 15.0% | 120 days |
| Overall GLP-1 (Obesity) | 32.3% | 27.2% | 426 days |
| Metformin (PCOS) | 31.2% | N/A | N/A |
These adherence challenges have a direct impact on treatment outcomes, particularly for managing PCOS. In prediabetic patients, a condition often linked to PCOS, the gap in adherence becomes even more pronounced. One-year nonadherence rates reach 55.68% for GLP-1 receptor agonists compared to 34.79% for Metformin. As Prime Therapeutics observed:
"This real-world study finds that persistence and adherence to these products is substantially lower than what has been reported in clinical trials".
These differences underline the importance of understanding how patient experiences in real-world settings shape adherence.
What Patients Say About Adherence
Patient experiences offer valuable insights into the barriers affecting adherence. For Metformin, approximately 30% of prescribed doses are missed, often due to side effects like diarrhea and flatulence. These gastrointestinal issues can make long-term use challenging.
GLP-1 receptor agonists come with their own set of hurdles. Annual costs exceeding $12,000 create a significant financial barrier. Additionally, shortages of semaglutide products further limit access. Side effects such as nausea and headaches, which are more common with GLP-1 therapies than with Metformin, also contribute to early discontinuation.
Convenience plays a major role in adherence. Patients using weekly GLP-1 injections are 3.09 times more likely to stick with their treatment for 12 months compared to those on daily regimens. This dosing advantage helps explain why Ozempic has higher persistence rates compared to Saxenda.
Why Adherence Rates Differ Between Treatments
Side Effects and How Patients Tolerate Them
Both GLP-1 receptor agonists and metformin are known to cause gastrointestinal distress, but the way patients experience these side effects differs significantly. GLP-1 receptor agonists are more likely to cause nausea, vomiting, dizziness, and headaches, while metformin's adverse effects are typically limited to diarrhea and abdominal pain. Neil Johnson highlighted that the gastrointestinal issues associated with metformin can sometimes lead to patients discontinuing the treatment altogether.
Professor Bing He from Shengjing Hospital of China Medical University explained:
"GLP-1 receptor agonists were associated with a higher incidence of nausea and headache than metformin"
These differences in side effect profiles play a key role in why adherence rates vary between GLP-1 therapies and metformin when used for PCOS treatment.
Cost and Access to Treatment
Financial considerations and access to medications also heavily influence adherence. GLP-1 treatments approved by the FDA come with a steep wholesale acquisition cost of over $12,000 per year. In contrast, metformin is widely available as an inexpensive generic drug, making it far more accessible for long-term use.
Insurance coverage further complicates the picture. Metformin is well-established as the first-line pharmacological option for addressing metabolic symptoms in PCOS. On the other hand, GLP-1 receptor agonists are often considered second-line or experimental treatments, especially for fertility-related outcomes. This classification can limit insurance coverage, forcing some patients to pay out of pocket or abandon treatment altogether.
Supply chain issues have also impacted GLP-1 adherence. Products like Ozempic and Wegovy, which contain semaglutide, have faced significant shortages, leading to approximately 11.1% of patients switching between different GLP-1 therapies within their first year of treatment.
Dosing Schedule and Convenience
Beyond cost and side effects, the frequency of dosing plays a critical role in adherence. According to research from the Medical University of South Carolina College of Pharmacy, patients using once-weekly GLP-1 receptor agonists showed an 11% lower risk of non-adherence compared to those using once-daily options. Erin R. Weeda emphasized:
"Once weekly dosing of injectable GLP-1RAs was associated with better adherence vs once daily dosing among patients with T2D. These findings... suggest that dosing frequency is an important factor to consider when selecting a GLP-1RA"
Metformin, on the other hand, requires daily oral dosing, which often involves taking it 1–3 times per day. The impact of dosing frequency is evident in persistence data: weekly semaglutide (Ozempic) keeps patients on treatment for a median of 279 days, compared to just 120 days for daily liraglutide (Saxenda). This nearly five-month difference underscores how dosing schedules influence patient adherence in practical settings.
