Intermittent Fasting and Insulin Sensitivity
Intermittent fasting (IF) and regular meal schedules are two dietary approaches often debated for improving insulin sensitivity, blood sugar control, and weight management. Here's the breakdown:
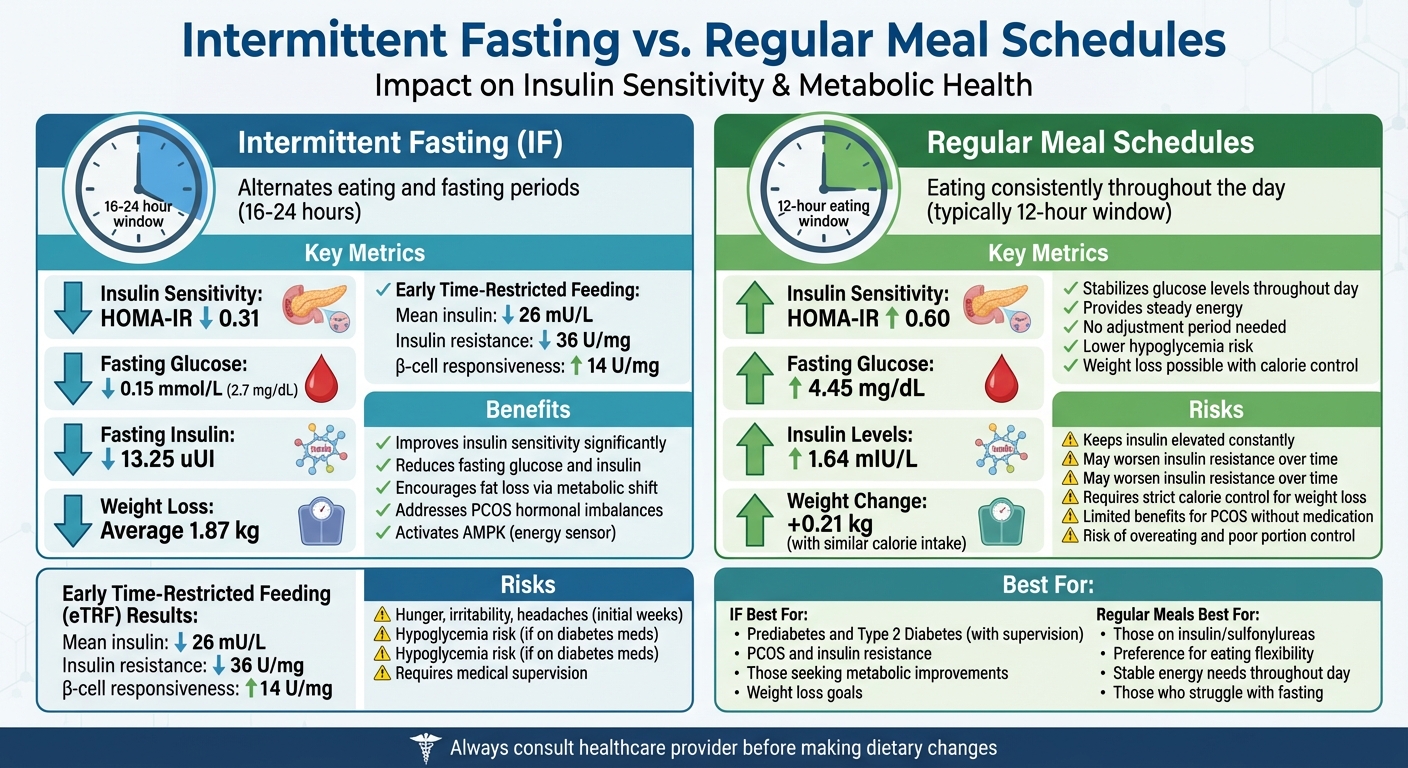
- Intermittent Fasting (IF): Alternates eating and fasting periods, typically within 16–24 hours. It reduces insulin levels, improves insulin sensitivity, and supports weight loss by encouraging the body to burn fat for energy. Early time-restricted feeding (eTRF), where meals end by mid-afternoon, aligns with the body's natural insulin response, showing measurable benefits in studies.
- Regular Meal Schedules: Involves eating consistently throughout the day, often in a 12-hour window. It stabilizes glucose levels but keeps insulin elevated, which may worsen insulin resistance over time. Weight loss is achievable but often requires strict calorie control.
Key Findings:
- IF lowers fasting glucose, insulin levels, and HOMA-IR (a marker of insulin resistance).
