5 Ways Menstrual Cycle Impacts Mental Health
Your menstrual cycle affects more than just your body - it can significantly influence your mental health. Hormonal changes throughout the cycle impact mood, anxiety, stress levels, and even existing mental health conditions. Here's a quick breakdown:
- Depression and Low Mood Before Your Period: Hormone drops, especially estrogen, can trigger depressive symptoms and energy loss.
- Increased Anxiety and Stress Sensitivity: Heightened amygdala activity during the luteal phase can worsen anxiety and stress.
- Worsening Psychotic Symptoms: Women with schizophrenia often experience more intense symptoms during specific cycle phases.
- Higher Suicide Risk: The perimenstrual phase sees a notable rise in suicide risk due to hormonal fluctuations.
- Impact on Other Conditions: Disorders like bipolar disorder, panic attacks, migraines, and more can worsen during hormonal shifts.
Tracking your cycle and symptoms can help identify patterns and guide effective treatment options. If these changes disrupt daily life, consult a healthcare provider for support.
Why Anxiety Spikes During PMS | The Menstrual Cycle's Impact On Women's Mental Health
How Hormones Affect Mental Health Throughout Your Cycle
How Hormones Affect Mental Health Throughout Your Menstrual Cycle
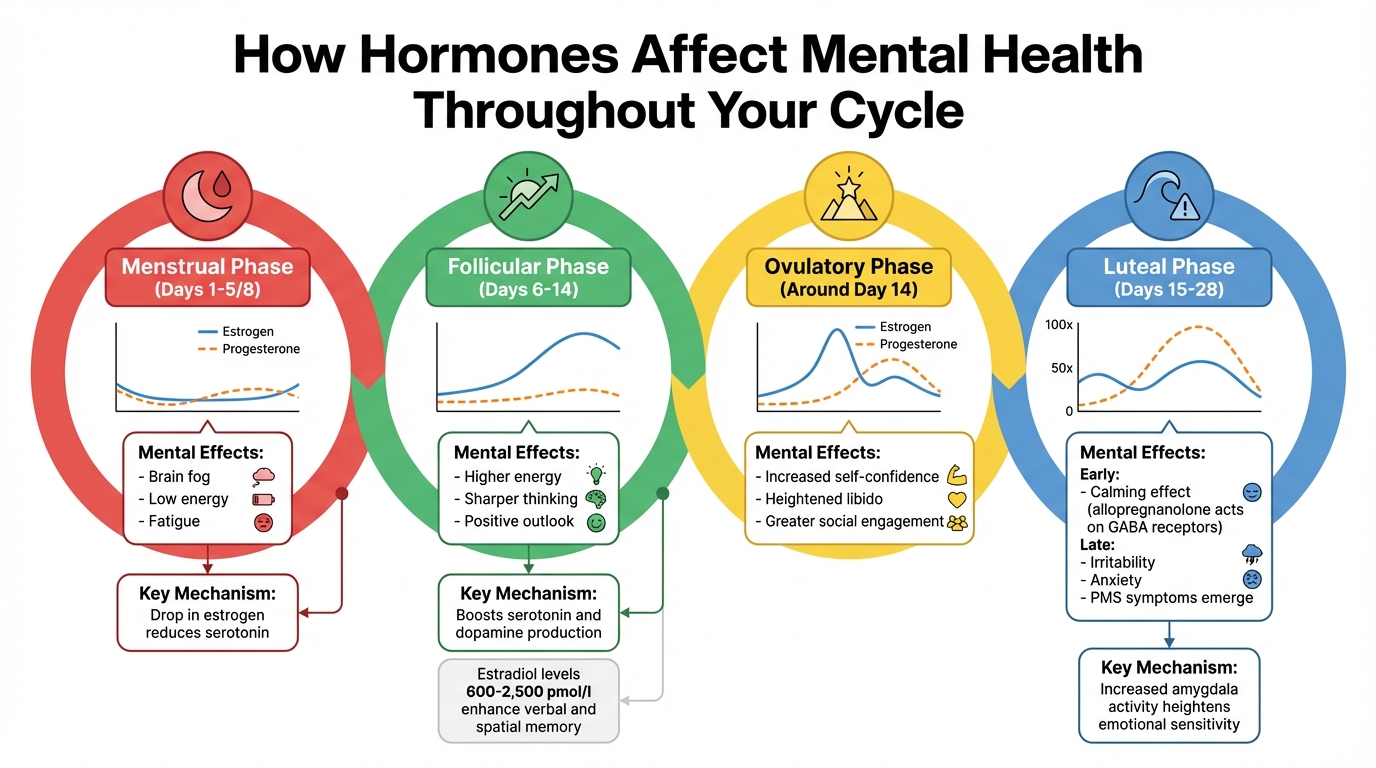
Your menstrual cycle has four distinct phases, each bringing hormonal changes that can influence your mood and mental clarity.