How Effectiveness and Side Effects Impact Adherence
Comparing Treatment Results
When treatments deliver noticeable results, patients are more likely to stick with them, even if side effects are present. For women with PCOS, GLP-1 receptor agonists have shown better outcomes compared to metformin, particularly in weight loss and improving insulin resistance.
Studies show that GLP-1 receptor agonists can reduce BMI by an average of 1.59 kg/m² and body weight by 3.57 kg (about 7.9 lbs) compared to metformin or placebo. They also lead to a reduction in waist circumference by 4.97 cm (nearly 2 inches), which is a significant improvement over metformin. For women dealing with PCOS-related obesity, these changes can be incredibly motivating, encouraging them to continue treatment despite occasional gastrointestinal discomfort.
| Outcome Measure | GLP-1 Receptor Agonists | Metformin |
|---|---|---|
| Weight Loss | 3.57 kg (7.9 lbs) reduction | Minimal impact on weight loss |
| BMI Reduction | 1.59 kg/m² decrease | ~0.1 kg/m² decrease |
| Insulin Resistance (HOMA-IR) | Greater improvement (MD –0.58 to –1.58) | Standard improvement; less effective |
| Waist Circumference | 4.97 cm (2 in) reduction | Minimal to moderate reduction |
| Glycemic Control | Stronger reduction in post-meal glucose and fasting insulin | Effective for fasting glucose but less so for post-meal insulin |
The measurable benefits of GLP-1 therapies often outweigh the discomfort caused by side effects. Interestingly, combining GLP-1 with metformin can lead to even better weight and waist circumference reductions without significantly increasing adverse effects.
These differences in outcomes lay the foundation for understanding how side effects influence patient adherence.
Common Side Effects of Each Treatment
While treatment effectiveness encourages adherence, side effects can make or break a patient's commitment. Both GLP-1 receptor agonists and metformin are known to cause gastrointestinal issues, but their side effect profiles differ.
GLP-1 therapies frequently cause nausea and vomiting, with diarrhea being another common complaint. Aleksandra Szczesnowicz highlights these as the primary side effects, alongside occasional headaches and dizziness. Higher doses of GLP-1, often prescribed for obesity management, can intensify gastrointestinal symptoms. However, patients tend to tolerate these side effects because of the significant weight loss benefits they experience - something metformin does not offer.
Metformin, on the other hand, is more likely to cause diarrhea, abdominal cramping, and bloating. While these symptoms can be uncomfortable, they are generally more predictable and less varied compared to those caused by GLP-1 therapies.
In real-world scenarios, the trade-off between effectiveness and side effects becomes clear. Only about 32.3% of patients remain on GLP-1 therapy after one year. For those who stick with it, the promise of significant weight loss serves as a powerful motivator. However, discontinuing GLP-1 therapy often leads to weight regain, underscoring the importance of long-term adherence.
sbb-itb-6dba428
Using GLP-1 Receptor Agonists and Metformin Together
Benefits of Combining Both Treatments
Pairing GLP-1 receptor agonists with metformin delivers results that surpass using either medication alone. This combination therapy has been shown to lead to an extra 1.37 kg of weight loss, a 0.88 kg/m² decrease in BMI, and a 2.46 cm reduction in waist circumference compared to metformin by itself. Beyond weight-related improvements, it enhances insulin sensitivity (HOMA-IR reduction of 1.58), lowers fasting blood glucose by 0.30 mmol/L, and boosts SHBG levels by 10.04 nmol/L, which helps address hyperandrogenemia and its associated symptoms.
The reproductive benefits are equally noteworthy. For instance, a study revealed that after 12 weeks of combining exenatide with metformin, the natural pregnancy rate was 43.6%, compared to just 18.7% with metformin alone. Additionally, this combination improves ovulation and menstrual regularity.
