Long-Term BHRT Use: Immune System Effects Explained
Hormones influence more than just menopause symptoms - they directly impact your immune system. Bioidentical Hormone Replacement Therapy (BHRT) aims to restore hormonal balance, potentially reducing inflammation and slowing immune aging. But long-term use comes with risks, including chronic inflammation, autoimmune conditions, and higher infection susceptibility.
Key Takeaways:
- What BHRT Does: BHRT uses plant-derived hormones identical to those in your body to manage menopause symptoms and immune changes.
- Immune Benefits: Estrogen and progesterone can lower inflammation, while testosterone modulates immune cell activity.
- Risks: Long-term BHRT may increase autoimmune risks, disrupt infection defenses, and lead to low-grade inflammation.
- Monitoring: Regular check-ups and tracking inflammatory markers are essential during BHRT.
- Lifestyle Tips: Anti-inflammatory diets, exercise, and stress management can help mitigate risks.
Balancing the benefits and risks of BHRT requires careful monitoring and personalized care. Learn how to protect your immune health while using BHRT.
How BHRT Affects the Immune System
How Hormones Regulate Immune Responses
Bioidentical Hormone Replacement Therapy (BHRT) influences immune cell activity by interacting directly with their receptors. When hormones like estrogen or testosterone are introduced through BHRT, they bind to receptors on immune cells - such as T cells, B cells, and macrophages - triggering a cascade of changes that can shape long-term immune function. Essentially, these hormones act as messengers, linking the endocrine system to immune responses.
Estrogen, for instance, plays a role in reducing inflammation. It achieves this by blocking the NF-κB pathway, which reduces the production of inflammatory molecules like IL-6 and TNF-α. Think of NF-κB as a master switch for inflammation - when estrogen interferes with it, the body generates fewer pro-inflammatory signals. Estrogen also shifts macrophages from an "M1" profile, which promotes inflammation and tissue damage, to an "M2" profile, which aids in tissue repair. Additionally, it encourages T helper cells to adopt a Th2 profile, favoring anti-inflammatory responses over aggressive immune attacks.
"Estrogens, and in particular E2, can control the proinflammatory signals/pathways of the immune system." – Alfred T. Harding, Massachusetts Institute of Technology
Testosterone presents a more nuanced picture. While it generally suppresses certain immune activities, it also amplifies monocyte responses, leading to increased production of TNF, IL-6, and IL-15. A 12-month study conducted at the Karolinska Institutet found that testosterone therapy raised SLAMF7 expression on monocytes, enhancing TNF responses. It also activated NF-κB-regulated genes in T cells and NK cells while reducing IRF7 expression in dendritic cells, which weakened type-I interferon responses.
Progesterone, on the other hand, has its own role in immune regulation. It promotes immune tolerance and helps maintain an anti-inflammatory environment. Together, these hormones create a delicate balance. Both estrogen and testosterone contribute anti-inflammatory effects, which can help restore hormonal levels, reduce systemic inflammation, and even increase pain thresholds.
These hormone-driven changes set the stage for the more lasting immune system adjustments observed with prolonged BHRT use.
Long-Term Immune Changes from BHRT
Over time, BHRT leads to sustained shifts in immune function. One key benefit is its ability to counteract "inflamm-aging", a chronic, low-level inflammation commonly associated with menopause. Research shows that menopausal hormone therapy (MHT) can lower elevated levels of pro-inflammatory cytokines like TNF-α, IFN-γ, and IL-6 in postmenopausal women. In one clinical trial, oral MHT reduced IL-1β levels from a median of 0.46 pg/mL to 0.26 pg/mL within just 12 weeks.
The method of hormone delivery also plays a role. Oral MHT has been shown to boost NK cells and B lymphocytes while reducing MCP-1, a pro-inflammatory marker. Meanwhile, transdermal MHT appears to enhance T-helper cell activity and increase anti-inflammatory markers like CD206 on monocytes. These findings suggest that the route of administration can influence which immune cells respond most strongly.
Long-term use of BHRT can also impact immune tolerance - the body's ability to differentiate between harmful threats and harmless substances. Some studies suggest that BHRT may suppress T-cell reactivity to mitogens, though this effect seems less pronounced in women who maintain an active lifestyle. Additionally, the therapy tends to shift the balance of T-helper cells, reducing Type 1 cytokines (like IL-2 and IFN-γ) while increasing Type 2 cytokines (like IL-4).
"The suppressive effect of HRT on T cell function in postmenopausal women may be attenuated by a physically active lifestyle." – Mark L. Failla et al.
BHRT can even prompt epigenetic changes that reprogram immune responses. For example, the 12-month testosterone study highlighted increased chromatin accessibility and transcription factor activity at NF-κB binding sites in T cells and NK cells. Testosterone also boosts the expression of SOCS1 and SOCS3 - proteins that act as negative regulators to dampen type-I interferon responses.
