Magnesium and PCOS: Benefits for Hormonal Health
Magnesium could help manage PCOS symptoms like insulin resistance, hormonal imbalances, and inflammation. Women with PCOS are often magnesium-deficient, which can worsen common issues like irregular periods, acne, and unwanted hair growth. Including magnesium in your routine - through diet or supplements - may improve insulin sensitivity, lower androgen levels, ease stress, and support better sleep.
Key takeaways:
- PCOS and Magnesium Deficiency: 1 in 4 women with PCOS consumes less than the recommended 320 mg of magnesium daily.
- Insulin Resistance: Magnesium helps improve glucose metabolism and reduces insulin resistance, a common PCOS issue.
- Stress and Sleep: Magnesium calms the nervous system, reducing anxiety and improving sleep quality.
- Hormonal Balance: It may help lower testosterone levels, reducing symptoms like hirsutism and acne.
- Best Sources: Magnesium-rich foods (pumpkin seeds, spinach, quinoa) or supplements like magnesium glycinate.
For best results, consult a healthcare provider to determine the right magnesium dosage and form for your needs.
PCOS and Hormonal Imbalances Explained
What Is PCOS and How Does It Affect Hormones?
Polycystic Ovary Syndrome (PCOS) throws off hormonal balance by causing insulin resistance, increased androgen levels, and inflammation. It impacts an estimated 6% to 10% of women of reproductive age worldwide.
Here’s how it works: When insulin sensitivity is impaired, blood sugar levels rise, prompting the body to produce more insulin. This excess insulin signals the ovaries to generate higher levels of androgens (male hormones), leading to symptoms like unwanted facial hair, acne, and hair thinning. Interestingly, magnesium plays a role here by aiding insulin receptor function and supporting glucose transport through GLUT-4, which can help counter some of these effects.
The symptoms of PCOS can vary widely. On the reproductive side, irregular or absent menstrual cycles are common - about 50% of women experience infrequent periods, while 20% face complete absence of menstruation (amenorrhea). Androgenic symptoms such as hirsutism (excess facial and body hair), acne, and hair loss (androgenic alopecia) affect up to 67% of women with PCOS. Additionally, around 70% experience insulin resistance, which can lead to metabolic issues like weight gain around the abdomen and skin conditions such as acanthosis nigricans. Mental health challenges, including anxiety, depression, and sleep disturbances, are also frequently reported.
This hormonal chaos not only drives PCOS symptoms but also increases the body’s demand for magnesium, often leading to a deficiency.
Why Women with PCOS Often Lack Magnesium
Women with PCOS are more likely to experience magnesium deficiency, thanks to a mix of poor dietary habits, insulin resistance, and chronic inflammation. Medications like birth control pills can further deplete magnesium levels, while persistent inflammation raises the body’s need for this essential mineral.
"Lower serum magnesium was associated with aggravated insulin resistance and higher testosterone levels among women with PCOS", explains Xi Luo and colleagues in Frontiers in Endocrinology.
The ripple effects of magnesium deficiency go beyond basic metabolism. Low magnesium levels have been linked to higher fasting glucose levels, more severe insulin resistance (measured by HOMA-IR), and elevated testosterone. Magnesium also influences how testosterone binds to sex hormone-binding globulin (SHBG), which affects the amount of free testosterone circulating in the blood. Common signs of magnesium deficiency in women with PCOS include muscle cramps, frequent migraines, anxiety, intense cravings for chocolate, and painful menstrual cycles.
Magnesium for Insulin Resistance and Metabolism
How Insulin Resistance Affects PCOS
Insulin resistance plays a significant role in PCOS. When your cells stop responding effectively to insulin, blood sugar levels rise. This triggers the pancreas to produce even more insulin, which, in turn, prompts the ovaries to release higher levels of androgens. These hormones are often linked to issues like acne, unwanted facial hair, and weight gain around the midsection. Over time, this creates a cycle where elevated insulin worsens resistance and drives even more androgen production. The result? Weight management becomes tougher, and the risk of developing type 2 diabetes increases. Interestingly, even a small drop in serum magnesium - just 0.1 mmol/L - has been associated with a higher diabetes risk. This highlights how crucial magnesium is for improving insulin sensitivity.
How Magnesium Improves Insulin Sensitivity
Magnesium plays a vital role in easing the metabolic challenges of insulin resistance. It’s essential for activating tyrosine kinase, an enzyme that ensures insulin receptors function properly. Magnesium also helps transport glucose into muscle and fat cells through GLUT-4 proteins. Without enough magnesium, this process falters, making it harder for your body to manage blood sugar.
