How PCOS Affects Ovarian Cancer Risk
Women with PCOS (Polycystic Ovary Syndrome) may wonder if their condition increases the risk of ovarian cancer. The short answer? The overall risk remains low, but postmenopausal women with PCOS may face a higher likelihood of developing ovarian cancer. Here’s what you need to know:
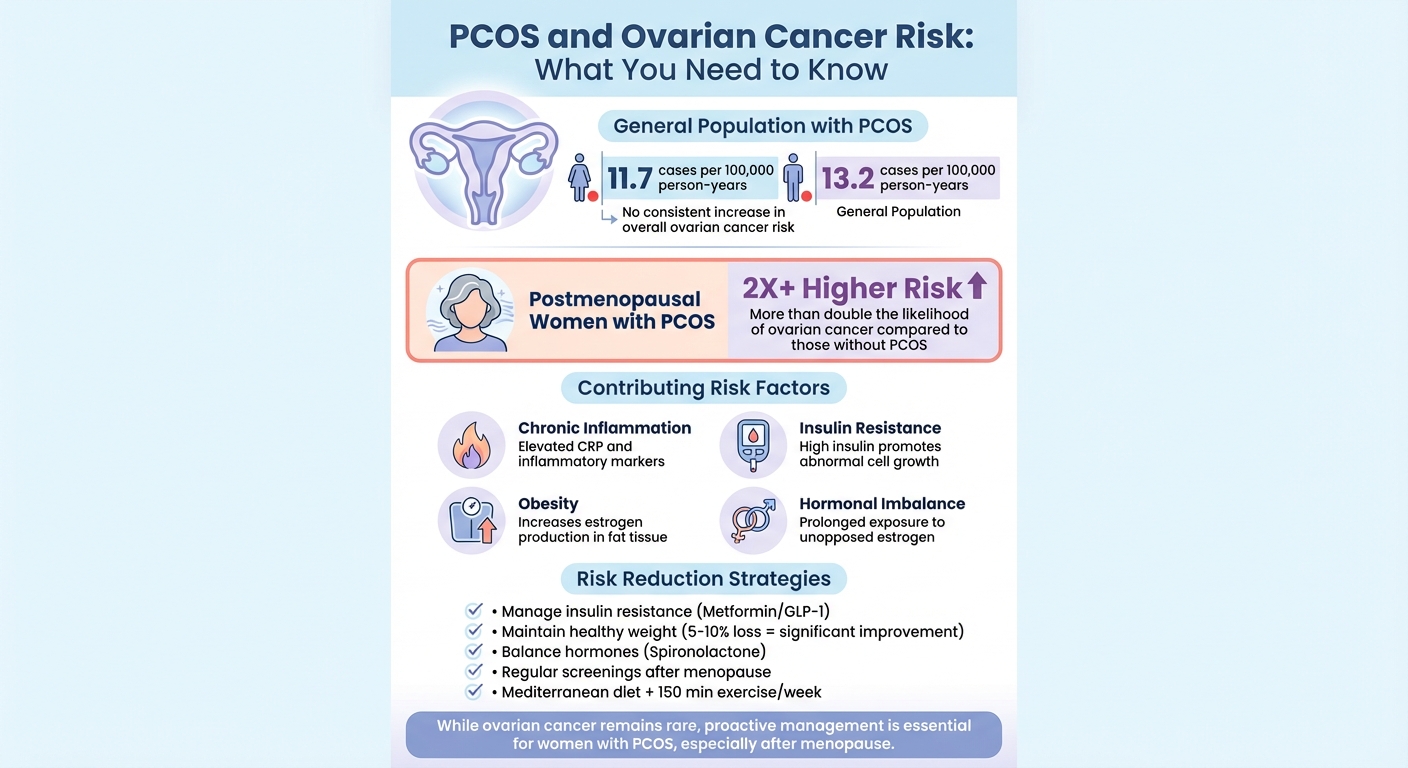
- General Risk: Studies show no consistent increase in ovarian cancer risk for women with PCOS overall.
- Postmenopausal Risk: Research indicates postmenopausal women with PCOS may have more than double the risk of ovarian cancer compared to those without PCOS.
- Other Cancer Risks: PCOS is more strongly linked to endometrial cancer due to prolonged hormonal imbalances.
- Key Factors: Chronic inflammation, insulin resistance, obesity, and hormonal imbalances may contribute to cancer risks in women with PCOS.
To lower your risk:
- Focus on managing insulin resistance with medications like Metformin or GLP-1 receptor agonists.
