Synthetic Hormones vs Bioidentical: Long-Term Studies
Choosing between synthetic and bioidentical hormones for hormone therapy can significantly impact your health. Here's what you need to know:
- Bioidentical hormones are chemically identical to natural human hormones, derived from plants like soy and yams. They align closely with your body's natural processes.
- Synthetic hormones, such as conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA), differ structurally from natural hormones and may interact differently with your body.
Key Findings:
- Cancer Risk: Synthetic hormones (e.g., CEE + MPA) may slightly increase breast cancer risk, while bioidentical hormones (e.g., estradiol + micronized progesterone) appear to have a lower associated risk.
- Cardiovascular Health: Synthetic hormones, especially oral forms, can increase risks of blood clots and stroke. Transdermal bioidentical hormones bypass the liver, reducing these risks.
- Metabolic Effects: Bioidentical progesterone has a neutral effect on insulin resistance, unlike synthetic progestins, which may worsen it.
- Quality of Life: Both types relieve menopausal symptoms, but bioidentical hormones may improve sleep and mood stability more effectively.
Quick Comparison:
| Criteria | Synthetic Hormones | Bioidentical Hormones |
|---|---|---|
| Breast Cancer Risk | Increased (e.g., CEE + MPA) | Lower with estradiol + micronized progesterone |
| Stroke & Clots | Higher risk with oral forms | Lower risk with transdermal delivery |
| Insulin Resistance | May worsen | Neutral effect |
| FDA Regulation | Strictly regulated | FDA-approved options exist; compounded forms lack oversight |
| Mood & Sleep | MPA linked to negative effects | Often improves sleep and mood |
Bottom Line: Your choice should depend on your health history, age, and treatment goals. Consult a healthcare provider to determine the best option for you.
Synthetic vs Bioidentical Hormones: Long-Term Health Outcomes Comparison
1. Synthetic Hormones
Long-Term Safety
Synthetic hormones, such as conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA), have been under the microscope for years, primarily through the Women's Health Initiative (WHI). This study remains the cornerstone for understanding their long-term safety. While these hormones are chemically designed to mimic natural effects, they do have structural differences. Over an 18-year period, synthetic hormone therapy showed no increase in all-cause mortality (27.1% vs. 27.6%) or cardiovascular mortality (8.9% vs. 9.0%). However, specific risks were identified: estrogen-only therapy elevated the risk of stroke and venous thromboembolism (VTE) by 11 cases per 10,000 person-years, whereas adding progestin (MPA) increased VTE risk to 21 cases per 10,000 person-years. These findings highlight the importance of evaluating cancer risks tied to synthetic hormones.
Cancer Risk
When it comes to cancer risk, synthetic hormone therapies show distinct patterns. The CEE plus MPA combination was associated with an increase in invasive breast cancer cases - 9 additional cases per 10,000 person-years during the intervention phase. Specifically, 206 cases were reported in the hormone group compared to 155 in the placebo group. This elevated risk led to the trial’s early termination at 5.6 years. On the other hand, estrogen-only therapy, used in women who had undergone hysterectomies, showed a protective effect, reducing breast cancer risk over 13 years of follow-up (hazard ratio of 0.79). Furthermore, breast cancer mortality after 18 years was lower for women on estrogen-alone therapy (0.55) compared to those on combination therapy (1.44). While combination therapy appeared to decrease endometrial cancer risk, this benefit only became evident after the treatment ended.
Cardiovascular and Metabolic Outcomes
Synthetic progestins like MPA have raised concerns due to their effects on cardiovascular and metabolic health. They have been shown to increase insulin resistance and contribute to plaque formation. Alison Culkin, Superintendent Pharmacist at Roseway Labs, sheds light on the issue:
"Synthetic progestins... promote atherosclerotic plaque formation, [and] interfere with estrogen's protective effects and increase insulin resistance".
This is particularly concerning for women with conditions like PCOS, where insulin resistance is already a significant issue. The WHI CEE-alone trial also highlighted risks, ending after 7.2 years due to a higher likelihood of stroke. Despite these challenges, synthetic hormone therapy did offer some metabolic advantages. For example, estrogen-only therapy reduced diabetes risk by 19 cases per 10,000 person-years, while combination therapy lowered it by 14 cases. Additionally, fracture risk saw a notable decline, with 53 fewer cases per 10,000 person-years among estrogen-only users.