Research shows that taking 250 mg of magnesium daily can significantly lower serum insulin levels and HOMA-IR scores while improving cholesterol profiles, including LDL and HDL levels.
"Magnesium increases insulin sensitivity through its influence on tyrosine-kinase activity, and its deficiency is associated with IR", states a study published in BMC Nutrition & Metabolism.
How to Take Magnesium for Metabolic Health
Not all magnesium supplements are created equal when it comes to absorption. Magnesium glycinate and magnesium bisglycinate are highly absorbable and gentle on the stomach, making them great for everyday use. Magnesium citrate is another good option but may cause mild laxative effects at higher doses. On the other hand, magnesium oxide, though commonly used due to its affordability, is poorly absorbed and more likely to cause digestive issues like diarrhea.
For metabolic health, studies suggest daily doses between 250 mg and 320 mg. The upper limit for supplemental magnesium is 350 mg per day for women over 14 years old. Going beyond this can lead to side effects like diarrhea, and extremely high doses (3–5 grams) could cause serious problems, including low blood pressure and confusion.
It’s essential to consult a healthcare provider before starting magnesium supplements, especially if you have kidney disease or heart conditions. Since your kidneys are responsible for clearing excess magnesium, any impairment in kidney function can lead to dangerous levels of magnesium in the body. Medical advice is also critical if you’re on medications like birth control pills or diuretics, which can further lower magnesium levels.
Magnesium for Stress, Sleep, and Hormonal Balance
How Stress and Poor Sleep Worsen PCOS
Living with chronic stress and poor sleep can make PCOS symptoms even harder to manage. When stress levels rise, your body releases more cortisol, a hormone that can worsen insulin resistance and disrupt hormonal balance - two key challenges of PCOS. On top of that, lack of sleep throws off your body’s ability to regulate blood sugar and can trigger more inflammation, creating a cycle that’s tough to break.
How Magnesium Calms the Nervous System
Magnesium plays a key role in calming the nervous system. It helps regulate neurotransmitters like GABA (gamma-aminobutyric acid), which is responsible for promoting relaxation and reducing feelings of anxiety. On top of that, magnesium supports enzymes that are involved in controlling blood sugar and stabilizing mood, making it a multitasker when it comes to emotional well-being.
"Magnesium works to calm the excitability of the nervous system to help reduce anxiety. Added bonus: Higher levels of magnesium can also help with sleep, which women with PCOS have difficulty with", explains Angela Grassi, MS, RDN, LDN, from the PCOS Nutrition Center.
Research backs this up. In an 8-week clinical trial, women with PCOS who took 250 mg of magnesium along with 6 mg of melatonin saw significant improvements in their Pittsburgh Sleep Quality Index scores. They also experienced a drop in testosterone levels, from 0.36 ng/mL to 0.27 ng/mL. This suggests that while magnesium alone offers benefits, pairing it with other nutrients like melatonin can amplify its effects on sleep and hormonal balance.
Using Magnesium for Stress and Sleep Support
If you’re looking for magnesium to help with stress and sleep, magnesium glycinate or magnesium bisglycinate are excellent options. These forms are easy for the body to absorb and gentle on the stomach, unlike magnesium oxide, which can sometimes cause digestive discomfort. Taking magnesium in the evening can help your body relax and prepare for restful sleep.
For daily supplementation, a dose between 200 mg and 500 mg is recommended, depending on your specific needs and whether you have a diagnosed deficiency. Some women also enjoy incorporating magnesium-rich, sleep-enhancing drinks into their nightly routines. However, always check with your healthcare provider before starting any new supplement, especially if you’re on medications or have kidney-related health concerns.
Next, we’ll dive into how magnesium can help reduce androgen excess and its related symptoms.
How Magnesium Helps with Hirsutism and Androgen Excess
How Androgens Cause Visible PCOS Symptoms
High androgen levels are a key driver behind some of the most noticeable symptoms of PCOS, including hirsutism (unwanted facial and body hair), scalp hair thinning (androgenic alopecia), and persistent acne. These symptoms can profoundly affect self-esteem and overall quality of life. For instance, up to 67% of women with PCOS experience androgenic alopecia, and more than one-third deal with acne caused by elevated androgen levels. Addressing the hormonal imbalance at the root of these symptoms is crucial for improving both physical and emotional well-being.