- Regular meal schedules are less effective for reversing insulin resistance but provide steady energy throughout the day.
- For conditions like PCOS, IF may better address hormonal imbalances, but both approaches require careful planning and medical guidance.
Quick Comparison:
| Criteria | Intermittent Fasting (IF) | Regular Meal Schedules |
|---|---|---|
| Insulin Sensitivity | Improves significantly (e.g., HOMA-IR ↓) | Maintains but less effective |
| Blood Sugar Control | Reduces fasting glucose and insulin | Stabilizes but less impactful |
| Weight Management | Encourages fat loss via metabolic shift | Relies on calorie control |
| PCOS Benefits | Addresses insulin resistance, hormones | Limited benefits without medication |
| Risks | Hunger, hypoglycemia (if unmanaged) | Overeating, sustained high insulin |
Both approaches have pros and cons, and the best choice depends on individual health needs, lifestyle, and medical conditions. Always consult with a healthcare provider before making major dietary changes.
Intermittent Fasting vs Regular Meal Schedules: Impact on Insulin Sensitivity and Metabolic Health
1. Intermittent Fasting
Impact on Insulin Sensitivity
Intermittent fasting triggers a metabolic reprogramming process, where your body shifts from using glucose to burning fatty acids and ketone bodies as its primary energy source. This metabolic adjustment activates AMP-activated protein kinase (AMPK), a key energy sensor in your cells. AMPK becomes active during periods of low energy, helping to restore glucose balance and improve how your cells respond to insulin. This change creates the foundation for dietary methods like early time-restricted feeding.
The timing of your eating window plays a crucial role. Early time-restricted feeding (eTRF) - which involves finishing your meals by mid-afternoon - works in harmony with your body's natural circadian rhythms, as insulin sensitivity tends to peak in the morning. In May 2018, researchers from the Pennington Biomedical Research Center, led by Dr. Elizabeth Sutton and Dr. Courtney Peterson, conducted a five-week study involving men with prediabetes. Participants adhered to a 6-hour eating window, ending their meals by 3:00 PM. The results? eTRF reduced mean insulin levels by 26 mU/l and decreased insulin resistance by 36 U/mg.
"We demonstrate for the first time in humans that eTRF improves some aspects of cardiometabolic health and IF's effects are not solely due to weight loss." - Dr. Courtney M. Peterson, University of Alabama at Birmingham
Effect on Blood Sugar Levels
Intermittent fasting enhances cellular responses, leading to lower daily insulin levels and improved pancreatic function, which directly supports better blood sugar regulation. While IF may not significantly alter fasting glucose levels in healthy individuals, it does reduce daily insulin levels and strengthens the pancreas's ability to manage blood sugar changes. A meta-analysis revealed that IF lowered fasting blood glucose by an average of 0.15 mmol/L, fasting insulin by 13.25 uUI, and HOMA-IR (a marker of insulin resistance) by 0.31. These improvements in metabolic markers build up over time, contributing to overall better health.
Weight Management Benefits
Intermittent fasting also supports weight management by making it easier for the body to tap into stored fat for energy. According to the same meta-analysis, participants practicing IF lost an average of 4.1 pounds (1.87 kg) and reduced their waist circumference by 0.8 inches (2.08 cm). In a 2018 case series led by Dr. Furmli, three patients with Type 2 Diabetes who incorporated three 24-hour fasts per week were able to completely stop using insulin therapy within just one month, all while experiencing substantial weight loss.
Applicability to PCOS and Insulin Resistance
For women with PCOS, intermittent fasting can be particularly beneficial. Lowering insulin levels not only improves metabolic health but also helps balance hormones, addressing symptoms such as irregular periods, excessive hair growth, and weight challenges. Victoria Della Rocca, RD and Nutrition Director, explains:
"Intermittent fasting can help people with PCOS control their insulin levels, balance their hormones and therefore improve their health and the symptoms of their disease"
That said, women with PCOS or diabetes should consult healthcare professionals before starting IF. Proper guidance is essential to manage medication adjustments and avoid risks like hypoglycemia. Oana Health provides personalized telehealth consultations and evidence-based treatments for insulin resistance and PCOS management. Their licensed professionals can help determine if intermittent fasting is a suitable option for your specific needs. Up next, we’ll look at how these results compare to regular meal schedules.