- Maintain a healthy weight through diet and exercise.
- Address hormonal imbalances with treatments like Spironolactone.
- Schedule regular screenings, especially after menopause.
Taking proactive steps with your healthcare provider can make a difference. While ovarian cancer is rare, being informed about the risks and prevention strategies is essential.
PCOS and Ovarian Cancer Risk: Key Statistics and Risk Factors
PCOS, Endometriosis, and Ovarian Cysts: Understanding Ovarian Cancer Risk
What Is PCOS? Hormonal Changes and Symptoms
Understanding the hormonal shifts in PCOS is essential to recognizing the long-term health risks tied to this condition.
Hormonal Imbalances in PCOS
PCOS revolves around three interconnected hormonal imbalances. First, there’s an increase in androgens, like testosterone, produced by the ovaries and sometimes the adrenal glands. This leads to noticeable symptoms like acne or unwanted hair growth. Second, insulin resistance plays a major role. When your body becomes less responsive to insulin, the pancreas compensates by producing more. These elevated insulin levels push the ovaries to produce even more androgens, creating a cycle that's hard to break. Finally, irregular or absent ovulation results in an overproduction of estrogen without enough progesterone to balance it. This imbalance, known as unopposed estrogen, affects the uterine lining and contributes to long-term health risks.
High insulin levels also lower sex hormone-binding globulin, which increases the amount of free estrogen and testosterone in the body. This amplifies the symptoms of PCOS. Additionally, many women experience low-grade inflammation, which researchers believe may exacerbate metabolic issues and increase cancer risks over time. These hormonal imbalances show up in various ways, described in the next section.
Common Symptoms of PCOS
One of the clearest indicators of PCOS is irregular menstrual cycles. This includes periods that are more than 35 days apart, fewer than eight periods a year, or cycles with very light or heavy bleeding. Many women also face weight gain, particularly around the abdomen, and struggle to lose weight despite their best efforts. Other signs of elevated androgens include unwanted facial or body hair (hirsutism), acne on the face, chest, or back, and thinning hair on the scalp, especially at the crown.
PCOS symptoms go beyond the visible. Women often experience difficulty conceiving, fatigue, mood swings such as anxiety or depression, and intense cravings for carbs. A skin condition called acanthosis nigricans, which appears as dark, velvety patches in body folds, can also signal insulin resistance. The symptoms vary widely - some women may be lean but have severe acne and irregular cycles, while others may experience significant weight gain but have relatively regular periods. Unfortunately, many women don’t receive a diagnosis until their 20s or 30s, often after struggling with infertility, even though the condition often begins in adolescence.
Identifying these symptoms early is critical. Prompt treatment can help regulate menstrual cycles, improve insulin sensitivity, and lower long-term risks, such as the two-to-three-fold increase in endometrial cancer risk caused by chronic unopposed estrogen. For those looking for convenient, tailored care, telehealth platforms like Oana Health (https://oanahealth.com) provide prescription-based treatments for challenges like insulin resistance, unwanted hair, acne, hair loss, and weight management. These services are offered by licensed medical professionals in the U.S. and include free home delivery.
PCOS and Ovarian Cancer Risk: What Research Shows
The connection between PCOS (polycystic ovary syndrome) and ovarian cancer has been the focus of numerous studies. Overall, the findings present a more reassuring outlook than some might anticipate.
Does PCOS Increase Ovarian Cancer Risk?
Current evidence does not consistently show an overall heightened risk of ovarian cancer for women with PCOS. A 2009 meta-analysis led by Chittenden and colleagues initially reported that women with PCOS faced about 2.5 times the risk of developing ovarian cancer (OR: 2.52, 95% CI: 1.08–5.89). However, more recent research has not consistently supported this finding.
For instance, a large Danish registry study, which included nearly 2 million women, found a slightly lower age-adjusted incidence of ovarian cancer in women with PCOS - 11.7 cases versus 13.2 cases per 100,000 person-years. After accounting for factors like obesity and education, the risk between women with and without PCOS appeared similar. Additionally, a 2023 systematic review on gynecologic cancers in women with PCOS found no compelling evidence of a general increase in ovarian cancer risk, contrasting with the well-documented higher risk for endometrial cancer.
Interestingly, genetic studies using Mendelian randomization suggest a possible inverse relationship between genetically predicted PCOS and invasive ovarian cancer, particularly for the endometrioid subtype. Despite these findings, the research remains inconsistent, leaving the overall picture inconclusive.