The overall effect is a recalibrated immune system that produces fewer inflammatory signals while maintaining its protective functions. However, achieving this balance requires careful monitoring, as the line between helpful immune modulation and excessive immune suppression can be razor-thin.
BHRT, Your Immune System, and Your Health Part 2
Immune Health Risks of Long-Term BHRT Use
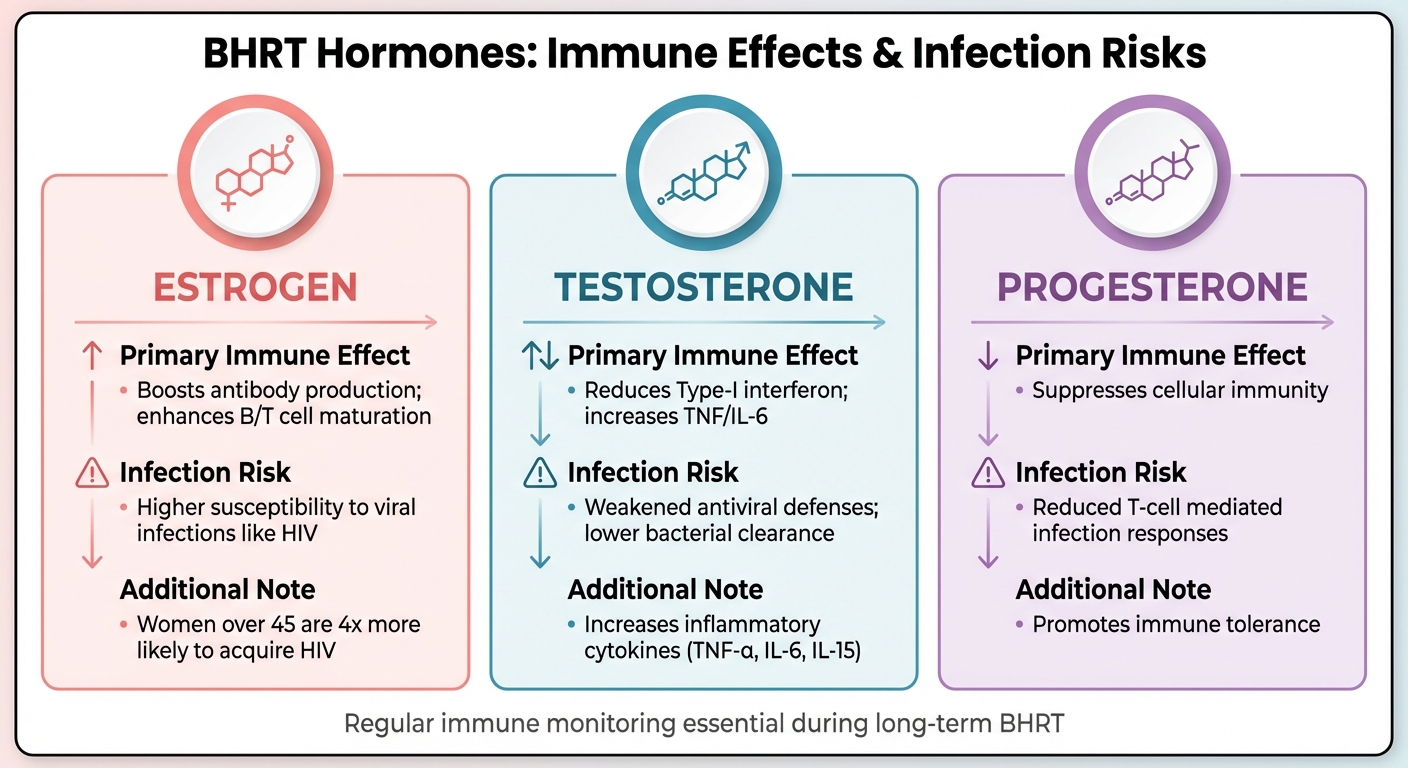
How Different BHRT Hormones Affect Immune Function and Infection Risk
While BHRT (Bioidentical Hormone Replacement Therapy) can influence immune function in positive ways, prolonged use introduces risks that may develop over time.
Chronic Inflammation from BHRT
Testosterone therapy is known to increase monocyte activity, which in turn ramps up the production of pro-inflammatory cytokines like TNF-α, IL-6, and IL-15. A study published in Nature in July 2024 followed 23 trans men undergoing testosterone therapy over a 12-month period. Blood samples taken at the start, 3 months, and 12 months into treatment revealed that testosterone activated key inflammatory pathways in T cells and natural killer cells. The therapy also disrupted a balance between type-I interferon and TNF, leading to increased inflammatory cytokine production alongside reduced antiviral defenses.