2. Regular Meal Schedules
Impact on Insulin Sensitivity
In the United States, most people eat within a 12-hour window each day. This habit keeps the body in a near-constant state of insulin production. Here’s how it works: every time you eat, your pancreas releases insulin to help your cells absorb glucose. When meals and snacks are spread throughout the day, insulin levels stay elevated, which can make cells less responsive to the hormone over time. This reduced sensitivity forces the body to produce even more insulin. A 26-week study found that participants on a regular eating schedule saw their HOMA-IR (a measure of insulin resistance) rise by 0.60, while their insulin levels increased by 1.64 mIU/L.
Between 2016 and 2018, researchers at the Pennington Biomedical Research Center, led by Dr. Elizabeth F. Sutton, used a 12-hour eating window as their baseline to test early time-restricted feeding. While a regular eating schedule kept metabolic markers stable, it didn’t show the same improvements in insulin sensitivity or blood pressure seen with more restrictive eating windows. This constant insulin stimulation lays the groundwork for challenges in blood sugar management, which we’ll explore next.
Effect on Blood Sugar Levels
Continuous eating patterns also make it harder to regulate blood sugar. In the same 26-week trial, fasting blood glucose levels in the regular eating group increased by 4.45 mg/dL, while the intermittent fasting group saw a decrease of 9.13 mg/dL. Interestingly, the body’s insulin sensitivity peaks in the morning and gradually declines as the day progresses. Eating late at night disrupts this natural rhythm, making blood sugar control even tougher.
For individuals with PCOS, the stakes are even higher. Elevated insulin levels can trigger the ovaries to produce excess testosterone, worsening hormonal imbalances and menstrual irregularities. Constant snacking, by keeping insulin levels elevated, can make managing these symptoms even more difficult.
Weight Management Benefits
When total calories are controlled, regular meal schedules can help maintain or even reduce weight. Studies suggest that calorie control through regular meals can achieve weight loss results similar to intermittent fasting. However, the quality of food matters just as much as the timing. For example, starting your day with a protein-packed breakfast like an omelet can keep you fuller and stabilize blood sugar better than high-carb options like bagels or cereal.
Dr. Janine Kyrillos, Director of Comprehensive Weight Management, emphasizes this point:
"When you lower calories without addressing the type of food, it's very difficult to sustain and can eventually lower metabolism and increase hunger levels." – Dr. Janine Kyrillos
That said, maintaining a calorie deficit over time can be challenging. In the 26-week study, participants following a regular eating schedule gained 0.21 kg, while those practicing intermittent fasting lost 1.74 kg.
Applicability to PCOS and Insulin Resistance
For women managing PCOS or insulin resistance, regular meal schedules require a thoughtful approach to both food quality and timing. Nutrition expert Victoria Della Rocca, RD, highlights the importance of personalization:
"No matter what, we always focus on nourishing the body first. We intentionally co-create a strategy with patients to continually explore and figure out what the body needs and when it needs it." – Victoria Della Rocca, RD
The main challenge with regular eating patterns for PCOS is the persistent insulin stimulation. Without giving the body extended periods of low insulin, it’s harder to address the hormonal imbalances that drive PCOS symptoms. A well-planned meal schedule that prioritizes nutrient-dense foods and aligns with the body’s natural rhythms - such as eating more calories at breakfast and fewer at dinner - can offer metabolic advantages. That said, the constant insulin stimulation from this pattern might limit long-term benefits for those dealing with insulin resistance. Platforms like Oana Health can provide tailored guidance to help you find the eating approach that works best for your metabolic needs and lifestyle.
Intermittent Fasting: Effects on Body Weight and Blood Sugar Regulation
sbb-itb-6dba428
Advantages and Disadvantages
Let’s take a closer look at the pros and cons of intermittent fasting (IF) and regular meal schedules, especially in terms of insulin sensitivity, blood sugar control, and weight management.
Intermittent Fasting
Research shows that intermittent fasting can significantly benefit metabolic health. For example, a study on men with prediabetes found that early time-restricted feeding - where all meals are consumed within a 6-hour window, with dinner before 3:00 PM - reduced average insulin levels by 26 ± 9 mU/L and improved β-cell responsiveness by 14 ± 7 U/mg, even without notable weight loss. The metabolic switch triggered by IF plays a key role in improving insulin sensitivity.
However, the first few weeks of IF can be tough. Hunger, irritability, and headaches are common as your body adjusts. For individuals on diabetes medications, fasting without proper monitoring can lead to dangerously low blood sugar levels.
