How Probiotics Help Insulin Resistance
Probiotics can improve insulin resistance by supporting gut health. For women with PCOS, insulin resistance affects up to 75%, leading to symptoms like acne, irregular cycles, and fertility issues. Gut imbalances (dysbiosis) worsen this condition, but probiotics can help by:
- Restoring gut bacteria balance: Probiotics increase beneficial strains like Lactobacillus and Bifidobacterium, reducing harmful bacteria and improving insulin signaling.
- Reducing inflammation: They lower markers like TNF-α and C-reactive protein (CRP), which disrupt insulin function.
- Improving glucose processing: Probiotics activate pathways like AMPK, enhancing glucose uptake in muscles and liver.
Studies show probiotics lower fasting insulin, blood sugar, and HOMA-IR levels within 8–12 weeks. Synbiotics (probiotics + prebiotics) provide even better results by boosting gut health further. Combining probiotics with treatments like Metformin can offer a more effective approach to managing PCOS symptoms. For personalized plans, services like Oana Health provide tailored options, including Metformin and synbiotic blends.
Research on PCOS and Probiotics
How Probiotics Improve Insulin Sensitivity
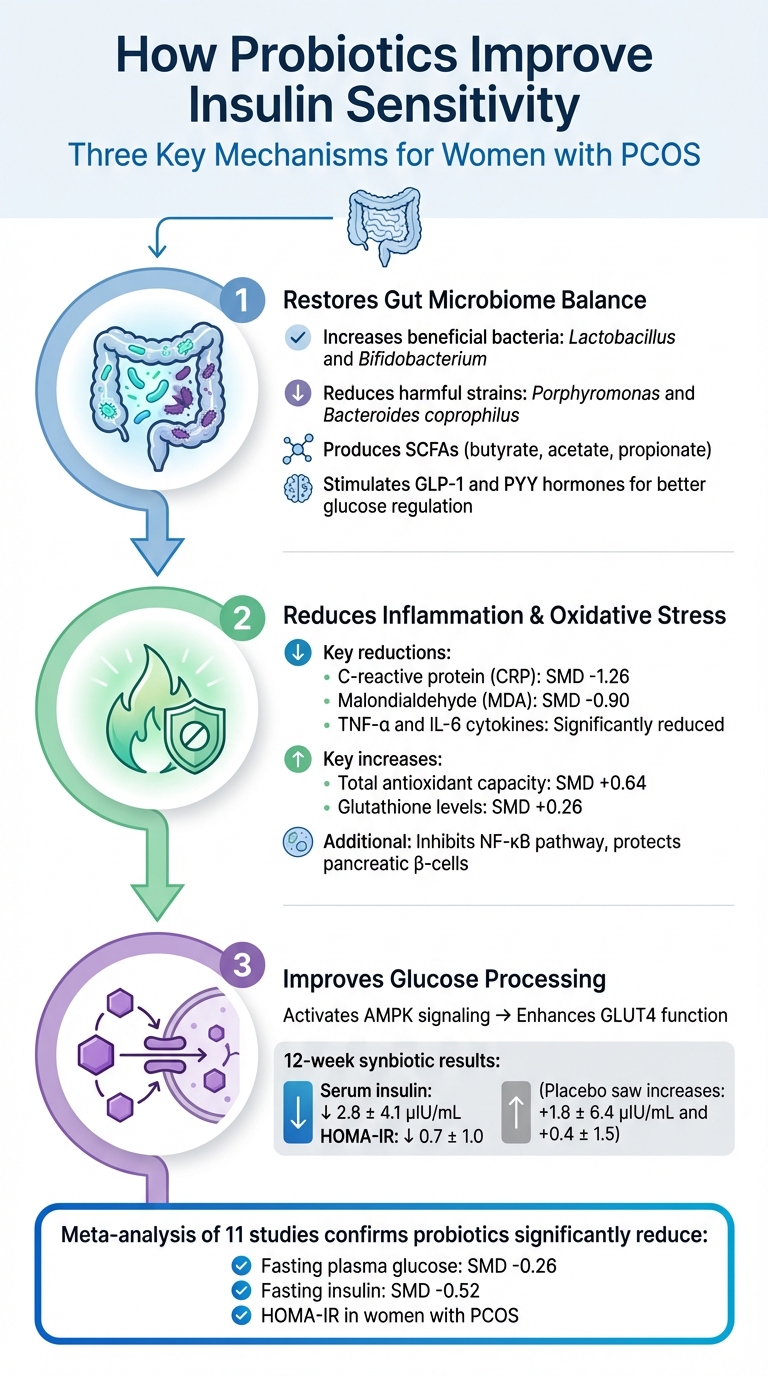
How Probiotics Improve Insulin Resistance in PCOS: 3 Key Mechanisms
Probiotics play a significant role in improving insulin sensitivity by addressing underlying metabolic issues. They work through various mechanisms that help combat insulin resistance, particularly in women with PCOS.