How Magnesium Helps Lower Androgens
Magnesium plays an important role in improving insulin sensitivity, which indirectly helps regulate the hormonal imbalances that contribute to symptoms like hirsutism. Since about 70% of women with PCOS have insulin resistance, managing insulin levels is a critical part of controlling androgen production. High insulin levels can stimulate the ovaries to produce more testosterone, worsening symptoms. Magnesium, as a cofactor for the insulin receptor, enhances glucose uptake and reduces the hormonal cascade that leads to excess androgen production.
"Lower serum magnesium was associated with aggravated insulin resistance and higher testosterone levels among women with PCOS", according to research published in Frontiers in Endocrinology.
Interestingly, studies have found that higher magnesium levels in the blood are linked to lower testosterone levels. Magnesium may also influence how testosterone interacts with Sex Hormone-Binding Globulin (SHBG), which determines how much active testosterone is available in the body.
However, clinical trials using low-dose magnesium oxide (250 mg) on its own have shown mixed results in directly reducing testosterone levels or improving hirsutism scores. On the other hand, when magnesium is combined with nutrients like Vitamin E or Zinc, the results have been more promising. These combinations have shown better outcomes in managing hormonal levels and reducing visible symptoms. This suggests that magnesium works best as part of a broader, multi-faceted treatment plan rather than as a standalone solution.
Combining Magnesium with Prescription Treatments
While magnesium provides essential metabolic support, pairing it with prescription treatments can help tackle androgen-related symptoms more directly. For example, spironolactone, available through Oana Health, blocks androgen receptors to reduce acne and unwanted hair growth. For those experiencing scalp hair loss, options like oral minoxidil or topical spironolactone may promote regrowth.
Combining these treatments with 200–500 mg of magnesium glycinate or bisglycinate daily can address both the visible symptoms and the underlying metabolic factors. However, it’s essential to consult your healthcare provider before starting any new supplement, especially if you’re already on prescription medications.
sbb-itb-6dba428
4 Health Benefits of Magnesium for PCOS Explain by Dr.Sneha Shetty
Adding Magnesium to Your PCOS Treatment Plan
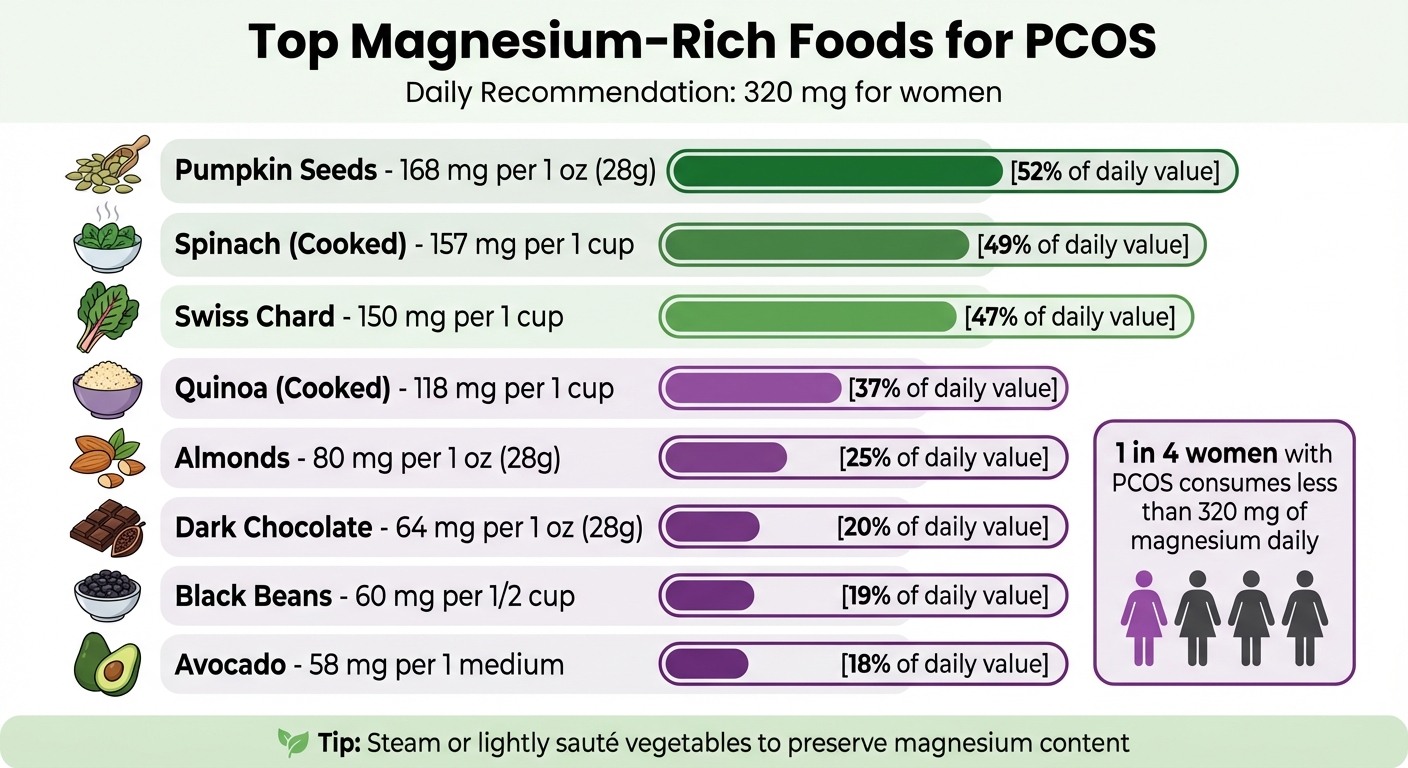
Magnesium-Rich Foods for PCOS: Top Sources and Daily Content
Foods High in Magnesium
