PCOS Medications: Rare Side Effects Explained
PCOS affects up to 13% of women globally, and medications like Metformin and GLP-1 receptor agonists (e.g., Semaglutide, Tirzepatide) are key treatments. These drugs help manage insulin resistance, weight, and hormonal imbalances. However, rare side effects exist and require attention. Here’s what you need to know:
- Metformin: Rare risks include lactic acidosis (linked to kidney/liver issues), vitamin B12 deficiency (6%-30% of long-term users), and low blood sugar (when combined with other diabetes drugs). Symptoms like rapid breathing, muscle pain, or extreme fatigue require immediate care.
- GLP-1 Medications: Rare risks include thyroid tumors (observed in animal studies), gallbladder issues (1%-1.6% experience gallstones), and pancreatitis. Watch for symptoms like neck lumps, severe abdominal pain, or jaundice.
- Pregnancy Considerations: GLP-1 medications must be stopped 2 months before conception, while Metformin may aid ovulation.
Key takeaway: Recognizing rare side effects early ensures safe and effective PCOS management. Always consult your doctor about your medical history and future plans before starting treatment.
Rare Side Effects of GLP-1 Medications (Ozempic and Semaglutide)

GLP-1 medications, like semaglutide, are commonly used to address weight loss and insulin resistance in individuals with PCOS. However, understanding the rarer risks associated with these treatments is crucial for making informed decisions. Below, we break down three uncommon but important risks to be aware of.
Thyroid Cancer Risk
Semaglutide comes with an FDA boxed warning regarding the potential risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC). Research on animals has shown that the medication can cause dose-dependent thyroid tumors in mice and rats. However, as Dr. Disha Narang, an endocrinologist, points out:
"The risk of medullary thyroid cancer was seen in phase 1 trials in animal studies. It's never actually been seen in a human."
Because of this potential risk, semaglutide is not recommended for those with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). The FDA advises that routine blood tests or thyroid ultrasounds may not be particularly helpful for early detection. Instead, watch for physical signs like a lump in the neck, persistent hoarseness, difficulty swallowing, or shortness of breath. If any of these symptoms arise, contact your healthcare provider immediately.
Gallbladder Problems
GLP-1 medications can sometimes lead to gallbladder issues through two main pathways. First, they may slow the gallbladder’s emptying process, which can result in gallstones. Additionally, rapid weight loss itself is a known risk factor for gallstone formation.
Data suggests that about 1 in 100 people taking Ozempic develop gallstones, while roughly 1 in 1,000 experience more severe complications like gallbladder infections (cholecystitis). Clinical trials have reported gallstones in 1.5% of patients on a 0.5 mg dose and 0.4% on a 1 mg dose, compared to 0% in the placebo group. Similar outcomes were observed with Wegovy, where 1.6% of users developed gallstones, compared to 0.7% in the placebo group.
Be mindful of "gallbladder attacks", which often occur after eating fatty meals and can last from minutes to hours. Symptoms to watch for include upper abdominal pain, fever, jaundice (yellowing of the skin or eyes), and pale, clay-colored stools. If you notice any of these signs, consult your provider, who may recommend an ultrasound for evaluation.
Pancreatitis and Severe Dehydration
Though rare, GLP-1 medications can cause acute pancreatitis. The risk may increase with rapid weight loss - more than 3.3 pounds per week - as this can lead to gallstones that might trigger pancreatitis. Symptoms to look out for include severe abdominal pain that radiates to the back and persistent vomiting. If these occur, stop taking the medication immediately and seek emergency medical help.
Gastrointestinal side effects like nausea, diarrhea, and vomiting are more common, occurring in about 15% to 30%, 10% to 15%, and 5% to 10% of patients, respectively, during clinical trials. These symptoms can lead to dehydration, which may cause unusual fatigue, reduced urination, rapid weight gain, or swelling in the legs and ankles. To stay hydrated, aim to drink 91–125 fluid ounces daily if experiencing these side effects. If symptoms persist, contact your healthcare provider promptly.
Rare Side Effects of Metformin
Metformin is a widely used medication for managing insulin resistance in conditions like PCOS. While it’s generally well-tolerated, there are a few rare but serious side effects that patients should be aware of.
Lactic Acidosis
One of the most concerning complications is metformin-associated lactic acidosis (MALA), a rare but life-threatening condition where lactic acid builds up in the blood faster than the body can remove it. This happens because metformin can interfere with mitochondrial function, reducing the liver’s ability to clear lactate.