The menstrual phase (days 1–5 or 8) begins when estrogen and progesterone levels hit their lowest point. This drop in estrogen reduces serotonin, a neurotransmitter that plays a big role in maintaining a positive mood. As a result, you might experience brain fog, low energy, and fatigue during this time.
In the follicular phase (days 6–14), estrogen levels gradually climb, which boosts serotonin and dopamine production. This increase often leads to higher energy levels, sharper thinking, and a more positive outlook. Research indicates that elevated estradiol levels - ranging between 600 and 2,500 pmol/l during the pre-ovulatory surge - can enhance performance in tasks requiring verbal and spatial memory.
The ovulatory phase (around day 14) is marked by a peak in both estrogen and testosterone. This hormonal surge can lead to increased self-confidence, heightened libido, and greater social engagement.
The luteal phase (days 15–28) sees a significant rise in progesterone, which can be nearly 100 times higher than estradiol during this phase. Initially, progesterone’s metabolite, allopregnanolone, has a calming effect by acting on GABA receptors. However, as hormone levels drop toward the end of the phase, irritability, anxiety, and other PMS symptoms may emerge. Additionally, this phase is associated with increased activity in the amygdala, which can heighten emotional sensitivity and make stress feel more intense.
1. Depression and Low Mood Before Your Period
In the week leading up to your period, your body undergoes rapid hormonal changes, with estrogen and progesterone levels dropping sharply. This decline can trigger depressive symptoms and a noticeable dip in mood. One of the main culprits is estrogen withdrawal, which plays a significant role in depression among women. When estrogen levels drop, it prompts the release of norepinephrine, which then reduces key neurotransmitters like serotonin, dopamine, and acetylcholine. The result? Increased fatigue and feelings of depression. Beyond that, this hormonal shift affects brain areas responsible for managing emotions, leading to a decline in motivation and pleasure as the brain's reward system becomes less responsive. For some women, these changes can create a foundation for more serious mental health challenges.
In certain cases, these shifts escalate into clinical conditions. For instance, Premenstrual Dysphoric Disorder (PMDD) - a severe form of premenstrual syndrome - affects about 3% to 8% of women of reproductive age. Symptoms of PMDD include overwhelming despair, intense anger, and even suicidal thoughts, making it difficult to maintain relationships, perform at work, or manage daily responsibilities.
"Symptoms of PMDD are so severe that people have trouble functioning at home, at work, and in relationships during this time. This is markedly different than other times during the month." - Johns Hopkins Medicine
Women with existing mood disorders often find their symptoms worsen during this time. This phenomenon, known as Premenstrual Exacerbation (PME), affects roughly 60% of women with major depressive or bipolar disorder and over half of those with other mood issues. To better understand and manage these patterns, tracking your symptoms daily for at least two menstrual cycles can be incredibly helpful. This information can guide you and your healthcare provider in finding the most effective treatment plan.
2. Increased Anxiety and Stress Sensitivity
The hormonal shifts during the mid-luteal phase can lead to heightened anxiety. As progesterone levels rise, the amygdala becomes more active and its connection with the prefrontal cortex strengthens. This combination often results in repetitive worrying and an increase in negative thought patterns. These changes in the central nervous system aren’t just mental - they can show up as physical symptoms too.
