How Pharmacogenomics Improves Hormonal Health
Pharmacogenomics (PGx) uses your DNA to personalize medication treatments, eliminating guesswork and reducing side effects. For hormonal health, this means better outcomes for conditions like PCOS, acne, hair loss, and menopause. Here's what you need to know:
- What it does: PGx identifies how your body processes medications based on your genes.
- Why it matters: Over 98% of people have genetic variations that affect drug metabolism, which can lead to ineffective treatments or harmful side effects.
- How it helps hormonal health: PGx optimizes medications like Metformin for PCOS, Spironolactone for acne, and hormone replacement therapy (HRT) for menopause.
- Getting started: A simple genetic test (cheek swab or saliva) provides lifelong insights to guide treatment decisions.
PGx is transforming hormonal health care by offering safer, more precise treatments tailored to your unique genetic profile.
Pharmacogenomics: A New Era of Patient-Centric Care
How Pharmacogenomics Works in Hormonal Health Treatment
Pharmacogenomic testing analyzes your DNA to uncover variations that influence how your body processes medications. These genetic differences, like single nucleotide polymorphisms (SNPs), remain consistent throughout your life, making a single test a resource you can rely on for years. This process revolves around two main mechanisms: pharmacokinetics (PK), which looks at how your body absorbs, breaks down, and eliminates a drug, and pharmacodynamics (PD), which focuses on how the drug interacts with its target in your body. Together, these mechanisms shed light on how your unique genetic makeup shapes your response to hormone therapies.
Many hormonal medications are metabolized by enzymes in the cytochrome P450 (CYP) system, particularly CYP2D6 and CYP2C19. Genetic testing can classify you as an ultra-rapid, normal, intermediate, or poor metabolizer. For instance, if you’re a poor metabolizer taking an SSRI, the medication may build up in your system, leading to side effects like QT interval prolongation. On the other hand, if you’re an ultra-rapid metabolizer, the drug may clear out too quickly to be effective.
"PGx is the future of medicine. I use it to bring precision to my prescribing. Now, I can more accurately predict adverse drug events, even outside of my specialty." - Jennifer Reed, FNP-BC, PMHNP-BC
These tests can also flag potential risks before they become serious. For example, testing for the F5 gene variant (rs6025) can reveal a higher risk of blood clots when using estrogen-containing contraceptives. Similarly, variations in the SLCO1B1 gene can indicate whether you’re likely to experience muscle pain from statins, which are sometimes used to manage metabolic symptoms associated with PCOS.
How Genes Affect Hormone Medication Response
Your genetic makeup plays a key role in determining how effective a medication will be and whether you’ll experience side effects. Variations in drug-metabolizing enzymes and transporters influence how quickly your body processes a medication. Plasma drug levels can differ by more than 1,000 times between two people of the same weight taking the same dose. This explains why some women with PCOS tolerate Metformin well, while others experience severe gastrointestinal issues.
The SLC22A1 gene is particularly relevant for Metformin, a common treatment for insulin resistance and PCOS. Variations in this gene affect how efficiently the drug enters cells, which can impact its ability to lower blood sugar. If testing reveals transport issues, your healthcare provider might adjust your dose or explore alternatives like GLP-1 agonists.
For mood-related symptoms tied to hormonal imbalances, CYP2C19 and CYP2D6 are crucial. These enzymes metabolize antidepressants like SSRIs, and genetic variations can determine whether the medication is effective or causes serious side effects. In fact, 95% of clinicians using pharmacogenetic testing report they can make safer, more confident treatment decisions.
This genetic insight allows for more precise management of specific hormonal conditions.
Hormonal Conditions That Benefit from Genetic Testing
Pharmacogenomic testing bridges genetic data with clinical care, offering tailored treatments for various hormonal health concerns.
PCOS and insulin resistance are among the top conditions where this testing shines. Beyond its role in optimizing Metformin dosing, testing can guide the use of Spironolactone for acne and hirsutism, helping predict risks like electrolyte imbalances. Women with PCOS taking statins can also benefit from SLCO1B1 testing to minimize muscle-related side effects.
For acne and hair loss, genetic testing can refine treatments. Medications like Spironolactone and Minoxidil work differently depending on your genetic profile, helping doctors fine-tune dosages for better outcomes.
Women exploring hormone replacement therapy (HRT) or contraceptives can gain critical safety insights from genetic testing. For instance, variations in CYP3A5 can affect how your body processes glucocorticoids (steroids), with poor metabolizers being at risk for severe side effects like rapid weight gain or Cushing’s syndrome.
As Victoria Rollinson and her colleagues explain:
"Genomic variation in genes involved in a drug's absorption, distribution, metabolism and elimination... can alter a drug's PK profile, influencing systemic exposure and resulting in altered drug response."