"Testosterone modulates a cross-regulated axis between type-I interferon and tumour necrosis factor." – Nature
This persistent low-grade inflammation differs from the acute inflammation that helps fight infections. Over time, it can contribute to immune imbalances and potential health complications.
Immune Dysregulation and Autoimmune Conditions
The inflammation caused by long-term BHRT can also lead to immune dysregulation, potentially triggering autoimmune conditions - especially in individuals already predisposed. Estrogen-based therapies, for example, enhance B-cell maturation and antibody production, which can sometimes worsen or even initiate autoimmune diseases like Systemic Lupus Erythematosus (SLE) and Sjögren's syndrome.
A large-scale study involving nearly 1.8 million women (average age 60.5) found a notable link between hormone therapy and the onset of autoimmune diseases, including lupus and rheumatoid arthritis. Women already face a fourfold higher risk of autoimmune disorders compared to men, and hormone therapy may amplify this vulnerability. Additionally, hormone-induced effects on the AIRE gene in the thymus - which normally helps prevent autoreactive T cells from entering circulation - could play a role in this process.
"Our study found a statistical link between hormone therapy and autoimmune diseases, but the actual increase in absolute risk is relatively small and varies by condition." – Dr. Xuezhi (Daniel) Jiang, Professor of Obstetrics and Gynecology, Drexel University College of Medicine
Beyond the risk of autoimmune flares, extended hormone therapy can disrupt the CD4⁺:CD8⁺ T cell ratio and weaken natural killer cell activity. This may accelerate immune-senescence, a process where the immune system ages prematurely and becomes less effective at responding to threats.
Higher Risk of Infections
Long-term BHRT can also compromise the immune system’s ability to fight infections. Testosterone therapy has been shown to reduce IFNα responses and impair neutrophil function, weakening defenses against viruses and bacteria. The same 12-month study noted a significant reduction in hallmark interferon-α responses, which further weakened antiviral immunity. Testosterone treatment has also been linked to increased markers of T-cell exhaustion, such as TIGIT, which can diminish adaptive immune responses.
For women on estrogen-based BHRT, the immune changes are different but equally concerning. While estrogen can help restore beneficial vaginal lactobacilli and lower the risk of urinary tract infections, research shows that women over 45 are four times more likely to acquire HIV. This increased risk may be tied to hormone-induced upregulation of CCR5 coreceptors on cervical CD4 T cells. Additionally, 10% to 15% of women over 60 experience recurrent urinary tract infections, a risk potentially linked to hormone-driven changes in the vaginal microbiome and local immune defenses.
| Hormone Type | Primary Immune Effect | Infection Risk |
|---|---|---|
| Estrogen | Boosts antibody production; enhances B/T cell maturation | Higher susceptibility to viral infections like HIV |
| Testosterone | Reduces Type-I interferon; increases TNF/IL-6 | Weakened antiviral defenses; lower bacterial clearance |
| Progesterone | Suppresses cellular immunity | Reduced T-cell mediated infection responses |
These varying immune effects highlight the importance of regular immune health monitoring for individuals undergoing long-term BHRT.
sbb-itb-6dba428
How to Protect Your Immune System During BHRT
Long-term BHRT doesn't have to interfere with your immune health. With the right monitoring, lifestyle changes, and personalized medical care, you can support your immune system while taking advantage of hormone therapy. Start by keeping an eye on key hormonal and inflammatory markers to catch any changes early.
Regular Immune System Monitoring
Tracking hormone levels is essential. Establish baseline levels for total testosterone and SHBG, and recheck them at 3 and 6 months to ensure they stay within premenopausal ranges.
It’s also important to monitor inflammatory markers. Menopause naturally leads to "inflammaging", a condition of chronic, low-grade inflammation characterized by elevated cytokines like IL-6, TNF-α, and MCP-1. Keeping tabs on these markers can provide valuable insights, especially since inflammation levels often decrease with hormone therapy in postmenopausal women.
"Monitoring hormone or drug levels does not correlate with the effectiveness or safety of HRT for managing vasomotor symptoms. Instead, clinicians should focus on assessing symptom relief and potential adverse effects." – StatPearls
Additionally, hormonal changes during BHRT can impact the vaginal microenvironment, potentially increasing the risk of urinary or vaginal infections. Regular monitoring for these issues is crucial.
Anti-Inflammatory Lifestyle Changes
Lifestyle adjustments can go a long way in reducing inflammation. A Mediterranean diet, rich in fruits, vegetables, nuts, whole grains, fatty fish, and olive oil, can provide antioxidants and help lower inflammation. Adding omega-3 fatty acids from sources like salmon, mackerel, or sardines can further support this effort.