Many women report experiencing a racing heartbeat, trouble sleeping, restlessness, and being unusually sensitive to noise during this phase. Later in the luteal phase, as hormone levels drop, the composition of GABA receptors changes, which reduces their calming effects and makes stress feel even more overwhelming.
Stress can also push progesterone to convert into cortisol, the body’s primary stress hormone. This can intensify the stress response and make emotional regulation more challenging. For women with existing anxiety disorders, this hormonal interaction may lead to Premenstrual Exacerbation (PME), where anxiety symptoms become significantly worse in the week leading up to menstruation.
"The window of vulnerability model proposes that natural increases in ovarian hormones in the mid-luteal phase of the menstrual cycle lead to systematic changes in brain networks associated with affective processing." - ScienceDirect
Recognizing these hormonal patterns can help you pinpoint when anxiety may peak, making it easier to manage stress effectively. Tracking your symptoms over two or three cycles can reveal your most vulnerable times. During the luteal phase, practices like mindfulness, yoga, or relaxation exercises may help you stay grounded. If anxiety starts to disrupt your daily life, consider discussing options like SSRIs or hormonal therapies with your healthcare provider. For personalized support in managing these hormonal changes and their effects on mental health, Oana Health offers telehealth consultations with licensed professionals who specialize in this area.
3. Worsening Psychotic Symptoms in Women with Schizophrenia
For women with schizophrenia, psychotic symptoms often intensify during specific phases of the menstrual cycle. Research highlights that 32.4% of women with schizophrenia experience a cyclical worsening of psychotic symptoms. This connection is tied to estrogen's influence on dopamine pathways.
Estrogen plays a critical role by naturally reducing dopamine transmission, functioning in a way similar to many antipsychotic medications. However, during the late luteal and menstrual phases, estrogen levels drop, which weakens this protective effect. This hormonal shift can lead to increased risks of hallucinations, paranoia, and other psychotic symptoms. In fact, studies show that hospital admission rates for women with schizophrenia are 1.48 times higher during the perimenstrual phase, the days surrounding the start of a period.
"Estrogen downregulates dopamine transmission, which mimics the antidopaminergic action of many antipsychotic medications."
- Ariel B. Handy, PhD, Harvard Medical School
The timing of symptoms is also significant. Positive symptoms, such as excitability or hostility, tend to peak in the days leading up to menstruation, while negative symptoms, like social withdrawal, are more prominent during menstruation itself. Additionally, positron emission tomography (PET) scans reveal that dopamine D2 receptor sensitivity in the striatum is about 12% higher during the luteal phase compared to the follicular phase. These findings underline the importance of tracking symptom patterns across different phases of the cycle.
Given these hormonal effects, monitoring symptoms in relation to the menstrual cycle can be a valuable tool. Keeping a detailed diary of symptoms and sharing it with a healthcare provider can help identify patterns and inform treatment decisions. Adjustments to antipsychotic medications or exploring options like estrogen augmentation therapy may be considered. For women managing the dual challenges of hormonal shifts and schizophrenia, resources like Oana Health provide telehealth consultations with licensed professionals who specialize in these complex interactions.
sbb-itb-6dba428
4. Higher Suicide Risk During Perimenstrual Phases
The days around menstruation carry an increased risk of suicide. Studies reveal a 26% higher risk of suicide deaths and a 17% higher risk of suicide attempts during the menstrual phase. Autopsy findings indicate that 25% to 54% of female suicides occur during menstruation.
This heightened risk is largely tied to hormonal changes. As estrogen levels drop right before and during menstruation, this decline can lead to depression, loss of interest, and cognitive difficulties. Additionally, low progesterone levels in the early follicular phase are associated with increased feelings of "perceived burdensomeness" - the belief that others would be better off without you. For women already struggling with mental health challenges, this time can be especially difficult. Research shows that psychiatric admissions rise by 20% during menstruation and by 13% in the premenstrual phase.
Women with existing mental health conditions face even greater risks. Those with a history of psychiatric diagnoses are five times more likely to attempt suicide during the menstrual phase compared to those without such a history. Among women diagnosed with Premenstrual Dysphoric Disorder (PMDD), 71.6% report experiencing suicidal thoughts at some point in their lives, and 34.7% have attempted suicide. For psychiatric outpatients, hormonal fluctuations contribute to about 25% of daily variations in suicidal thoughts.