Including magnesium-rich foods in your diet can help you meet your daily needs. For instance, pumpkin seeds pack a punch with 168 mg of magnesium per ounce - more than half the daily recommendation for women. Cooked spinach provides 157 mg per cup, and Swiss chard comes in at 150 mg per cup. Other great sources include quinoa (118 mg per cooked cup), almonds (80 mg per ounce), dark chocolate (64 mg per ounce), black beans (60 mg per half cup), and avocado (58 mg per medium fruit).
Here are some simple ways to incorporate these foods into your meals:
- Toss spinach or kale into your morning omelet or smoothie.
- Snack on almonds, cashews, or pumpkin seeds during the day.
- Replace white rice or refined pasta with quinoa or brown rice at dinner.
- Add black beans, edamame, or lentils to your meals once or twice a week.
- Treat yourself to dark chocolate paired with nuts for a magnesium boost.
Many individuals with PCOS struggle to meet the recommended daily intake of 320 mg, which increases the risk of deficiency. Contributing factors include poor soil quality, chronic stress that depletes magnesium, and higher magnesium demands due to inflammation. To preserve magnesium content in vegetables, opt for steaming or light sautéing.
| Food Item | Serving Size | Magnesium Content (mg) |
|---|---|---|
| Pumpkin Seeds | 1 oz (28g) | 168 mg |
| Spinach (Cooked) | 1 cup | 157 mg |
| Swiss Chard | 1 cup | 150 mg |
| Quinoa (Cooked) | 1 cup | 118 mg |
| Almonds | 1 oz (28g) | 80 mg |
| Dark Chocolate | 1 oz (28g) | 64 mg |
| Black Beans | 1/2 cup | 60 mg |
| Avocado | 1 medium | 58 mg |
If dietary sources aren’t enough, magnesium supplements can help fill the gap.
Magnesium Supplement Safety and Dosing
When food alone doesn’t provide enough magnesium, supplements can be a helpful addition. For women with PCOS, doses typically range from 200 mg to 350 mg daily, with clinical studies often using 250 mg per day for 8–12 weeks to improve metabolic health. The upper limit for supplemental magnesium is 350 mg per day to minimize side effects like diarrhea.
Magnesium glycinate (or bisglycinate) is often recommended for PCOS due to its high absorption rate and gentle effect on digestion. Magnesium citrate is another effective option, though it may cause some digestive discomfort for certain individuals. Forms like magnesium oxide or sulfate are less ideal, as they are poorly absorbed and more likely to act as laxatives.
If you have heart block or kidney disease, avoid magnesium supplements without consulting a healthcare provider. Additionally, some medications - such as birth control pills, diuretics, and proton pump inhibitors (PPIs) - can interfere with magnesium absorption or increase its excretion. If you’re taking medications like Metformin for insulin resistance or Spironolactone for androgen-related issues, speak with your doctor before adding magnesium to your routine. Taking supplements with meals can improve tolerance and absorption.