Although extremely rare - occurring in about 0.03 cases per 1,000 patient-years - MALA can be fatal in 30% to 50% of cases when it does occur. Clinical trials involving over 20,000 patient-years reported no cases of MALA, but it remains a critical condition to recognize and manage.
"Lactic acidosis is a medical emergency that must be treated in a hospital setting."
– U.S. Food and Drug Administration (FDA)
MALA is diagnosed when blood pH drops below 7.35 and lactate levels exceed 5.0 mmol/L. It’s often linked to toxic levels of metformin in the blood, typically due to underlying kidney or liver issues. To address this, the FDA updated its guidelines in 2016, allowing metformin use in patients with mild to moderate kidney impairment but advising against its use in those with severe kidney disease (eGFR below 30 mL/min/1.73 m²). Regular monitoring of kidney function, including annual eGFR tests, is recommended for anyone taking metformin.
"The risk of lactic acidosis increases with the degree of renal dysfunction and the patient's age."
– U.S. Food and Drug Administration (FDA)
Symptoms to watch for include rapid breathing, extreme fatigue, irregular heartbeat, cold sensations in the extremities, muscle pain, and abdominal discomfort. To minimize risk:
- Limit alcohol consumption, as it can amplify metformin’s effects on lactate metabolism.
- Stop metformin temporarily before surgeries or imaging procedures involving contrast dyes, which may affect kidney function.
- Discontinue metformin and consult your doctor immediately in cases of severe dehydration caused by fever, vomiting, or diarrhea.
Vitamin B12 Deficiency
Long-term use of metformin can interfere with vitamin B12 absorption in the stomach and small intestine, leading to a deficiency in about 6% to 30% of users - especially those on higher doses or taking it for four years or longer.
A vitamin B12 deficiency can have serious consequences. As Diana Isaacs, PharmD, from Cleveland Clinic explains:
"If you don't have enough vitamin B12, that can lead to neuropathy, or the numbness and tingling of your hands and feet and can even cause memory problems."
– Diana Isaacs, PharmD, Cleveland Clinic
This deficiency can also result in pernicious anemia, marked by a lack of healthy red blood cells. For individuals with PCOS, maintaining vitamin B12 levels above 450 pg/mL is considered ideal. Symptoms of deficiency include extreme fatigue, muscle weakness, shortness of breath, pale or yellow skin, heart palpitations, memory issues, depression, confusion, numbness or tingling, mouth ulcers, and digestive discomfort.
If you’ve been on metformin for four or more years, it’s important to have your vitamin B12 levels checked annually. Beyond standard serum tests, measuring serum homocysteine and urinary methylmalonic acid (MMA) levels offers a more thorough evaluation. If a deficiency is detected, your doctor may recommend vitamin B12 injections, which are often more effective than oral supplements due to metformin’s impact on stomach absorption.
Severe Low Blood Sugar
While metformin alone rarely causes hypoglycemia, the risk increases when it’s combined with insulin or sulfonylureas. Diana Isaacs, PharmD, clarifies:
"Metformin doesn't usually cause hypoglycemia on its own unless it's taken in combination with insulin or other diabetes medications like sulfonylureas..."
– Diana Isaacs, PharmD, Cleveland Clinic
Other factors, like skipping meals, insufficient carbohydrate intake, or excessive exercise, can also trigger low blood sugar. Alcohol consumption - especially on an empty stomach or in excess - further heightens the risk. Additionally, conditions like kidney or liver disease and hypothyroidism can make hypoglycemia more likely.
Symptoms of low blood sugar include shaking, sweating, dizziness, confusion, extreme hunger, and a rapid heartbeat. To help prevent these episodes, take metformin with food and keep fast-acting carbohydrates like sugar cubes, fruit juice, or candies nearby for quick relief if needed.