While ovarian cancer risk in women with PCOS seems relatively stable overall, age-specific variations are worth noting.
Postmenopausal Risk in Women with PCOS
Although the general risk of ovarian cancer doesn’t appear significantly elevated, studies suggest that postmenopausal women with PCOS may face higher risks. Notably, research highlights more than double the likelihood of developing serous borderline ovarian tumors in this group - tumors that have the potential to progress toward malignancy.
Dr. Clarissa Frandsen, a leading researcher, has called for updated clinical guidelines to address the increased ovarian cancer risk in postmenopausal women with PCOS. She emphasizes the importance of raising awareness, especially since effective screening tests for ovarian cancer remain unavailable. Similarly, Dr. Cristina Magli from the European Society of Human Reproduction and Embryology has urged closer monitoring of postmenopausal women with PCOS.
Given the hormonal changes associated with menopause and the potential risks, healthcare providers should encourage women with PCOS to report symptoms like bloating, pelvic pain, feeling full quickly, or urinary urgency. Timely discussions with a healthcare professional can help address these concerns effectively.
sbb-itb-6dba428
Factors Linking PCOS to Ovarian Cancer
The relationship between PCOS (Polycystic Ovary Syndrome) and ovarian cancer is not fully understood, but researchers have identified several biological processes that might increase cancer risk in certain women. These processes are particularly relevant for postmenopausal women with PCOS, who may face heightened risks.
Chronic Inflammation
Women with PCOS often deal with chronic low-grade inflammation, as indicated by elevated levels of markers like C-reactive protein (CRP) and inflammatory cytokines. This ongoing inflammation can damage cellular DNA and promote the formation of new blood vessels, creating an environment that supports tumor growth. To combat inflammation, adopting an anti-inflammatory diet and incorporating 1,000 mg of omega-3 fatty acids (EPA+DHA) daily may be helpful [5].
Insulin Resistance and Obesity
Insulin resistance is a common feature of PCOS and leads to higher levels of circulating insulin. Elevated insulin can encourage abnormal cell growth and interfere with programmed cell death (apoptosis). Additionally, many women with PCOS struggle with overweight or obesity, which increases estrogen production in fat tissue. This excess estrogen worsens insulin resistance and inflammation, further altering the ovarian environment. These effects are particularly pronounced after menopause, when progesterone levels naturally decline. Managing weight through a healthy diet, regular exercise, and, when necessary, medications like metformin can improve metabolic health and reduce these risks.
Prolonged Hormonal Exposure
PCOS often results in irregular or absent ovulation, leading to fewer progesterone surges and prolonged exposure to estrogens and androgens. While this "unopposed estrogen" pattern is strongly linked to endometrial cancer, some experts believe long-term hormonal imbalances may also impact ovarian and fallopian tube cells. The repeated formation of ovarian cysts and incomplete follicle rupture can cause cycles of tissue damage and repair, which have historically been associated with epithelial ovarian cancer.
Interestingly, fewer lifetime ovulations are generally tied to a lower ovarian cancer risk. However, this potential benefit in women with PCOS may be offset by factors like obesity, elevated androgen levels, and metabolic dysfunction. On a positive note, hormonal contraceptives, which regulate menstrual cycles, are known to lower ovarian cancer risk in the general population. These insights highlight the importance of tailored strategies to manage hormonal and metabolic health, particularly for women with PCOS, to help reduce their ovarian cancer risk.
How to Reduce Ovarian Cancer Risk with PCOS
Taking control of factors like insulin resistance, hormonal imbalances, and weight can significantly lower the risk of ovarian cancer, especially after menopause.
Managing Insulin Resistance
Improving how your body handles insulin is a major step. Medications like Metformin can help by reducing glucose production in the liver and enhancing insulin sensitivity. This lowers chronic high insulin levels, which are linked to abnormal cell growth.
For those who experience side effects from oral Metformin, topical alternatives provide a gentler option. As one user, Carrie S., shared:
I'm so glad I discovered Oana's metformin lotion! I used to struggle a lot with the side effects for oral metformin and this is a great alternative for me. I get the benefits without the upset stomach and nausea.
Another effective option is GLP-1 receptor agonists, such as Semaglutide. These medications not only improve insulin sensitivity but also support weight loss, addressing two major risk factors at once. Companies like Oana Health offer tailored treatments, including oral Metformin ER (starting at $22/month), topical Metformin (starting at $89/month), and dual agonist GLP-1 tablets ($199/month), all delivered with free shipping.
