Common Problems with Hormonal Acne Treatments and Solutions
Hormonal acne is tricky to treat because it’s tied to internal hormone imbalances. Standard treatments like antibiotics often fail since they don’t address the root cause. Even effective options like spironolactone or oral contraceptives take months to show results, leading to frustration and dropout. High relapse rates after stopping treatment and side effects like irregular bleeding or nausea add to the challenges.
The best way to manage hormonal acne is with a combination of approaches: hormonal blockers (like spironolactone), topical treatments (retinoids or azelaic acid), and lifestyle changes (diet adjustments for insulin resistance). Addressing underlying conditions like PCOS or stress is also key. Maintenance therapy is crucial to prevent relapses, and regular monitoring ensures treatments remain effective. For long-term success, consistency and a tailored plan are essential.
Treating HORMONAL Adult Acne
Common Problems with Hormonal Acne Treatments
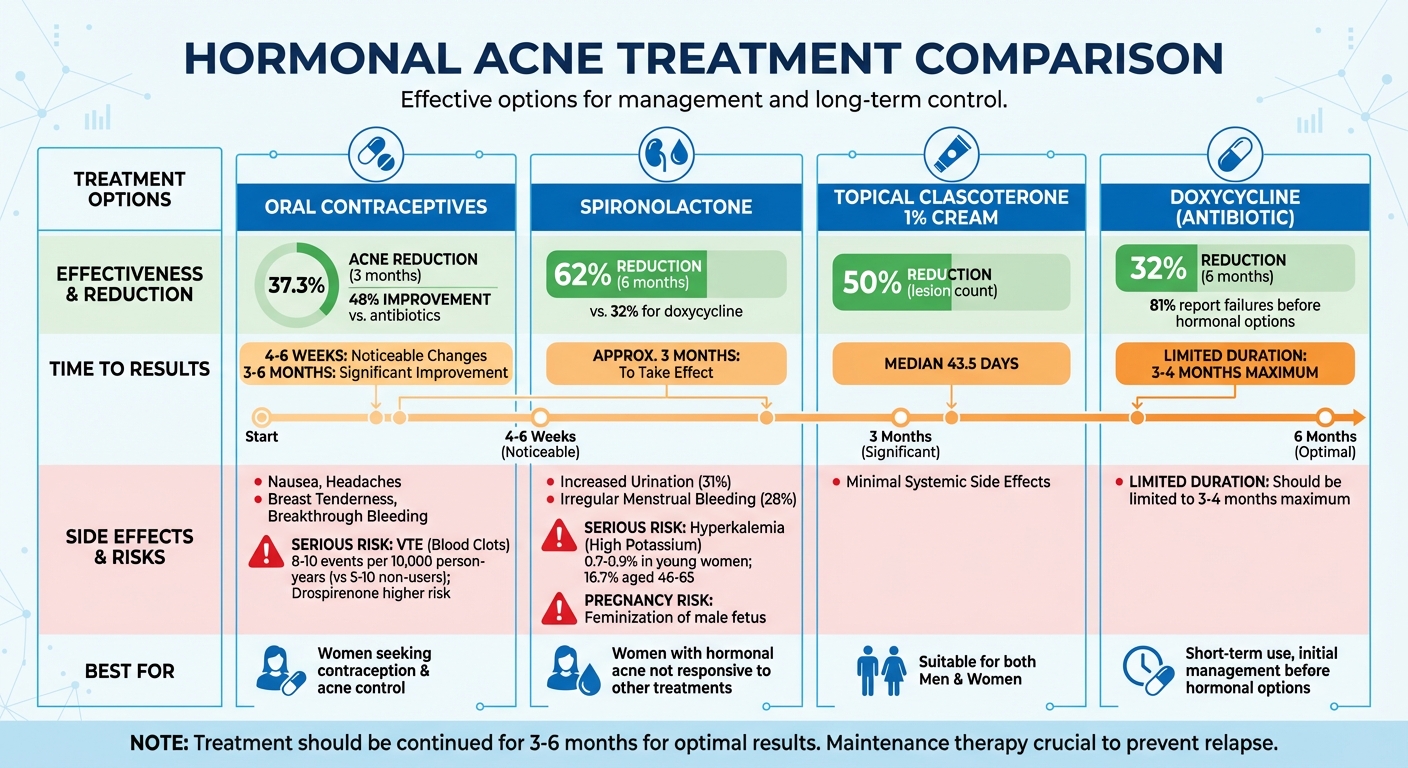
Hormonal Acne Treatment Comparison: Effectiveness, Timeline, and Side Effects
Slow Results and Patient Frustration
Hormonal treatments like combined oral contraceptives and spironolactone work by targeting androgen activity, but they often take time to show visible results. For instance, oral contraceptives can reduce acne by 37.3% after three months, with improvements reaching 48% over a similar period when compared to antibiotics. Spironolactone typically requires around three months to take effect, while topical clascoterone 1% cream achieves a 50% reduction in lesion count after a median of 43.5 days.