Comparing Rare Side Effects Across PCOS Medications
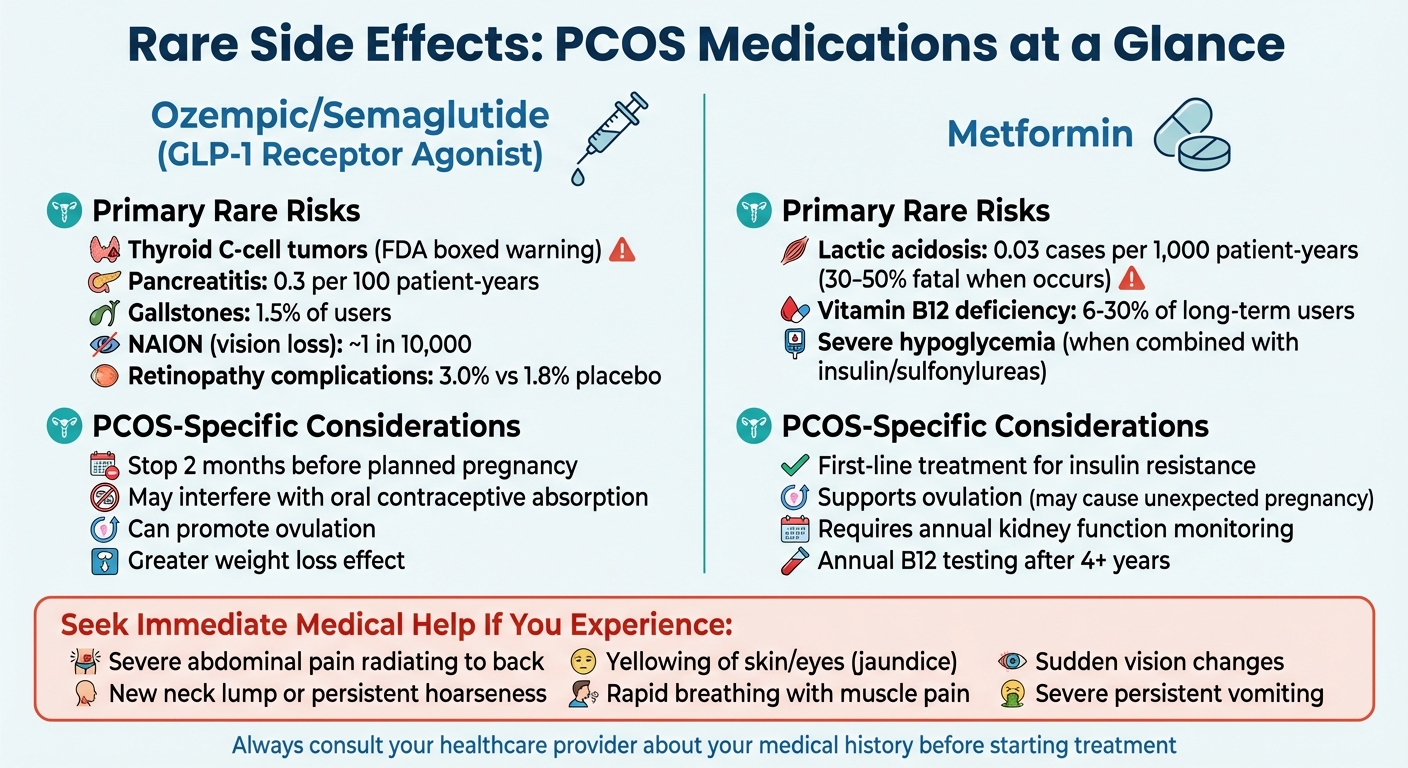
PCOS Medications Rare Side Effects Comparison Chart
Side-by-Side Comparison Table
For women managing PCOS, understanding rare side effects is an important part of balancing the benefits and risks of treatment. Comparing these risks can help guide decisions about which medication might be the best fit. While GLP-1 receptor agonists and Metformin are generally considered safe, each comes with specific rare side effects worth noting.
| Medication | Primary Rare Risks | Frequency / Risk Level | PCOS-Specific Considerations |
|---|---|---|---|
| Ozempic / Semaglutide | Thyroid C-cell tumors (boxed warning), Pancreatitis, Gallbladder disease, NAION (vision loss), Ileus | Pancreatitis: 0.3 per 100 patient-years; Gallstones: 1.5%; NAION: ~1 in 10,000; Retinopathy complications: 3.0% vs. 1.8% placebo | Discontinue at least 2 months before planned pregnancy; may interfere with oral contraceptive absorption due to delayed stomach emptying; can promote ovulation |
| Metformin | Lactic acidosis, Vitamin B12 deficiency, Severe hypoglycemia (when used with insulin or sulfonylureas) | Lactic acidosis: very rare; Vitamin B12 deficiency: may occur with long-term use | First-line treatment for insulin resistance; supports ovulation, which may lead to unexpected pregnancy |
This comparison emphasizes the differences that can influence treatment choices. For example, GLP-1 receptor agonists are associated with greater weight loss and improved insulin sensitivity but carry a thyroid cancer warning. According to the prescribing information:
"In rodents, semaglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures. It is unknown whether Ozempic® causes thyroid C-cell tumors... in humans."