Once insulin resistance is under control, focusing on hormonal balance and weight can further reduce your risk.
Addressing Hormonal Imbalances and Weight
High androgen levels can disrupt hormonal balance and increase cancer risk. Medications like Spironolactone block androgen receptors, helping to treat symptoms like unwanted facial hair while promoting a healthier hormonal environment. Since elevated androgens are linked to higher ovarian cancer risk, managing these levels is crucial.
Weight management is another key factor. Losing just 5-10% of your body weight can dramatically improve insulin resistance and reduce inflammation - both of which play a role in cancer risk. Obesity can worsen the metabolic challenges associated with PCOS. Combining medications like Spironolactone with a calorie-controlled diet and regular exercise yields the best results.
Lifestyle Changes and Routine Screenings
Medications are helpful, but lifestyle changes and routine screenings are equally important for reducing ovarian cancer risk.
Adopt a Mediterranean-style diet rich in vegetables, fatty fish, and whole foods while limiting refined carbs. Aim for at least 150 minutes of moderate exercise each week, like brisk walking, to improve insulin sensitivity and reduce inflammation. Adding about 1,000 mg of omega-3 fatty acids (EPA+DHA) daily can also help lower inflammation within 8-12 weeks [5].
Regular screenings are vital, particularly for postmenopausal women with PCOS, who face more than double the risk of ovarian cancer compared to those without PCOS. Annual transvaginal ultrasounds, CA-125 blood tests, and pelvic exams are recommended for early detection. Work with your healthcare provider to create a screening plan tailored to your specific risks and needs.
Conclusion
Although PCOS does not significantly raise the overall risk of ovarian cancer, research shows that postmenopausal women with PCOS face more than double the risk compared to those without the condition. This highlights the importance of tailored management strategies to address these specific risks.
Taking steps to manage insulin resistance, maintain a healthy weight, and balance hormones can help reduce these risks. Even a small weight loss - just 5–10% of your body weight - can lead to meaningful improvements in metabolic health by addressing factors like chronic inflammation and prolonged hormonal exposure. Pairing regular physical activity with a Mediterranean-style diet can further support these efforts and promote overall well-being.
Routine check-ins with your healthcare provider are equally essential, especially after menopause. While there isn’t a standard screening test for ovarian cancer in women with average risk, discussing any noticeable changes or concerns during regular appointments ensures that potential problems are caught early.
For those seeking additional support, Oana Health provides personalized telehealth services grounded in science. Their licensed medical professionals offer treatments like oral Metformin ER (starting at $22/month), topical Metformin (starting at $89/month), and dual agonist GLP-1 tablets (starting at $199/month), all delivered to your doorstep with free shipping. Taking proactive steps now can make a lasting difference in safeguarding your health.
FAQs
Does having PCOS increase my risk of ovarian cancer after menopause?
Having PCOS might slightly raise the likelihood of ovarian cancer, but it doesn't guarantee you'll develop it after menopause. Other elements, like your family history, lifestyle choices, and overall health, also influence your risk.
You can take steps to lower this risk by focusing on things like keeping a healthy weight, managing hormone levels, and addressing insulin resistance. If you're worried, it's a good idea to talk with a healthcare provider. They can help you understand your personal risk factors and explore ways to stay proactive about your health.
What can women with PCOS do to lower their risk of ovarian cancer?
Women with PCOS can take practical steps to reduce their risk of ovarian cancer. One key approach is maintaining a healthy weight by focusing on a balanced diet paired with regular physical activity. This can help regulate hormones and minimize inflammation, both of which play a role in overall health.
Addressing insulin resistance under medical supervision is another important step. Additionally, steering clear of smoking and keeping alcohol consumption in check can make a meaningful difference.
Regular check-ups with your healthcare provider are essential for monitoring your health and catching potential issues early. By taking these steps, you not only support hormonal balance but also enhance your overall well-being for the long term.
What ovarian cancer symptoms should women with PCOS be aware of?
Women with PCOS should pay close attention to signs that might indicate ovarian cancer. Symptoms such as persistent pelvic or abdominal pain, bloating, frequent urination, and feeling full quickly after eating are worth noting. While these can overlap with PCOS symptoms, it's crucial to seek medical advice if they appear suddenly, become severe, or persist over time.
Routine check-ups and honest conversations with your doctor are essential for catching potential issues early. If you’re navigating PCOS and have concerns about your risk, working with licensed professionals, like those at Oana Health, can provide tailored guidance to help safeguard your health.