This slow progress can be discouraging, leading many patients to abandon treatment before it reaches its full potential. Setting realistic expectations is crucial - patients should be informed that noticeable changes might take four to six weeks, with significant improvements often requiring three to six months.
"Treatment of acne can be difficult due to its long time course, chronicity, and low patient adherence." - James Q. Del Rosso, Dermatologist
When treatments are stopped prematurely, patients face the risk of relapse, creating additional challenges.
High Relapse Rates After Stopping Treatment
Hormonal acne is not a one-time issue; it’s a chronic condition. The underlying androgen activity that drives the acne doesn’t disappear once treatment stops. This is why maintenance therapy is so important. Continuing treatment even after the skin clears helps prevent new breakouts, as the hormonal imbalance remains active beneath the surface.
Side Effects and Safety Concerns
Hormonal treatments come with their own set of challenges. Combined oral contraceptives may cause side effects like nausea, headaches, breast tenderness, and breakthrough bleeding. Rare but serious risks include venous thromboembolism (VTE), with approximately 8–10 events per 10,000 person-years among users, compared to 5–10 events in non-users. Drospirenone-containing contraceptives carry a slightly higher VTE risk compared to those with levonorgestrel.
Spironolactone, another common treatment, can lead to side effects like increased urination (31% of users) and irregular menstrual bleeding (28%). While the risk of hyperkalemia (high potassium) is low in young women (0.7%–0.9%), it rises significantly to 16.7% in older women aged 46–65. Additionally, spironolactone poses risks during pregnancy, as it may cause feminization of a male fetus, making effective contraception essential. Other treatments, such as flutamide and high-dose cyproterone acetate, carry risks of severe liver damage, necessitating regular liver function monitoring.
"Spironolactone provides a safe low-cost alternative to reduce use of oral antibiotics for women with persistent acne, suitable for use in primary care." - NIHR Health and Social Care Delivery Program
To manage side effects, combining treatments can be effective. For example, pairing spironolactone with oral contraceptives can regulate menstrual cycles and reduce breakthrough bleeding. For gastrointestinal issues, starting metformin at a low dose (500 mg) and taking it with meals can improve tolerance.
Poor Response to Single Treatments
Treating hormonal acne with a single approach often falls short because it addresses only one of the four key pathways: sebum production, keratinization, bacterial growth, or inflammation. For example, antibiotics target bacteria and inflammation but fail to tackle the hormonal triggers. This explains why 81% of women report treatment failures with systemic antibiotics before turning to hormonal options.
Topical treatments alone are also insufficient for moderate to severe hormonal acne. Sebaceous glands can produce active androgens like DHT locally, even when systemic androgen levels appear normal in blood tests.
In a study comparing spironolactone (150 mg/day) to doxycycline (100 mg/day) over six months, spironolactone reduced global acne scores by 62%, compared to doxycycline’s 32% reduction. This highlights the importance of addressing the hormonal root cause rather than just surface symptoms. Tackling all pathways is essential, as will be explored in the next section on comprehensive treatment strategies.