2. Bioidentical Hormones
Long-Term Safety
Bioidentical hormones are chemically identical to the ones your body naturally produces, making them distinct from synthetic alternatives. The FDA has approved several bioidentical hormone products, including specific estrogens and progesterone, after rigorous testing for safety and effectiveness. Despite this, an estimated 1–2.5 million U.S. women over 40 use compounded formulations, which are not regulated by the FDA. As highlighted by the National Academies of Sciences, Engineering, and Medicine:
"The FDA does not review or approve compounded preparations for safety, quality, or effectiveness".
For younger women aged 50–59, the likelihood of experiencing a major adverse event is less than 1 in 100 over five years of treatment. JoAnn Manson, Chief of the Division of Preventive Medicine at Brigham and Women's Hospital, underscores the importance of appropriate use:
"HT appears to have a favorable benefit:risk balance when used for treating menopausal symptoms and when used relatively short term, particularly in younger and recently menopausal women".
These insights provide a foundation for understanding the broader implications of bioidentical hormone use, including cancer risks.
Cancer Risk
The cancer risks associated with bioidentical hormones differ from those linked to synthetic therapies. A 13-year follow-up from the Women's Health Initiative revealed fewer cases of invasive breast cancer in the estrogen-alone trial group (104 cases) compared to the placebo group (135 cases), with the reduction becoming statistically significant after treatment ended. When bioidentical micronized progesterone is paired with estradiol, the risk of breast cancer appears lower than with synthetic progestins like medroxyprogesterone acetate. Alison Culkin, Superintendent Pharmacist, explains:
"The incidence of breast cancer seems to be lower in women treated with oestradiol and micronised progesterone (both bioidentical hormones), rather than with synthetic progestins".
For women with a uterus, combining bioidentical progesterone with estrogen is essential to prevent endometrial hyperplasia, which can lead to uterine cancer. However, hormone therapy is not recommended for individuals with a history of breast cancer.
Cardiovascular and Metabolic Outcomes
Bioidentical hormones stand out in their impact on cardiovascular and metabolic health, particularly when delivered transdermally. Transdermal 17β-estradiol bypasses the liver, which is thought to lower the risk of venous thromboembolism (VTE) and stroke compared to oral synthetic estrogens. A Swedish study conducted between 2007 and 2020, involving 919,614 women, found that oral continuous estrogen-progestin therapy was linked to a higher VTE risk (hazard ratio 1.61). Simon JA highlights the potential benefits of transdermal approaches:
"The use of transdermal oestradiol and micronized progesterone could may eliminate the excess risk of venous thromboembolism, stroke, cholecystitis, and possibly even breast cancer associated with oral HRT use".
Additionally, bioidentical progesterone does not seem to contribute to insulin resistance, unlike synthetic progestins. Both bioidentical and synthetic hormone therapies have been shown to reduce diabetes risk in long-term studies. For younger women (ages 50–59), estrogen-alone therapy has been linked to better outcomes for heart attack risk and all-cause mortality compared to older age groups.
Mood and Quality of Life
Beyond physical health, bioidentical hormones play an important role in improving quality of life. They help alleviate hot flashes, enhance sleep, and ease joint pain. However, side effects like breast tenderness, mood swings, and weight gain can occur. The Cleveland Clinic advises caution:
"Your risk of heart disease and breast cancer may also increase if you are older or use hormonal therapy for an extended period".
To minimize risks, it’s crucial to use the lowest effective dose for the shortest time necessary to manage symptoms. Women with a history of blood clotting disorders, heart disease, or stroke should consult their healthcare providers before starting hormone therapy.