Balancing Gut Bacteria
Probiotics help restore balance in the gut microbiome by increasing beneficial bacteria like Lactobacillus and Bifidobacterium, while reducing harmful microbes. This enhanced balance strengthens the intestinal barrier and improves insulin signaling. Women with PCOS often have an imbalance in their gut bacteria, with higher levels of harmful strains like Porphyromonas and Bacteroides coprophilus, and lower levels of bacteria that produce short-chain fatty acids (SCFAs).
The beneficial bacteria ferment dietary fiber into SCFAs such as butyrate, acetate, and propionate. These SCFAs stimulate the release of hormones like glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), which improve glucose regulation, enhance insulin secretion, and even help suppress appetite.
Lowering Inflammation and Oxidative Stress
Chronic inflammation is a key driver of insulin resistance, and probiotics help counteract this by reducing levels of pro-inflammatory cytokines like TNF-α and IL-6, as well as markers of oxidative damage such as C-reactive protein (CRP) and malondialdehyde (MDA). Studies have shown that probiotic supplementation significantly lowers CRP (SMD -1.26) and MDA (SMD -0.90) in women with PCOS.
At the same time, probiotics enhance the body’s antioxidant defenses by increasing total antioxidant capacity (SMD 0.64) and boosting glutathione levels (SMD 0.26). They also inhibit the NF-κB pathway, which is a major contributor to systemic inflammation. These combined effects protect pancreatic β-cells from oxidative damage, ensuring better insulin production.
Enhancing Insulin Utilization
Probiotics also improve how the body processes glucose by activating 5'-AMP-activated protein kinase (AMPK) signaling. This activation enhances the function of glucose transporter 4 (GLUT4) in the muscles and liver, which helps regulate blood sugar levels.
In a 12-week clinical trial, women with PCOS who took synbiotics experienced a reduction in serum insulin by 2.8 ± 4.1 μIU/mL and a drop in HOMA-IR by 0.7 ± 1.0. Meanwhile, the placebo group saw increases of 1.8 ± 6.4 μIU/mL and 0.4 ± 1.5, respectively. A meta-analysis of 11 studies further confirmed that probiotics significantly reduced fasting plasma glucose (SMD -0.26), fasting insulin (SMD -0.52), and HOMA-IR in women with PCOS.
"Probiotics and/or prebiotics could be a promising approach to improve insulin sensitivity by favourably modifying the composition of the gut microbial community, reducing intestinal endotoxin concentrations and decreasing energy harvest." - Nutrition Research Reviews
Through these mechanisms, probiotics offer a targeted way to reshape metabolic responses and improve insulin sensitivity in women with PCOS.
Research on Probiotics and Insulin Resistance
Effects on HOMA-IR and Fasting Insulin Levels
Studies show that probiotics can play a significant role in improving markers of insulin resistance. Meta-analyses highlight that probiotics help lower HOMA-IR (SMD –0.53), fasting insulin (SMD –0.52; reductions ranging from 1.29 to 2.27 µIU/mL), and fasting blood glucose (SMD –0.26, about 5.6 mg/dL). A systematic review of 11 randomized clinical trials conducted between 2017 and 2022 supported these findings, particularly in overweight or obese women with PCOS. These results emphasize the need to determine which probiotic strains are most effective.