Experts in the field have highlighted the synergy between these treatments. Mojca Jensterle, from the University Medical Center Ljubljana, explains:
"The combined action of both pharmacotherapies, GLP-1 and metformin, may be more effective than the individual action of each drug for the treatment of the metabolic and reproductive disturbances linked to PCOS and may even improve metabolic outcomes in women who previously exhibited deficient responses to metformin."
– Mojca Jensterle, Department of Endocrinology, University Medical Center Ljubljana
Interestingly, metformin has the ability to enhance the body’s natural GLP-1 levels, which might allow for lower doses of GLP-1 receptor agonists without sacrificing results. This combination not only improves health outcomes but can also strengthen a patient’s commitment to sticking with the treatment plan.
Adherence with Combination Therapy
The enhanced benefits of combination therapy often encourage patients to stay on track with their treatment. Positive results - such as improved weight loss and metabolic health - can be highly motivating. However, it’s worth noting that combining these medications may increase gastrointestinal side effects, making gradual dose adjustments essential.
Dosing convenience also plays a role in adherence. Studies have shown that once-weekly GLP-1 formulations reduce the risk of non-adherence by 11% compared to daily injections. Using a weekly GLP-1 option, like dulaglutide or extended-release exenatide, alongside daily metformin simplifies the routine, making it easier for patients to manage.
For women who haven’t responded well to metformin alone, adding a GLP-1 receptor agonist can be a game-changer. This combination addresses both metabolic challenges and reproductive issues, offering a valuable option for managing PCOS-related obesity and infertility.
WHO endorsement sparks new discussion around GLP-1 drugs and PCOS
How Oana Health Supports PCOS Treatment Adherence
Managing PCOS treatment over the long term can be a tough road for many, with adherence rates often falling short. Factors like high costs and complicated medication routines make it even harder for patients to stay consistent. Oana Health steps in to address these challenges head-on, offering a telehealth platform designed to make PCOS treatment more accessible and sustainable for patients.
Customized Treatment Plans
Oana Health creates tailored treatment plans to meet individual patient needs. Options include medications like Oral Metformin ER for $22 per month, a Metformin & Spironolactone combo for $32 per month, or Oral GLP-1 & Metformin therapy priced at $199 per month. This personalized care is especially important since combination therapies can lead to side effects like nausea and vomiting. To help patients manage these challenges, licensed medical professionals adjust doses gradually and provide guidance on proper medication use.
For those who prefer a more convenient dosing schedule, Oana Health offers once-weekly GLP-1 formulations, which have been shown to reduce the risk of non-adherence by 11% compared to daily injections. This approach pairs convenience with professional support, ensuring patients have the tools they need to stick with their treatment plans.
Easy Access and Professional Support
Through telehealth, Oana Health eliminates the need for in-person visits, while free shipping ensures medications arrive directly at patients' doorsteps. This is especially important when daily GLP-1 regimens face a high risk of discontinuation within just 120 days. Patients also benefit from ongoing support from licensed medical professionals who help manage side effects and provide guidance, keeping them on track. This consistent support is vital for reaching the 5–10% weight loss needed to improve ovulation and metabolic health in PCOS.
Affordable PCOS Medication Options
Cost is one of the biggest hurdles to staying on treatment. Oana Health addresses this by offering competitive pricing, such as Metformin for $22 per month and advanced combination therapy with Oral GLP-1 & Metformin for $199 per month. These prices are far more manageable compared to standard GLP-1 treatments, which can exceed $1,000 per month. For patients who experience side effects from oral medications, alternatives like Metformin HCL Lotion 20% are available for $43 per month. By combining telemedicine with compounding pharmacies, Oana Health reduces financial barriers, giving patients a better chance to stick with their treatment long enough to see meaningful improvements.
Conclusion
When it comes to treating PCOS, GLP-1 receptor agonists and Metformin show clear differences in how well patients stick to their prescribed regimens. Real-world data reveals that adherence rates for GLP-1 therapies are significantly lower than for Metformin, largely due to side effects both medications can cause. While GLP-1 therapies are known for achieving greater weight loss compared to controls, they often come with side effects like nausea, vomiting, and dizziness, which lead many patients to stop treatment prematurely.