How Oana Health Personalizes PCOS Care
Oana Health offers tailored PCOS treatment plans that integrate magnesium supplementation with FDA-approved therapies designed to address your specific symptoms. For example:
- If insulin resistance is a concern, your provider might pair magnesium with Metformin to support better glucose regulation.
- For acne or unwanted facial hair, Spironolactone may be recommended to block androgen receptors while magnesium aids overall metabolic balance.
- For hair loss, options like oral minoxidil or topical spironolactone can be combined with magnesium to encourage hair regrowth.
Oana Health’s licensed medical professionals take a comprehensive look at your health history, medications, and risk factors for magnesium deficiency - such as the use of birth control pills - to determine the best magnesium type and dose for you. Since magnesium plays a role in over 300 enzyme systems that regulate blood sugar and insulin signaling, their recommendations are customized to your unique metabolic needs and PCOS profile. Plus, all treatments are conveniently delivered to your door with free shipping, making it easier to stay on track with your personalized care plan.
Conclusion: Magnesium as Part of a Complete PCOS Care Plan
Magnesium plays a key role in managing PCOS by improving insulin sensitivity, lowering androgen levels, and supporting a healthier stress response. It’s involved in crucial enzymatic processes that aid glucose metabolism and help calm the nervous system, which can reduce stress and promote better sleep quality. Women with PCOS are also at a significantly higher risk of magnesium deficiency.
The benefits of magnesium are most effective when combined with other nutrients and tailored treatments. Research suggests that pairing magnesium with nutrients like Vitamin E or Zinc can further enhance results, particularly for managing glucose metabolism and reducing inflammation. This synergistic approach builds on the metabolic and hormonal improvements discussed earlier, addressing insulin resistance and androgen-related symptoms in a more comprehensive way.
Incorporating magnesium into a broader treatment plan, including prescription therapies, can take PCOS management to the next level. For example, Oana Health offers a personalized approach, combining magnesium recommendations with customized prescription treatments. Their licensed professionals design care plans that fit your specific needs, whether you’re managing insulin resistance, tackling hair growth concerns, or supporting hair regrowth. Plus, treatments are delivered directly to your door with free shipping, making it easier to stay on track with your care.
"Magnesium supplementation in women with PCOS had a significant positive effect on improving total quality of life and its components." - Reproductive Biology and Endocrinology
This integrated approach not only helps manage symptoms but also promotes long-term hormonal balance and a better quality of life for women living with PCOS.
FAQs
How does magnesium help improve insulin resistance in women with PCOS?
Magnesium plays an important role in addressing insulin resistance, a frequent issue for women with PCOS. It works as a co-factor in insulin signaling pathways, enabling your cells to more efficiently absorb glucose from the bloodstream. This can help lower fasting blood sugar levels and enhance insulin sensitivity, making it easier to manage symptoms like weight gain and fatigue.
By promoting stable blood sugar levels, magnesium may also help reduce the risk of long-term health issues linked to insulin resistance, such as type 2 diabetes. Adding magnesium-rich foods or supplements to your routine can be a straightforward way to support better hormonal balance and overall well-being.
What type of magnesium supplement is best for managing PCOS symptoms?
Magnesium plays an important role in managing common PCOS symptoms, such as insulin resistance, hormonal imbalances, and stress. Studies have found that magnesium can help improve glucose regulation and lower oxidative stress - two factors that are particularly beneficial for women dealing with PCOS.
When it comes to choosing a magnesium supplement, there isn’t a one-size-fits-all solution. However, forms like magnesium citrate and magnesium glycinate are often recommended because they’re easier for the body to absorb. The best option for you will depend on factors like your body’s absorption ability and any other health conditions you might have.
For tailored advice, Oana Health’s telehealth clinicians can evaluate your specific hormonal and metabolic needs. They’ll recommend the most appropriate magnesium supplement for you and ensure it’s conveniently delivered to your home with free shipping.
Can magnesium help reduce androgen levels and ease PCOS symptoms?
Magnesium is known for its health benefits, but current studies indicate it doesn’t directly reduce androgen levels or significantly alleviate symptoms like excess facial or body hair (hirsutism) in individuals with PCOS. That said, magnesium can still play a role in supporting overall hormonal balance by aiding with insulin resistance, stress management, and improving sleep quality - common hurdles for those managing PCOS.
For a well-rounded approach to PCOS management, it’s important to focus on treatments that tackle various aspects, including hormonal imbalances, weight regulation, and mental health. Always consult a healthcare professional to develop a plan tailored to your needs.