Bio-Identical vs. Synthetic Hormones
sbb-itb-6dba428
Advantages and Disadvantages
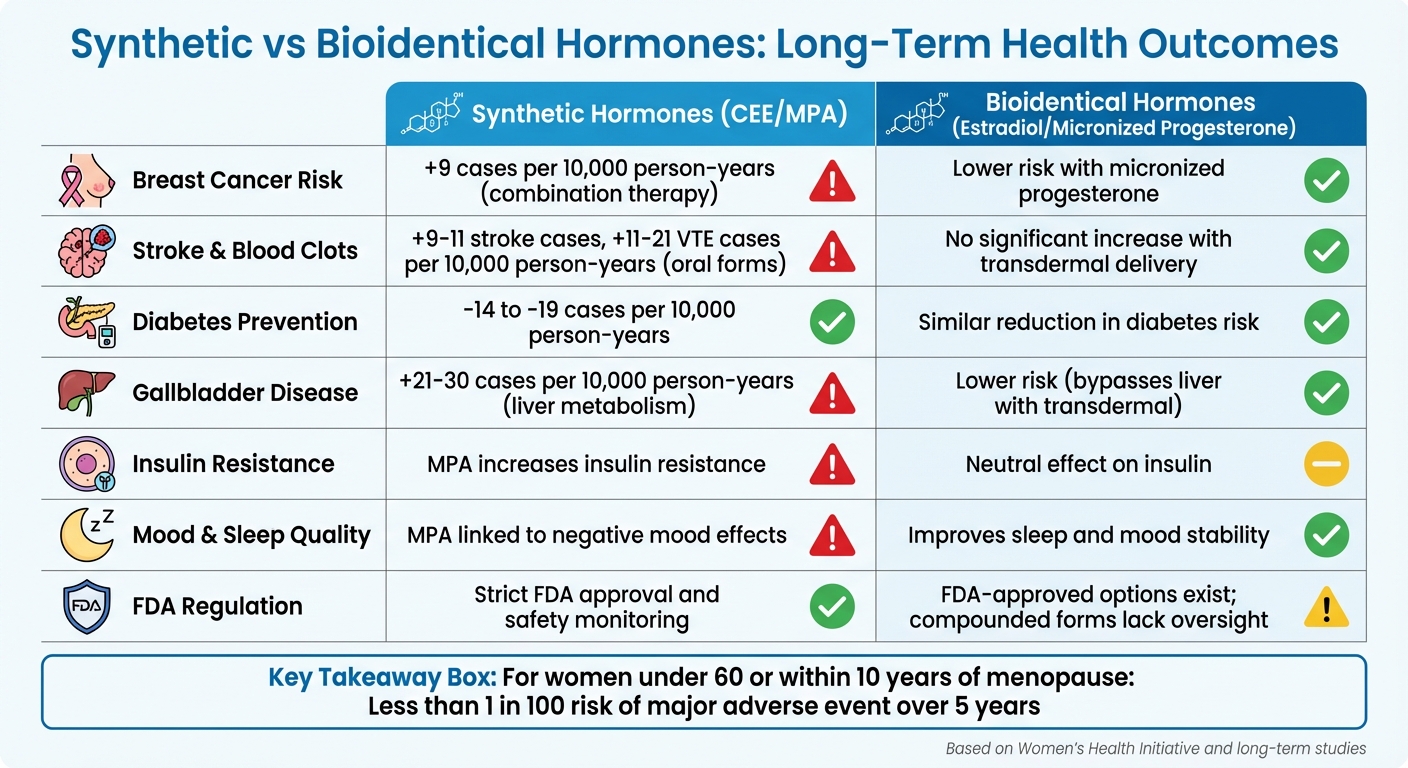
When comparing synthetic and bioidentical hormones, studies highlight distinct trade-offs. The table below outlines key differences based on long-term research, including findings from the Women's Health Initiative.
| Health Outcome | Synthetic Hormones (CEE/MPA) | Bioidentical Hormones (Estradiol/Micronized Progesterone) |
|---|---|---|
| Breast Cancer Risk | Increased by 9 cases per 10,000 person-years with combination therapy | Potentially lower risk with micronized progesterone compared to synthetic progestins |
| Stroke & Blood Clots | Oral forms raise stroke risk by 9–11 cases and venous thromboembolism (VTE) by 11–21 cases per 10,000 person-years | Transdermal estradiol shows no significant increase in VTE or stroke risk |
| Diabetes Prevention | Reduced by 14–19 cases per 10,000 person-years | Similar reduction in diabetes risk |
| Gallbladder Disease | Increased by 21–30 cases per 10,000 person-years due to liver metabolism | Lower risk with transdermal forms that bypass the liver |
| Mood & Sleep Quality | MPA linked to negative mood effects | Micronized progesterone improves sleep and mood stability |
| Metabolic Effects | MPA increases insulin resistance | Bioidentical progesterone appears to have a neutral effect on insulin |
| Regulatory Oversight | FDA-approved with strict safety monitoring | FDA-approved options exist, but compounded preparations lack oversight |
These findings highlight how hormone delivery methods and timing influence outcomes. Both synthetic and bioidentical hormones effectively reduce hot flashes and night sweats. However, transdermal bioidentical estradiol avoids liver metabolism, potentially lowering the production of clotting factors linked to oral synthetic estrogens.