– Novo Nordisk
On the other hand, Metformin's rare risks include lactic acidosis and vitamin B12 deficiency. The Mayo Clinic describes lactic acidosis as:
"The symptoms of lactic acidosis are severe and quick to appear, and usually occur when other health problems not related to the medicine are present and are very severe, such as a heart attack or kidney failure."
– Mayo Clinic
What to Consider When Choosing a Medication
When deciding on a treatment, your personal health history, current conditions, and future plans play a crucial role. PCOS comes with its own metabolic challenges, so tailoring the choice to your unique situation is key.
Your medical history is critical. If you or a family member has a history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), GLP-1 medications are not recommended. Additionally, for those with severe kidney or liver disease or congestive heart failure, the risk of lactic acidosis with Metformin is higher.
Pregnancy plans matter. GLP-1 medications need to be stopped at least two months before trying to conceive due to limited safety data. In contrast, Metformin may help restore ovulation, which could lead to an unexpected pregnancy if reliable contraception isn’t used. Also, because GLP-1 medications delay stomach emptying, they can interfere with oral contraceptive absorption.
Pre-existing conditions can influence safety. If you have diabetic retinopathy, for example, GLP-1 medications may not be the best choice. The European Medicines Agency (EMA) advises:
"If patients experience a sudden loss of vision or rapidly worsening eyesight during treatment with semaglutide, they should contact their doctor without delay. If NAION is confirmed, treatment with semaglutide should be stopped."
– European Medicines Agency (EMA)
Lifestyle factors also play a role. Around 7% of patients in clinical trials discontinued semaglutide due to severe gastrointestinal side effects. For those with a history of eating disorders, the appetite suppression caused by GLP-1 medications could trigger disordered eating patterns. Metformin, on the other hand, usually causes mild digestive issues that tend to improve over time.
Insulin resistance severity guides treatment. Metformin has been the go-to treatment for PCOS-related insulin resistance for years. However, newer research suggests that GLP-1 receptor agonists may be more effective in reducing BMI and waist circumference in women with PCOS. Ultimately, your doctor will weigh factors like your level of insulin resistance, weight loss goals, and overall metabolic health when recommending the best medication for you.
sbb-itb-6dba428
When to Get Medical Help and How Oana Health Can Support You
Warning Signs That Need Immediate Attention
Understanding when to seek medical help while taking PCOS medications can be crucial. Some symptoms demand immediate action, while others require prompt communication with your healthcare provider.
Stop your medication and seek emergency care immediately if you experience severe abdominal pain that doesn’t go away, especially if it spreads to your back. This could signal pancreatitis, which requires urgent medical attention. Swelling of the face, lips, tongue, or throat, as well as difficulty breathing or swallowing, could indicate a severe allergic reaction. In such cases, discontinue the medication and contact your healthcare provider right away. Additionally, symptoms like a new lump or swelling in your neck, hoarseness, or trouble swallowing could point to thyroid tumors and should be addressed promptly.
Be alert to gallbladder issues, which might appear as intense pain in the upper stomach, fever, jaundice (yellowing of the skin or eyes), or pale, clay-colored stools. Persistent vomiting or diarrhea can lead to dehydration and kidney problems, which may show up as reduced urination, back pain, or swelling in the legs or ankles. Sudden vision changes also require immediate attention from your healthcare provider. Additionally, you can report any adverse drug reactions directly to the FDA by calling 1-800-FDA-1088.
Recognizing these warning signs early can help ensure your treatment plan is adjusted quickly and appropriately.
How Oana Health Supports PCOS Treatment
Managing PCOS medications effectively requires ongoing support, especially when dealing with potential side effects. This is where telehealth platforms like Oana Health come in, offering continuous monitoring and personalized care. Oana Health connects patients with licensed physicians through independently owned medical practices, ensuring that treatment plans are tailored to your needs and adjusted for safety as necessary.