The FDA has embraced this personalized approach, noting that over 270 medications now include warnings, dosage guidelines, or drug interaction advice based on specific genetic variants. When it comes to hormonal health, this means fewer side effects and quicker paths to effective treatments.
Personalized Treatment Approaches for Specific Conditions
Pharmacogenomics is transforming the way we approach hormonal health treatments by replacing guesswork with genetic insights to guide medication choices.
PCOS and Insulin Resistance: Tailoring Metformin and GLP-1 Agonist Doses
Polycystic ovary syndrome (PCOS) affects around 10%–13% of women of reproductive age, with many also grappling with insulin resistance. Metformin is often the go-to treatment for managing PCOS-related metabolic issues, but how well it works can depend on genetic factors.
For example, variations in the OCT1 gene can influence metformin's effectiveness. Women with PCOS also face a significantly higher lifetime risk - 4 to 7 times greater - of developing type 2 diabetes. This underscores the need for personalized dosing strategies to optimize outcomes.
"Metformin can be a helpful part of treatment for some women with PCOS, especially those with insulin resistance or certain pregnancy risks. Still, it is not a one-size-fits-all solution." - Saeede Saadati et al.
When metformin and lifestyle changes aren’t enough, GLP-1 receptor agonists like semaglutide or liraglutide offer a strong second-line option. These medications can be introduced with gradual dose increases to reduce gastrointestinal side effects. Companies like Oana Health provide oral GLP-1 combined with Metformin for $199/month, with licensed professionals overseeing prescriptions and home delivery.
Acne and Hair Loss: Adjusting Spironolactone and Minoxidil Treatments
For conditions like acne and hair loss, pharmacogenomics fine-tunes anti-androgen therapies. Spironolactone, for instance, works by blocking androgen receptors, which helps reduce the effects of DHT, a hormone linked to both acne and hair loss. Genetic variations in these receptors can affect how well the treatment works.
Genetic testing can guide dosage adjustments to enhance treatment effectiveness. Similarly, the success of minoxidil for hair loss depends on genetic factors that influence how the body absorbs and metabolizes the drug. Oana Health offers oral Minoxidil starting at $25/month and topical Spironolactone for $43/month, both tailored to individual needs.
Menopause and Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) during menopause often requires highly individualized dosing, as women can respond very differently to estrogen levels needed for symptom relief. Pharmacogenomics helps identify genetic variants in enzymes responsible for hormone metabolism, allowing for treatments that are both effective and less likely to cause side effects.
"Personalized management of menopausal symptoms and other menopause-related disorders should be based, among other variables, on pharmacogenomics." - Amos Pines, Sackler School of Medicine, Tel-Aviv University
For example, testing for the F5 gene variant (rs6025), also called Factor V Leiden, can pinpoint women at higher risk for venous thromboembolism when using systemic estrogen. Research like the Kronos Early Estrogen Prevention Study (KEEPS) has examined how single nucleotide polymorphisms (SNPs) impact cardiovascular health in women undergoing HRT. Over four years, the study found that SNPs in the innate immunity pathway influenced cardiovascular outcomes, showing how genetic testing can predict long-term health effects beyond immediate symptom management.