Which Probiotic Strains Work Best
Certain strains from the Lactobacillus and Bifidobacterium families consistently show benefits in improving insulin sensitivity. Among Lactobacillus, the most researched strains include L. acidophilus, L. rhamnosus, L. reuteri, L. plantarum, L. casei, and L. fermentum. For Bifidobacterium, strains like B. bifidum, B. longum, B. breve, B. animalis, and B. lactis have demonstrated similar benefits.
Interestingly, probiotics with multiple strains tend to outperform single-strain options. A 2022 randomized, double-blind study published in the European Journal of Nutrition tested a seven-strain probiotic blend in 104 women with PCOS aged 18–40. The formula included L. acidophilus UBLA-34, L. rhamnosus UBLR-58, and L. reuteri UBLRu-87 (2 billion CFU each), along with L. plantarum UBLP-40, L. casei UBLC-42, L. fermentum UBLF-31, and B. bifidum UBBB-55 (1 billion CFU each). After six months, participants saw significant improvements in menstrual cycle regularity (p = 0.023) and testosterone levels (p = 0.043). While strain selection is key, the duration of supplementation also matters.
How Long to Take Probiotics for Results
Daily and consistent use is critical to achieving results. Clinical trials suggest that taking probiotics for 8 to 12 weeks is usually required to see noticeable improvements in insulin sensitivity and related blood markers. A meta-analysis found that interventions lasting more than 8 weeks consistently reduced fasting blood glucose, whereas shorter durations often led to mixed outcomes. Research on Type 2 Diabetes further supports this, showing that extended supplementation - 12 weeks or longer - yields better reductions in HbA1c and HOMA-IR levels.
sbb-itb-6dba428
Probiotics vs. Synbiotics for Insulin Resistance
What Makes Probiotics and Synbiotics Different
Probiotics are live microorganisms, primarily from the Lactobacillus and Bifidobacterium groups, that contribute to maintaining a healthy gut environment. Synbiotics, on the other hand, take it a step further by combining probiotics with prebiotics - fiber sources like inulin or fructo-oligosaccharides. Prebiotics act as fuel for probiotics, helping them survive and thrive in the gut. Together, this duo strengthens the gut barrier by reducing intestinal permeability and boosting the production of short-chain fatty acids (SCFAs), which play a role in improving insulin signaling and glucose regulation. The inclusion of prebiotics in synbiotics amplifies these effects, making them a more effective tool for metabolic support.
Benefits of Synbiotics for PCOS
Synbiotics stand out for their enhanced metabolic benefits, particularly for women managing PCOS. Research indicates that synbiotics outperform probiotics alone when it comes to improving insulin resistance in PCOS. A 2024 systematic review highlighted that synbiotics were more effective in improving markers like HOMA-IR, fasting glucose levels, and hormonal balance. In fact, recent clinical trials on PCOS interventions show that 70% of them involved synbiotic treatments.
One 12-week study demonstrated the impact of a synbiotic blend containing L. acidophilus, L. casei, B. bifidum, and 800 mg of inulin. The results showed a reduction in serum insulin by 2.8 µIU/mL and a decrease in HOMA-IR by 0.7, while the placebo group saw an increase in these markers. Synbiotics also significantly lowered C-reactive protein levels by 1.26 to 1.69 mg/L, pointing to reduced inflammation. For the best results in managing insulin resistance, look for formulations that combine multiple probiotic strains with prebiotics like inulin to enhance gut health and metabolic outcomes. These findings highlight the growing role of synbiotics in comprehensive PCOS care.
Using Probiotics with Other PCOS Treatments
Combining Probiotics with Metformin
Probiotics and Metformin can work together to address insulin resistance from different angles. While Metformin improves how cells respond to insulin, probiotics focus on gut health, helping to correct imbalances that might contribute to metabolic issues. For example, gut dysbiosis can increase intestinal permeability, allowing bacterial toxins like lipopolysaccharides to enter the bloodstream, which can disrupt insulin signaling .
When used together, these treatments may help restore the integrity of the intestinal barrier and further enhance insulin sensitivity. This combination approach takes advantage of probiotics' ability to improve metabolic markers when paired with conventional therapies . For the best results, consider multi-strain probiotic formulations and aim for an 8–12 week course. Companies like Oana Health offer personalized PCOS treatment plans that incorporate Metformin. For instance, Oral Metformin ER starts at $22/month, and combination options such as Metformin & Spironolactone are available for $32/month.