Treatment timing also plays a crucial role. For women under 60 or within 10 years of menopause, the absolute risk of a major adverse event is less than 1 in 100 over five years. As Gerald Gartlehner, MD, MPH, explains:
"Hormone therapy for the primary prevention of chronic conditions in menopausal women is associated with some beneficial effects but also with a substantial increase of risks for harms".
Long-term studies emphasize the importance of safety monitoring alongside hormone composition. FDA-approved formulations provide rigorous oversight, while compounded bioidentical hormones - used by 1 to 2.5 million U.S. women over 40 - lack testing for purity, safety, or consistent dosing. These risks are not typically associated with FDA-approved products.
For women considering hormone therapy, evaluating personal risks and choosing FDA-approved options is key. Consulting with healthcare professionals, such as those at Oana Health, ensures treatments are tailored to individual needs.
Conclusion
Research indicates that both synthetic and bioidentical hormones can effectively address menopausal symptoms, but their risk profiles differ. Choosing the right option depends on factors like individual health history, age, and specific treatment goals.
The way these hormones are formulated also plays a significant role in their safety. For example, transdermal estradiol and micronized progesterone (forms of bioidentical hormones) are associated with a lower risk of blood clots and strokes because they bypass the liver during metabolism. JoAnn Manson, a Professor of Medicine at Harvard Medical School, emphasizes the importance of tailoring treatments to the individual:
"It will become very important to do risk stratification... to individualize and personalize HT treatment, and clinicians will need to be given the latitude to use clinical judgment".
These insights extend beyond menopause to conditions like PCOS. While synthetic birth control pills are often the first-line treatment for managing androgen levels, bioidentical progesterone can aid in regulating the endometrial lining. Combined with lifestyle changes, this approach can help reduce long-term complications.
Telehealth platforms like Oana Health make it easier to access FDA-approved, customized hormonal therapies. With professional guidance, treatments are adjusted based on clinical symptoms rather than unreliable hormone level tests. For women dealing with PCOS symptoms like unwanted facial hair, hair loss, or insulin resistance, this ongoing support can be invaluable.
As discussed, the type of hormone formulation and how it’s delivered are key factors in achieving better long-term outcomes. By working closely with knowledgeable healthcare providers, women can ensure their hormone therapy aligns with their health needs and minimizes potential risks.
FAQs
What are the key differences between synthetic and bioidentical hormones?
Synthetic hormones are lab-created substances crafted to imitate natural hormones, though their molecular structure differs from those the body naturally produces. These hormones are generally FDA-approved and must pass strict testing to ensure their safety and effectiveness.
Bioidentical hormones, in contrast, are formulated to have the exact molecular structure of the hormones your body makes. They may also be FDA-approved, but some are compounded in specialized pharmacies using plant-based sources. It's important to note that compounded bioidentical hormones can vary in purity and aren’t held to the same regulatory standards as their FDA-approved counterparts.
Grasping these distinctions is key when exploring hormone therapy, as they can influence factors like safety, effectiveness, and how well the treatment suits an individual over time.
What impact do bioidentical hormones have on cardiovascular health compared to synthetic hormones?
Long-term research suggests that bioidentical hormones might pose a lower or similar risk for cardiovascular problems compared to synthetic hormones. However, the findings aren't entirely clear-cut, as some studies have not identified a clear safety edge.
One reason bioidentical hormones are often highlighted is their molecular structure, which closely mirrors the body's natural hormones. This similarity may play a role in their potential cardiovascular advantages. Still, any decision about treatment should be made in partnership with a licensed healthcare provider, taking into account your individual health profile and potential risks.
Are bioidentical hormones less likely to increase cancer risk compared to synthetic hormones?
When it comes to hormone therapy, there's currently no solid proof that bioidentical hormones are safer or pose a lower cancer risk compared to synthetic hormones. Both options have comparable safety profiles when used correctly and under the guidance of a healthcare professional.
The key is to work closely with a licensed healthcare provider who can evaluate your individual needs and health situation. This personalized approach ensures you receive the safest and most effective hormone therapy for your circumstances.