These tailored approaches are paving the way for pharmacogenomics to become an integral part of hormonal health care, offering treatments that align closely with each individual’s genetic profile.
sbb-itb-6dba428
How to Add Pharmacogenomics to Your Treatment Plan
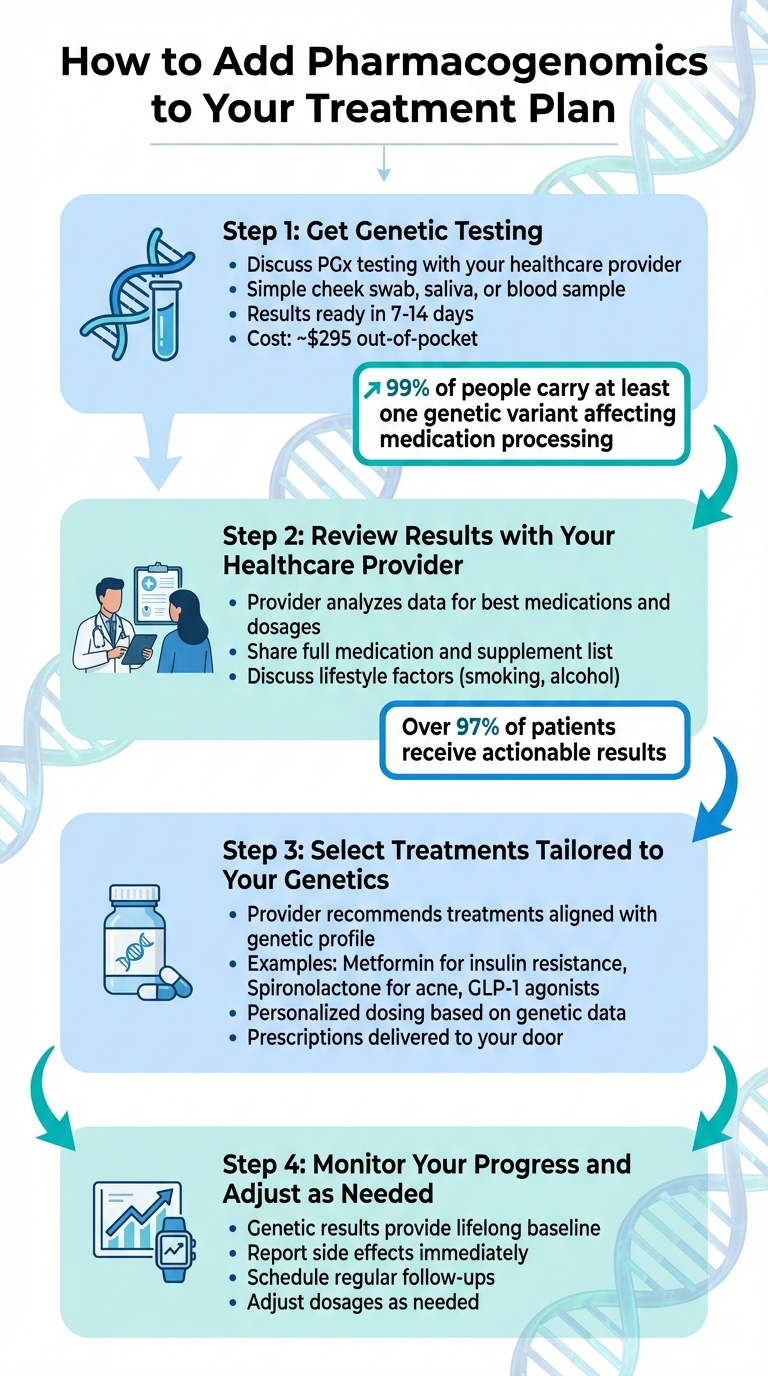
4 Steps to Add Pharmacogenomics to Your Hormonal Health Treatment Plan
Integrating genetic testing into your hormonal health care involves four straightforward steps. These steps help tailor your treatment plan based on your unique genetic makeup, ensuring medications are as effective as possible.
Step 1: Get Genetic Testing
Start by discussing pharmacogenomic (PGx) testing with your healthcare provider. This step is crucial because nearly 99% of people carry at least one genetic variant that can influence how their body processes medications. PGx tests are simple and use a cheek swab, saliva, or blood sample.
Once the lab receives your sample, results are typically ready in 7 to 14 days. If you’re using a telehealth service, you can even have a collection kit sent directly to your home. Before proceeding, check your insurance coverage. If paying out-of-pocket, expect the cost to be around $295.
Step 2: Review Results with Your Healthcare Provider
When your results are ready, your provider will analyze the data to identify the best medications and dosages for you. This step is critical because over 97% of patients who undergo PGx testing receive actionable results that impact their treatment or dosing.
Make sure to share a full list of all your current medications and supplements during this review. Be upfront about your lifestyle habits, like smoking or alcohol use, as these can affect how your body metabolizes medications [2,25]. Your provider will explain whether your current treatments are effective, if dosage adjustments are necessary, or if any medications pose a higher risk of side effects. This discussion lays the groundwork for a personalized treatment plan.
Step 3: Select Treatments Tailored to Your Genetics
Using your genetic test results, your provider can recommend treatments that align with your genetic profile. For example, they might adjust metformin for insulin resistance, modify spironolactone dosing for acne or unwanted hair, or choose the most suitable GLP-1 agonist for your needs.
Oana Health offers a range of personalized treatment options delivered right to your door with free shipping. These include:
- Oral GLP-1 & Metformin for managing PCOS at $199/month
- Oral Minoxidil for hair loss starting at $25/month
- Topical Spironolactone for $43/month
All prescriptions are carefully reviewed by licensed medical professionals who consider both your genetic data and medical history.
Step 4: Monitor Your Progress and Adjust as Needed
Your genetic results provide a baseline for life, but ongoing monitoring is key to ensuring your treatment remains effective. If you notice side effects, report them immediately. For instance, if your body metabolizes a medication too slowly due to a genetic variant, you might need a lower dose to avoid side effects.
"If your body breaks down a medication too quickly, too slowly or not at all, then a typical dose of it won't work as intended." - Cleveland Clinic
Schedule regular follow-ups with your provider to track your progress and make any necessary adjustments. Many telehealth platforms make this process convenient with quick online consultations. By staying proactive, you can ensure your treatment continues to work for you.