The frequency of dosing also plays a big role in how likely patients are to continue their treatment. Weekly GLP-1 formulations tend to have better adherence rates compared to daily options. However, the steep annual cost of GLP-1 therapies remains a major obstacle for long-term use. These challenges highlight the importance of making treatments more convenient and offering robust patient support.
One promising option is combination therapy. Research shows that combining GLP-1 receptor agonists with Metformin can deliver better metabolic outcomes, such as improved insulin sensitivity and hormonal balance, without significantly increasing side effects. This strategy could help patients meet their treatment goals more effectively while addressing the limitations of each individual medication. The enhanced metabolic benefits of combination therapy make a strong case for providing structured patient support to maximize success.
For patients struggling with adherence, solutions like those offered by Oana Health can make a real difference. Their personalized care and telehealth services provide accessible options, including Oral Metformin ER for $22 per month and Oral GLP-1 & Metformin combination therapy for $199 per month. These plans not only offer medications but also professional support to help patients manage side effects and stay consistent with their treatment. For PCOS patients, the right mix of medication, support, and accessibility can pave the way for lasting results.
FAQs
Why do some patients struggle to stick with GLP-1 or Metformin for managing PCOS symptoms?
Adherence to GLP-1 receptor agonists and Metformin in managing PCOS can be tough, largely because of side effects like nausea, gastrointestinal discomfort, or an upset stomach. These unpleasant symptoms often make it hard for patients to stick with their prescribed regimen.
Another hurdle is the waiting period for noticeable results. Both medications typically need consistent use over weeks or even months before any significant changes become apparent, which can feel discouraging for some. On top of that, the daily routines required to take these medications can seem inconvenient, especially for those juggling busy schedules.
How do side effects influence the use of GLP-1 receptor agonists and Metformin for PCOS treatment?
Side effects play a big role in how well patients stick to treatments like GLP-1 receptor agonists and Metformin for managing PCOS. For GLP-1 receptor agonists, the most common side effects include nausea, vomiting, and mild diarrhea. These symptoms are usually temporary and don’t take away from the treatment’s benefits, such as weight loss and improved insulin sensitivity. In fact, many patients find the appetite-suppressing effects of GLP-1 to be worth the initial discomfort, especially with the convenience of once-weekly dosing.
Metformin, on the other hand, is known for causing more persistent gastrointestinal issues, such as diarrhea, abdominal cramps, and nausea. These side effects are frequent and often lead to patients lowering their dose or stopping the medication altogether. This can reduce its effectiveness in improving ovulation, balancing hormone levels, and supporting weight management in PCOS.
While both treatments offer benefits, GLP-1 receptor agonists generally have fewer side effects that patients find easier to tolerate, which leads to better adherence. Services like Oana Health’s telehealth platform can guide patients in managing these challenges and finding the treatment plan that works best for them.
What are the advantages of using GLP-1 receptor agonists with Metformin for PCOS treatment?
Combining GLP-1 receptor agonists (GLP-1 RAs) with Metformin has shown promising results for women with PCOS, especially in tackling weight management and improving both metabolic and reproductive health. Research highlights that this combination can lead to greater weight loss - typically around 5–10% of total body weight - compared to using Metformin on its own. This weight loss plays a key role in lowering insulin resistance, stabilizing blood sugar levels, and improving cholesterol and triglyceride levels.
Beyond metabolic improvements, this dual therapy also helps regulate hormones by balancing androgen levels. This hormonal shift often leads to more consistent menstrual cycles and better ovulation rates. The mechanism here is quite complementary: GLP-1 RAs work by reducing appetite, while Metformin decreases glucose production in the liver. Together, they allow for lower doses of each drug, minimizing side effects like gastrointestinal issues and making it easier for patients to stick to their treatment plan.
For women in the U.S. dealing with PCOS, this approach offers a more targeted way to address key symptoms like insulin resistance, while delivering meaningful improvements in both metabolic and reproductive health.