"The luteal/perimenstrual phase of the menstrual cycle may represent the only recurrent, biological, predictable, idiographic variable capable of predicting phases of increased suicide risk."
- Hafsah A. Tauseef, Department of Psychiatry, University of Illinois Chicago
To address these risks, it's crucial to track your symptoms daily for at least two cycles and share this information with your healthcare provider. This tracking helps identify whether you're dealing with Premenstrual Exacerbation of an existing condition or PMDD - two issues that require different treatment plans. For women navigating hormonal changes alongside mental health challenges, platforms like Oana Health offer telehealth consultations with licensed professionals who specialize in these complex interactions, providing tailored care plans.
5. Worsening of Other Mental Health and Medical Conditions
Hormonal shifts don't just influence emotional well-being - they can also worsen existing mental health disorders and physical illnesses. For example, 60% of women with major depressive disorder or bipolar disorder report mood changes tied to their menstrual cycle.
Different mental health conditions react uniquely to these hormonal fluctuations. Women with bipolar disorder may experience depressive episodes, mania, or hypomania triggered by hormonal changes throughout their cycle. Research indicates that 64% to 68% of women with bipolar disorder report mood changes linked to their cycle. Similarly, women with panic disorder often notice an increase in the frequency and intensity of attacks during the premenstrual phase. For those with generalized anxiety disorder (GAD), the mid-luteal phase can bring heightened worry and social withdrawal, with about 45% of women with GAD reporting more severe social anxiety symptoms premenstrually.
Physical health conditions also follow this pattern. Migraines, for instance, are often tied to hormonal changes - about 50% of migraines in women are linked to their menstrual cycle, typically triggered by the sharp drop in estrogen before menstruation. A study on women undergoing IVF treatment found that 28.6% experienced migraines due to sudden estrogen withdrawal, with 82% of those migraines being debilitating. Other conditions, including asthma, epilepsy, rheumatoid arthritis, and irritable bowel syndrome, also tend to worsen during specific phases of the cycle.
"Hormonal fluctuations during the menstrual cycle present a unique period of vulnerability for the onset or exacerbation of psychiatric symptoms, impacting diagnosis, risk assessment, and treatment." - Jenny Lin et al., Frontiers in Psychiatry
The biological mechanisms behind these changes are complex. Fluctuations in estrogen and progesterone can alter GABA-A receptors in the brain, which play a role in reducing anxiety and stabilizing mood. These shifts can also cause structural changes in the hippocampus, a region critical for managing emotions. For women with pre-existing conditions, these changes can make otherwise manageable symptoms feel overwhelming. Talking to a healthcare provider about adjusting medication during the luteal phase or other targeted strategies can help improve symptom management.
Tracking Symptoms and Getting Support
If you’ve noticed changes in your mental health throughout the month, keeping track of your symptoms can make a big difference. Monitoring daily symptoms is much more reliable than trying to recall how you’ve felt after the fact. Experts recommend tracking for at least two consecutive cycles to identify patterns and differentiate between conditions like PMDD, where symptoms occur only before menstruation, and premenstrual exacerbation, where an existing condition worsens during the luteal phase.
Daily symptom tracking can uncover trends you might not otherwise notice. Tools like Daylio (used by over 20 million people with a 4.8/5 rating) and Moodfit simplify this process by letting you log your mood along with factors like sleep, exercise, and nutrition. For example, one study involving 352 women with depression found that 54.3% experienced significantly lower mood scores during the perimenstrual period - three days before to two days after menstruation - compared to the rest of their cycle.
"Ecological momentary assessment of mood over at least two consecutive cycles could be a useful tool for understanding menstrual cycle-related mood changes and diagnostic clarity may lead to alternative treatment and management options." - Glyn Lewis, Professor of Epidemiological Psychiatry, University College London
Once you’ve identified clear patterns, share this information with your healthcare provider to discuss potential treatment options. If your symptoms are severely affecting your daily life, work, or relationships - or if you’re experiencing intense low mood, crippling anxiety, or increased suicidal thoughts - reach out for professional support. For immediate assistance, call or text 988. For more tailored care, Oana Health offers telehealth consultations specializing in hormonal and mental health.