Benefits of Using Pharmacogenomics for Hormonal Health
Better Results and Fewer Side Effects
Genetic testing takes the guesswork out of prescribing by helping doctors pinpoint the right medication and dosage from the start. Research shows that treatments guided by pharmacogenomics (PGx) reduce adverse reactions from 27.7% to 21% in general cases. Severe toxicity rates drop dramatically too - from 73% to 28% - which significantly lowers the risk of drug-induced fatalities.
"By customizing medication regimens to align with each patient's unique genetic profile, pharmacogenomics minimizes the risk of adverse reactions and maximizes therapeutic benefits."
– James Wallace, CEO, DecisionRx
This tailored approach is especially beneficial for hormonal therapies. Identifying genetic variations ahead of time helps avoid ineffective treatments and dosing problems that can cause unwanted side effects or poor results. By addressing these issues upfront, patients experience better outcomes and quicker access to effective care.
More Convenient Access Through Telehealth
The combination of safer, more effective treatments with telehealth creates a new level of convenience. Now, pharmacogenomic testing doesn’t even require a clinic visit. With telehealth platforms, you can order an at-home kit, collect a cheek swab or saliva sample, and have your results evaluated by a licensed provider - all from the comfort of your home.
For example, Oana Health offers a fully streamlined process. After reviewing your genetic results and medical history, your provider can prescribe the optimal treatment, which is then shipped directly to your door with free delivery. This is especially helpful for managing chronic conditions like PCOS, where ongoing adjustments to medication are often required.
On top of improving care, pharmacogenomic-guided therapy can save patients over $3,600 annually by reducing unnecessary hospital visits, emergency room trips, and wasted prescriptions.
Conclusion
Pharmacogenomics is changing the game by replacing the old trial-and-error method with treatments tailored to your DNA. This means healthcare providers can prescribe the right medication at the right dose from the very beginning. It’s a shift toward precision that ensures treatment plans are optimized from day one.
Experts are highlighting this transformation in medicine.
"Pharmacogenomics represents a paradigm shift in drug therapy, offering the promise of personalized medicine tailored to the individual genetic makeup of each patient."
– Maria Garcia, Department of Clinical Pharmacy, Harvard Medical School
The benefits? Fewer side effects, better results, and reduced costs. For conditions like PCOS, insulin resistance, and menopause, genetic testing can pinpoint the most effective treatments - whether it’s Metformin, Spironolactone, or the right hormone replacement therapy.
Platforms like Oana Health make this personalized care more accessible than ever. With at-home genetic testing, remote consultations with licensed providers, and customized treatments shipped straight to your door, telehealth is breaking down barriers. This is especially helpful for managing chronic hormonal conditions that require ongoing adjustments.
Pharmacogenomics offers a straightforward solution for achieving better hormonal health. It eliminates the frustration of ineffective medications or unwanted side effects, giving you the tools to take control of your health.
FAQs
How does pharmacogenomics enhance treatment for hormonal conditions like PCOS and menopause?
Pharmacogenomics takes a closer look at your genetic blueprint to customize treatments for hormonal conditions like PCOS and menopause. By examining how your genes influence drug metabolism and hormone responses, healthcare providers can pinpoint the medications that work best for you and fine-tune the dosage to match your needs.
This tailored approach can make treatments more effective - whether it's estrogen therapy for menopause or insulin-sensitizing drugs for PCOS - while also lowering the chances of unpleasant side effects. Essentially, it creates a treatment plan that's as individual as your genetic profile, offering a targeted and science-driven way to support your hormonal health.
How can pharmacogenomic testing help address hormonal health issues, and what steps are involved?
Pharmacogenomic testing offers a personalized way to address hormonal health challenges like PCOS, insulin resistance, and acne. By analyzing your genetic profile, it helps pinpoint the medications and dosages that are most likely to work for your body, cutting down on the guesswork often involved in treatment.
Here’s how the process works:
- Talk to a healthcare provider: Book a virtual appointment with an Oana Health clinician to discuss your hormonal health concerns and see if pharmacogenomic testing is a good fit for you.
- Submit a DNA sample: A simple cheek swab is all it takes. The sample is then sent to a lab for analysis.
- Get personalized treatment: Once your results are in, your provider will review the genetic findings alongside your health history. From there, they’ll design a treatment plan tailored specifically to your needs, which could include prescription therapies.
This approach not only enhances treatment effectiveness but also provides a genetic roadmap you can rely on for managing hormonal health throughout your life.
How does my DNA impact how hormonal medications work for me?
Your DNA holds the blueprint for how your body handles hormonal medications. Variations in your genetic code - like differences in the enzymes that break down hormones or in the genes responsible for hormone receptors - can influence how quickly a medication is processed, how efficiently it reaches its target, and how well it interacts with receptors.
These genetic variations can impact not only how effective a medication is for you but also whether you're more likely to experience side effects. By using pharmacogenomics to analyze your genetic profile, treatments can be tailored specifically to your needs, making them both safer and more effective.