Regular Meal Schedules
Regular meal schedules provide stability, as they maintain steady glucose levels throughout the day. They don’t require an adjustment period, which minimizes the risk of hypoglycemia for those not on medications.
On the flip side, constant eating can keep insulin levels elevated, potentially worsening insulin resistance over time. While weight loss is achievable through calorie restriction on a regular eating plan, it often demands careful portion control and disciplined food choices. For women with PCOS, regular eating patterns alone may not effectively address hormonal imbalances unless paired with targeted medical treatments.
Comparison Table
Here’s a side-by-side breakdown of how these two approaches stack up:
| Criteria | Intermittent Fasting (IF) | Regular Meal Schedules |
|---|---|---|
| Insulin Sensitivity | Lowers HOMA-IR by 0.31 and improves β-cell responsiveness | Maintains sensitivity but is less effective at reversing hyperinsulinemia |
| Blood Sugar Control | Reduces fasting glucose by 0.15 mmol/L and lowers HbA1c levels | Keeps glucose levels consistent but with less impact on baseline reduction |
| Weight Management | Encourages fat loss through metabolic switching; average weight loss of 1.87 kg | Relies on strict calorie counting for similar results |
| PCOS Applicability | Helps address insulin resistance and hormonal imbalances with medical support | Less effective for hormonal regulation without medication |
| Risks | Hunger, irritability, and hypoglycemia risk for those on diabetes meds; one study links eating windows under 8 hours to a 135% higher cardiovascular death risk | Overeating, poor portion control, and sustained high insulin levels |
Key Takeaway
For women with PCOS or insulin resistance, personalized plans are essential. Platforms like Oana Health can provide tailored strategies and integrate treatments like Metformin or GLP-1 medications to enhance metabolic outcomes.
Conclusion
Intermittent fasting has shown measurable benefits, such as lowering HOMA-IR by 0.31 and reducing fasting glucose by 0.15 mmol/L (around 2.7 mg/dL). On the other hand, sticking to regular meal schedules offers consistent nutritional support and lowers the risk of hypoglycemia. Deciding between these approaches depends heavily on your medications, lifestyle, and specific metabolic markers. For individuals managing conditions like PCOS or type 2 diabetes, this decision must be tailored to your unique health and medication needs.
If you're using insulin or sulfonylureas, intermittent fasting requires careful planning and close medical supervision to prevent hypoglycemia risks. This is a critical consideration when exploring any dietary changes.
Your metabolic markers and daily rhythms play a major role in how your body responds to fasting. Platforms like Oana Health provide personalized treatment plans that combine prescription medications - such as Metformin or GLP-1 therapies - with customized dietary strategies. These plans aim to address insulin resistance, regulate hormones, and promote sustainable weight loss.
Before making any changes, consult with a healthcare provider who can evaluate your individual health profile and guide you toward the best approach for your body.
FAQs
How does intermittent fasting help improve insulin sensitivity compared to eating on a regular schedule?
Intermittent fasting has been shown to improve how the body handles insulin by reducing fasting insulin levels and triggering cellular repair mechanisms. These shifts can lead to a noticeable decrease in insulin resistance, often surpassing the effects of traditional eating patterns - even without factoring in weight loss.
When you extend the time between meals, your body gets a chance to let insulin levels drop naturally. This process helps cells become more responsive to insulin over time, which can play a key role in managing blood sugar levels and promoting better metabolic health.
What are the benefits of early time-restricted feeding for individuals with insulin resistance?
Early time-restricted feeding (eTRF) offers a range of benefits for individuals dealing with insulin resistance. By improving insulin sensitivity and promoting healthier beta-cell function, it helps the body regulate blood sugar more efficiently. On top of that, eTRF has been linked to lower blood pressure, reduced oxidative stress, and a diminished evening appetite - all of which support better metabolic health, even without weight loss.
This method is especially useful for those managing conditions like prediabetes or insulin resistance. By working in harmony with the body's natural circadian rhythms, eTRF enhances metabolic processes and helps the body function more effectively.
Can intermittent fasting be risky for people taking diabetes medication?
Intermittent fasting can be risky for people taking diabetes medication. Without the right medical guidance, fasting might cause dangerous drops in blood sugar levels (hypoglycemia) or lead to other complications. This happens because many diabetes medications are designed to regulate blood sugar based on consistent meal schedules.
If you're on diabetes medication and thinking about trying intermittent fasting, it's essential to talk to your healthcare provider first. They can evaluate your unique situation and adjust your treatment plan to keep you safe while considering fasting as a way to improve insulin sensitivity.