Personalized Treatment Plans with Oana Health
Tailored treatment plans can make a big difference in managing PCOS, especially since symptoms can vary widely - from hormonal imbalances to metabolic challenges. A personalized approach ensures that treatments are designed to meet your specific needs, making them more effective than a one-size-fits-all method.
At Oana Health, treatment plans combine options like Metformin, GLP-1 medications, and topical therapies. Licensed professionals create a plan based on your unique symptoms, whether you're addressing insulin resistance, weight management, or unwanted hair growth. These plans align with the gut-health-focused approach to PCOS and are conveniently delivered to your home. Options include Oral Metformin ER at $22/month, Metformin & Spironolactone at $32/month, Oral GLP-1 & Metformin at $199/month for advanced insulin resistance, and Topical Spironolactone at $43/month for targeting hair loss with reduced systemic effects.
Conclusion
Probiotics play a key role in improving insulin sensitivity for women with PCOS by focusing on gut health. By restoring the balance of gut bacteria, these beneficial microbes help reduce inflammation, strengthen the gut lining, and improve the body’s insulin response. Studies consistently show that regular probiotic use can lower important markers of insulin resistance .
Because PCOS presents differently in each individual, personalized treatment is essential. Its complex nature, particularly its effects on metabolism, often requires a combination of therapies for the best outcomes. Pairing probiotics with other proven treatments can offer a more comprehensive approach to managing PCOS symptoms.
Oana Health offers tailored PCOS treatment plans designed to address your specific symptoms and metabolic needs. From Metformin for insulin resistance to GLP-1 medications for weight management or topical solutions for hair loss, their medical team creates a plan just for you and delivers it right to your door.
FAQs
How can probiotics improve insulin resistance in women with PCOS?
Probiotics have shown promise in improving insulin resistance for women with PCOS by promoting a healthier gut microbiome. A well-balanced gut can support better metabolic function and help reduce inflammation. Research highlights that specific probiotic strains, such as Lactobacillus and Bifidobacterium, may reduce fasting glucose, insulin levels, and markers of insulin resistance like HOMA-IR by as much as 30% compared to a placebo.
These benefits are driven by several important mechanisms:
- Balancing gut bacteria: This encourages the production of short-chain fatty acids (SCFAs), which play a role in enhancing glucose uptake and improving insulin sensitivity.
- Strengthening the gut barrier: A stronger gut barrier helps prevent harmful endotoxins from entering the bloodstream, which can reduce inflammation.
- Regulating hormone levels: Probiotics can increase sex-hormone-binding globulin (SHBG) and lower testosterone levels, aiding in the restoration of healthy insulin signaling.
By addressing these underlying factors, probiotics can contribute to better metabolic health and help alleviate PCOS-related symptoms. For those seeking a tailored, science-driven approach to managing insulin resistance and PCOS, Oana Health offers telehealth programs designed to meet individual needs.
What makes synbiotics more effective than probiotics alone for managing insulin resistance?
Synbiotics, a blend of probiotics (helpful bacteria) and prebiotics (the fibers that nourish them), have shown promise in addressing insulin resistance. Studies indicate that synbiotics can lead to more noticeable decreases in fasting insulin levels and HOMA-IR (a marker for insulin resistance) compared to using probiotics alone. Beyond this, they may also aid in better glucose regulation, improved lipid levels, and hormonal balance, making them an effective option for supporting metabolic health.
By promoting a healthier gut environment, synbiotics could be especially beneficial for women dealing with conditions like PCOS, helping to manage insulin resistance and its associated symptoms more effectively.
How long does it take for probiotics to improve insulin sensitivity?
Most individuals begin to see changes in insulin sensitivity after consistently taking probiotics for 12 to 16 weeks. That said, the timeline can differ based on factors like diet, daily habits, and the type of probiotic strain being used.
The secret lies in staying consistent. Regular use gives probiotics the time they need to support gut health, a crucial player in the metabolic processes tied to insulin resistance.