Untreated Underlying Causes
Conditions like PCOS, nonclassic congenital adrenal hyperplasia, and insulin resistance often drive hormonal acne. Research shows that over half of adult acne patients have elevated androgen levels. Women with PCOS, for instance, are 1.6 times more likely to experience acne than those without the condition.
Diet and lifestyle also play a role. High-glycemic diets can spike insulin levels, triggering androgen fluctuations and increasing sebum production. Stress adds to the problem by releasing corticotrophin-releasing hormone (CRH), which stimulates sebaceous glands. Genetics can’t be overlooked either - 50% of patients with postadolescent acne report having a first-degree relative with the condition.
"Increased androgen production plays a major role in inducing the sebum alterations that participate to the pathogenesis of adult acne." - Enrico Carmina, MD, Endocrinology Unit, University of Palermo
Without addressing these underlying issues - such as screening for hyperandrogenism or managing insulin resistance - treatments are unlikely to succeed in the long term. Tailored combination therapies are key to effective and lasting management.
Solutions: Evidence-Based Approaches to Hormonal Acne
Combining Hormonal and Topical Therapies
Pairing oral hormonal treatments with topical solutions addresses both internal hormonal triggers and external skin concerns. Medications like spironolactone or combined oral contraceptives help reduce androgen-driven oil production, while topical treatments work directly on the skin's surface. This combination provides a dual approach to managing hormonal acne.
For instance, using topical retinoids alongside oral spironolactone accelerates the clearing of clogged pores and prevents new breakouts. Starting with a mild formulation - such as retinol 0.25% combined with niacinamide 2% - can reduce irritation, with gradual increases as your skin adjusts. Additionally, a 2.5% micronized benzoyl peroxide formulation is effective for controlling bacteria while being gentle enough for sensitive skin, a common issue in adult hormonal acne.
"Hormonal therapies are essential strategies to treat acne. Clinicians should expand the use of existing and emerging hormone therapy as part of their acne treatment strategies." - The Author(s), PubMed
Another promising option is clascoterone, a topical anti-androgen that blocks androgen receptors in the skin with minimal systemic side effects. This makes it a good choice for both men and women who may not tolerate oral hormonal treatments. To support the skin barrier while using potentially drying treatments like benzoyl peroxide or retinoids, non-comedogenic, oil-free moisturizers with niacinamide are highly recommended.
Addressing underlying metabolic factors is also crucial for a comprehensive treatment plan.
Treating PCOS and Insulin Resistance
For women with PCOS, managing insulin resistance is a key step in controlling acne long term. Insulin resistance contributes to increased androgen production by lowering levels of sex hormone-binding globulin (SHBG) and stimulating androgen production in the ovaries and adrenal glands. Women with PCOS are also at a higher risk for type 2 diabetes and metabolic syndrome.
Tackling metabolic issues complements hormonal and topical therapies for a well-rounded approach. For those who are overweight, weight loss and calorie-restricted diets are effective first steps to reduce insulin resistance and improve overall health. Metformin, an insulin-sensitizing medication, is another option, restoring regular menstrual cycles in 50% to 70% of women with PCOS. It’s also affordable, costing around $4 per month for a typical dosage.
All women diagnosed with PCOS should undergo screening for type 2 diabetes using a two-hour oral glucose tolerance test. Additional evaluations for dyslipidemia and hypertension are crucial, regardless of body weight. For cases where standard treatments fall short, combining oral contraceptives with anti-androgens like spironolactone often yields better results. In more severe cases of hyperandrogenism, consulting a reproductive endocrinologist may be necessary for specialized care.
Reducing Antibiotic Use and Resistance
Minimizing antibiotic use is essential for long-term acne management, especially to prevent bacterial resistance. Oral antibiotics should be limited to 3–4 months for moderate-to-severe flare-ups and should never be used alone. Combining topical antibiotics with benzoyl peroxide or retinoids helps eliminate the risk of resistance.