Bringing at least two months of symptom data to your appointments can help guide diagnosis and treatment decisions. Whether it’s adjusting medications during the luteal phase or considering hormonal therapies, having detailed records ensures you can get the support you need.
Conclusion
Your menstrual cycle impacts much more than just your physical health - it also plays a significant role in mental well-being. It can influence mood, anxiety levels, psychotic symptoms, suicide risk, and other mental health conditions. These five patterns highlight the deep connection between hormonal changes and mental health.
Recognizing these patterns is a crucial first step toward improving outcomes. Many women may not realize the link between their cycles and mental health until they start tracking their symptoms. Identifying a consistent pattern in your symptoms allows you to plan ahead, make adjustments to treatments, and reduce feelings of being overwhelmed. This understanding not only brings clarity but also paves the way for more focused and effective treatment.
"Diagnostic clarity may lead to alternative treatment and management options." - BMJ Mental Health
If you’ve noticed shifts in your mental health throughout the month, don’t dismiss them. Understanding these changes can lead to treatments tailored specifically to your needs.
Whether you’re managing a diagnosed mental health condition or experiencing symptoms for the first time, seeking professional support can be transformative. For care that addresses both hormonal and mental health concerns, Oana Health provides telehealth consultations to help you navigate these challenges. By tracking your cycle, you can take charge of your mental health and work toward a better quality of life.
FAQs
How can I track how my menstrual cycle affects my mental health?
To get a clear picture of how your menstrual cycle affects your mental health, start by using a trusted period-tracking app to log the different phases of your cycle. Pair this with daily mood tracking - rate your mood, energy levels, and anxiety every day. It’s also helpful to jot down notes about lifestyle factors like how much sleep you’re getting, your stress levels, or even your caffeine intake. This can help you distinguish between hormonal shifts and external influences.
At the end of each cycle, take some time to review your notes and look for patterns. For instance, you might notice heightened anxiety or a dip in mood during the luteal phase. If recurring mental health struggles stand out, reaching out to a licensed clinician through Oana Health could be a good next step. Their experts can provide personalized advice and treatment options. By tracking consistently, you’ll gain a deeper understanding of your body and be better equipped to take steps toward improving your mental well-being.
What are the best ways to manage PMDD symptoms?
Premenstrual dysphoric disorder (PMDD) can often be managed through a mix of lifestyle changes, therapy, and medication, tailored to the severity of symptoms and individual needs.
Lifestyle changes play a key role in easing PMDD symptoms. Regular exercise, eating a balanced diet that’s low in caffeine and alcohol, maintaining healthy sleep habits, and incorporating stress-reduction techniques like mindfulness or yoga can help alleviate mood swings and physical discomfort.
When lifestyle adjustments aren’t enough, therapy options like cognitive-behavioral therapy (CBT) or counseling can offer valuable tools to manage emotional challenges and improve overall well-being. For more severe symptoms, medications may be necessary. These might include selective serotonin reuptake inhibitors (SSRIs) or hormonal treatments, such as birth control pills containing drospirenone. Additionally, some individuals find relief with supplements like calcium, magnesium, or vitamin B6.
For personalized care, Oana Health’s telehealth services connect you with licensed professionals who specialize in female hormone health. They can assess your symptoms and provide tailored, prescription-based treatments delivered straight to your door, making care both accessible and convenient.
How can hormonal changes during the menstrual cycle increase the risk of suicidal thoughts?
Hormonal fluctuations, especially the rapid drop in estradiol and progesterone right before menstruation, can have a noticeable impact on mood and mental well-being. This shift can trigger heightened feelings of anxiety, irritability, or even hopelessness, potentially increasing the likelihood of experiencing suicidal thoughts or behaviors.
For some, these mood disturbances can be particularly intense, especially if they are dealing with conditions like premenstrual dysphoric disorder (PMDD). If you or someone you care about is navigating these challenges, seeking guidance from a healthcare provider can make a meaningful difference.