Equally important is cutting back on foods that can fuel inflammation. Refined carbs (like white bread and pastries), processed meats, sugary drinks, and trans fats found in margarine are common culprits. How you cook matters too - opt for baking, steaming, or quick stir-frying instead of deep-frying or grilling at high heat, which can produce inflammatory compounds.
"Many experimental studies have shown that components of foods or beverages may have anti-inflammatory effects." – Dr. Frank Hu, Professor of Nutrition and Epidemiology, Harvard School of Public Health
Supporting your gut health is another key step. Probiotic-rich foods like yogurt with live active cultures, along with prebiotic fibers found in asparagus, bananas, and chicory, can help regulate your immune system. Regular exercise, stress management, and steering clear of smoking and excessive alcohol also play a role in maintaining immune function during BHRT.
Personalized Telehealth Support from Oana Health
For the best results, combine your monitoring and lifestyle changes with expert medical advice. The FDA advises using the lowest effective hormone doses for the shortest necessary duration. Personalized care ensures your hormone therapy is tailored to your needs, including the type, dose, and delivery method.
Oana Health provides customized telehealth consultations with licensed professionals specializing in female hormone management. Through virtual check-ups, providers can assess your symptoms and make adjustments to your treatment plan if needed.
The delivery method you choose also impacts your immune health. Transdermal estradiol patches or gels are often preferred over oral options because they bypass the liver. If your uterus is intact, your provider will include a progestogen in your BHRT plan to prevent endometrial hyperplasia.
"HRT management individualized to the lowest effective dose that relieves symptoms is recommended." – StatPearls
Conclusion
Long-term use of BHRT may help counteract immune aging by stabilizing cellular responses and reducing chronic inflammation associated with higher levels of IL-6 and TNF-α in postmenopausal women. When carefully administered, BHRT could also support a healthier immune system by increasing B-cell numbers and improving T-cell function.
Personalized treatment and consistent monitoring are key. The FDA advises using the lowest effective dose for the shortest time necessary to manage symptoms while minimizing potential risks.
Incorporating lifestyle changes like an anti-inflammatory diet, regular physical activity, stress reduction, and avoiding smoking can further reduce inflammation and strengthen immune health alongside BHRT.
Selecting the right delivery method is also important. Transdermal estrogen, for instance, avoids the liver and lowers the risk of blood clots compared to oral options. For women with a uterus, including a progestogen is crucial to prevent endometrial complications. Together, these approaches can help ensure safer and more effective results with BHRT.
FAQs
What are the potential effects of long-term BHRT use on the immune system?
Long-term use of bioidentical hormone replacement therapy (BHRT) may influence the immune system in a few notable ways. It can dampen cellular immunity by decreasing T-cell activity and reducing the function of natural killer cells - both of which play a key role in protecting the body from infections. Additionally, it may impact innate immune responses, potentially making the body more susceptible to certain infections.
If you're using or thinking about starting BHRT, it's crucial to have an open conversation with a licensed healthcare provider. Regular monitoring and tailored adjustments to your treatment plan can help address these potential immune-related concerns.
How can I keep track of my immune health while using BHRT?
Monitoring your immune system while undergoing bioidentical hormone replacement therapy (BHRT) is a key step in maintaining your overall health. Over time, BHRT can affect immune responses by influencing cytokines, T-cell activity, and inflammation levels, making it important to keep an eye on these changes.
Regular blood tests can help you track important markers like white blood cell counts and cytokine levels, such as IL-6 and TNF-α. Additionally, take note of any frequent infections, unusual fatigue, or changes in your skin, as these could indicate shifts in your immune health. Supporting your immune system through consistent exercise, quality sleep, and a diet rich in nutrients is equally crucial.
With Oana Health, licensed clinicians can assist you in scheduling lab tests, reviewing your results, and adjusting your BHRT plan - all without leaving your home. If you experience recurring infections or receive abnormal lab results, don’t hesitate to connect with your provider for tailored care.
What can I do to reduce the impact of long-term BHRT on my immune system?
Engaging in regular physical activity can help offset the potential immune-suppressing effects associated with long-term bioidentical hormone replacement therapy (BHRT). Research indicates that pairing BHRT with an active lifestyle can enhance immune function by increasing T-cell activity and improving natural killer cell response. To support your immune system, aim for at least 150 minutes of moderate aerobic exercise each week - activities like brisk walking or cycling are great options. Additionally, include two sessions of light resistance training to further strengthen your body’s defenses.
Beyond exercise, maintaining overall wellness plays a key role in supporting immune health. A nutrient-rich diet filled with fruits, vegetables, lean proteins, and healthy fats provides important nutrients like vitamins C and D, as well as zinc - essential components for a strong immune system. Make sleep a priority, aiming for 7–9 hours each night, and incorporate stress-reducing practices such as mindfulness or yoga to help lower chronic inflammation. These combined habits can help your body adapt to hormonal changes while keeping your immune system resilient.