"Concurrent use of benzoyl peroxide eliminates the risk of resistance development." - Medscape
Once significant improvement is achieved, transitioning to long-term maintenance with topical retinoids like tretinoin, adapalene, or tazarotene is key. For women experiencing cyclical flares or signs of hyperandrogenism, spironolactone (25–200 mg daily) or specific oral contraceptives are more effective alternatives to repeated antibiotic courses. These options address the root cause of acne rather than just managing symptoms temporarily.
Here’s a quick guide to treatment strategies that reduce antibiotic resistance while maintaining effectiveness:
| Treatment Type | Recommended Use | Role in Reducing Resistance |
|---|---|---|
| Oral Antibiotics | Limited to 3–4 months for moderate-to-severe flares | Short-term use only; never used alone |
| Benzoyl Peroxide | Topical application, often in fixed-dose combinations | Prevents/eliminates antibiotic resistance |
| Topical Retinoids | Long-term maintenance therapy | Non-antibiotic; normalizes skin cell turnover |
| Spironolactone | Systemic treatment for women (25–200 mg/day) | Non-antibiotic alternative targeting sebum production |
Building an Effective Skin-Care Routine
A solid skin-care routine supports medical treatments and helps maintain results over time. Non-comedogenic, oil-free moisturizers are crucial for keeping the skin barrier healthy, especially when using drying treatments like retinoids or benzoyl peroxide. Gentle cleansers with low-strength salicylic acid (0.5%) are another option to clean the skin without irritation.
Daily application of mineral-based, non-comedogenic sunscreen is a must, particularly when using retinoids. Harsh scrubs and over-washing should be avoided, as they can strip the skin and trigger increased oil production. Adjusting your diet to reduce dairy and refined sugars may also help by lowering systemic inflammation.
Consistency is key. Stick with combination treatments for at least four to six weeks to see noticeable improvement. For those seeking personalized care, Oana Health offers telehealth consultations with licensed medical professionals who can prescribe and deliver treatments directly to your home. This tailored approach ensures you’re on the right path to managing hormonal acne effectively.
sbb-itb-6dba428
Developing a Long-Term Acne Management Plan
Keeping acne under control for the long haul requires a well-thought-out plan and regular adjustments to maintain clear skin after initial improvements.
Regular Monitoring and Treatment Adjustments
Hormonal acne is a chronic condition, meaning it needs consistent care and monitoring. Plan to check in with your dermatologist every 4–6 weeks to evaluate how your treatment is working and make necessary adjustments. For example, spironolactone dosages often start at 50 mg daily and can be gradually increased up to 200 mg over 4–6 week intervals. If you're using oral contraceptives, keep an eye on your blood pressure, and for those with kidney or heart conditions, potassium levels should also be monitored.
Pay attention to changes in your menstrual cycle - spironolactone can sometimes cause mid-cycle bleeding, which might signal the need for a dose adjustment or the addition of an oral contraceptive. If topical retinoids are causing irritation, try applying them less frequently or layering them over a moisturizer to reduce discomfort. These small but critical tweaks can help you establish a stable, long-term treatment routine.
Transitioning to Maintenance Therapy
Once your acne is under control, the next step is maintenance. This phase focuses on preventing new breakouts and avoiding relapse. A combination of hormonal therapies like spironolactone or oral contraceptives with topical treatments such as retinoids or azelaic acid works well for this purpose. This approach also helps reduce the risk of antibiotic resistance and minimizes the long-term side effects of systemic medications.
Spironolactone, for instance, has been shown to be safe for long-term use, with an eight-year study reporting that only 15% of users stopped due to side effects. For those looking for alternative options, topical treatments like clascoterone can also be effective, though they can be pricey. The key to success here is consistency - sticking to your maintenance plan even after your skin clears significantly lowers the chances of a relapse.
The Benefits of Personalized, Integrated Care
Long-term acne management works best when it's tailored to your unique needs, combining hormonal, metabolic, and targeted treatments. For those with underlying conditions like PCOS or insulin resistance, adding metformin (500–2,000 mg daily) to hormonal therapies can address the root causes of acne.