Through Oana Health, you can access PCOS-related medications such as Ozempic, compounded semaglutide, and Metformin ER. These prescriptions are delivered directly to your door with free shipping. The platform also provides educational tools to help you understand potential risks, like vitamin B12 deficiency or lactic acidosis linked to Metformin use. For common side effects like gastrointestinal discomfort, your provider can adjust dosages to help minimize these issues, which often improve over time.
Interestingly, research shows that women may be twice as likely as men to experience side effects from GLP-1 medications. Dr. Beverly Tchang, Obesity Medicine Advisor for Ro, sheds light on this:
"The sensitivity to GI side effects of GLP1s may be more pronounced in women because they already have a longer gut transit time compared to men."
With telehealth services, you can quickly reach your healthcare provider if any symptoms arise, avoiding the need for in-person visits. This immediate access to professional guidance is especially helpful for managing rare or unexpected side effects that require swift attention.
Conclusion
Being aware of the rare side effects of PCOS medications equips you to make informed decisions about your treatment and safeguard your health. Serious complications like pancreatitis, thyroid tumors, or lactic acidosis are uncommon, but recognizing the warning signs early can make a critical difference. Acting promptly can help prevent life-threatening issues and ensure your treatment remains both effective and safe for your unique needs.
The benefits of PCOS medications often outweigh the risks, especially when a small weight loss of just 5%–10% can lead to significant symptom improvement. However, this requires personalized care tailored to your individual risk factors, health history, and family background - not a one-size-fits-all approach.
Before starting any treatment, it's essential to discuss your medical history with your healthcare provider. For example, if you have a family history of medullary thyroid carcinoma or MEN 2, GLP-1 medications might not be suitable. If you're planning a pregnancy, you’ll need to stop semaglutide at least two months beforehand. Additionally, women taking anti-androgens like spironolactone must use reliable contraception to avoid potential harm to a developing fetus. These factors highlight the importance of ongoing professional guidance.
Telehealth platforms, like Oana Health, offer continuous support to help you manage PCOS effectively. Their licensed physicians provide personalized treatment plans, adjust dosages when necessary, and monitor for any concerning symptoms. With options like Metformin ER starting at $22 per month and oral semaglutide at $199 per month - delivered directly to your door with free shipping - you can enjoy both convenience and expert oversight.
Staying in regular contact with your healthcare team is key. Keep track of your symptoms and seek help immediately if anything feels off. With proper monitoring and support, you can manage PCOS while minimizing risks and ensuring your treatment plan works for you.
FAQs
What symptoms might indicate a thyroid cancer risk with GLP-1 medications?
While it's uncommon, GLP-1 medications have been associated with thyroid C-cell tumors in certain cases. Keep an eye out for warning signs like a new lump in your neck, trouble swallowing, ongoing hoarseness, or a persistent cough. If you experience any of these symptoms, reach out to your healthcare provider without delay to ensure everything is checked thoroughly.
What can I do to reduce the risk of lactic acidosis while taking Metformin?
To help reduce the risk of lactic acidosis while taking Metformin, make sure to take the medication with meals to minimize stomach discomfort. Begin with the lowest dose prescribed and gradually increase it as instructed by your healthcare provider. Staying hydrated is key - drink plenty of water, and try to limit alcohol intake, as dehydration and excessive alcohol use can heighten the risk.
Regular monitoring of kidney function is crucial, particularly if you’re 65 or older or have a history of kidney, heart, or vascular issues. Watch for warning signs like unusual fatigue, muscle pain, trouble breathing, or a slow heartbeat. If you notice any of these symptoms, reach out to your doctor immediately, as they could signal lactic acidosis.
What should I know about taking PCOS medications if I’m planning to get pregnant?
If you’re planning to get pregnant, it’s essential to stop using GLP-1 receptor agonists (like semaglutide or tirzepatide) before trying to conceive. These medications aren’t recommended for women aiming to get pregnant and could also make oral contraceptives less effective. Have a conversation with your healthcare provider about switching to a pregnancy-safe alternative, such as metformin.
At the same time, begin taking prenatal vitamins with folic acid to support a healthy pregnancy. Work closely with your healthcare provider to keep an eye on your blood sugar and hormone levels during this pre-conception phase. These proactive steps can help you manage your PCOS symptoms and prepare your body for a healthy pregnancy.