For a more personalized approach, services like Oana Health offer integrated care plans delivered right to your home. This kind of coordinated strategy ensures that your treatment evolves alongside your body's needs, helping you maintain clear skin for the long term. By addressing the underlying factors and staying consistent, you can make acne a thing of the past.
Conclusion: Managing Hormonal Acne with a Complete Approach
Dealing with hormonal acne calls for a well-rounded strategy that tackles the issue from multiple angles. The most effective plans often combine hormonal therapies, like spironolactone or oral contraceptives, with topical treatments such as retinoids or azelaic acid. Together, these treatments address the various factors that contribute to acne. Studies confirm that this combined approach leads to higher success rates in achieving clear or nearly clear skin compared to relying on a single treatment method. Beyond just clearing up acne, this approach helps lay the groundwork for better long-term skin health.
Another major advantage of combination therapy is its ability to prevent antibiotic resistance while minimizing scarring and pigmentation. It also makes transitioning from active treatment to maintenance therapy smoother, ensuring lasting results without the need for prolonged antibiotic use. This balanced approach aligns with earlier research emphasizing the importance of addressing both the immediate symptoms and the underlying hormonal causes of acne.
"Hormonal therapies are essential strategies to treat acne. Clinicians should expand the use of existing and emerging hormone therapy as part of their acne treatment strategies." - Howa Yeung, MD, Emory University School of Medicine
Maintaining these results requires ongoing, personalized care. Tailored treatments that address underlying health issues, such as PCOS or insulin resistance, play a key role. Services like Oana Health provide integrated care plans, combining hormonal therapies, topical solutions, and lifestyle support - all conveniently delivered to your door. This kind of coordinated care ensures your treatment adapts to your changing needs, giving you the best chance at maintaining clear and healthy skin over time.
FAQs
Why does it take so long to see results from hormonal acne treatments?
Hormonal acne treatments require patience because they tackle the underlying issue: hormonal imbalances. These treatments work by slowly balancing hormone levels and controlling the production of excess oil (sebum). Once this process is underway, the skin’s natural turnover cycle, which typically takes 4 to 6 weeks, begins to clear up existing acne.
Sticking to your treatment plan consistently is key. While results won’t appear overnight, gradual improvements over weeks or even months are a normal part of the healing process as your skin adapts and recovers.
What happens if you stop hormonal acne treatment too early?
Stopping hormonal acne treatment too soon can bring on a rebound flare-up, reversing the improvements you’ve worked hard to achieve. On top of that, you might deal with side effects like redness, dryness, peeling, and irritation - all of which can leave your skin feeling sensitive and uncomfortable.
To keep your progress on track and prevent setbacks, stick to your treatment plan exactly as prescribed by your healthcare provider. If you’re thinking about stopping or switching treatments, make sure to consult with your provider first. They can help guide you through a smooth transition and minimize any potential issues.
What can I do to reduce side effects from hormonal acne treatments?
Managing the side effects of hormonal acne treatments is a key part of achieving clearer, healthier skin while keeping discomfort at bay. The first step? Stay in close contact with your healthcare provider to tweak your treatment plan when necessary. Often, combining low-dose oral medications - like spironolactone or birth control pills - with topical options such as retinoids or benzoyl peroxide can help reduce side effects without compromising effectiveness.
To keep your skin protected and comfortable, use a gentle, fragrance-free moisturizer to counteract dryness and peeling. Daily application of a broad-spectrum sunscreen with SPF 30 or higher is also essential, as many treatments can increase your skin's sensitivity to sunlight, leading to irritation or hyperpigmentation. Taking oral medications with food can help prevent stomach upset, and drinking plenty of water supports your skin's overall health. If you notice persistent or severe side effects, such as headaches or significant irritation, reach out to your provider for guidance on adjusting your regimen.
By pairing the right treatments with proper skin care and maintaining open communication with your healthcare team, you can effectively manage side effects and stay on track toward achieving clearer, more comfortable skin.
