MBSR for PCOS: What Studies Show
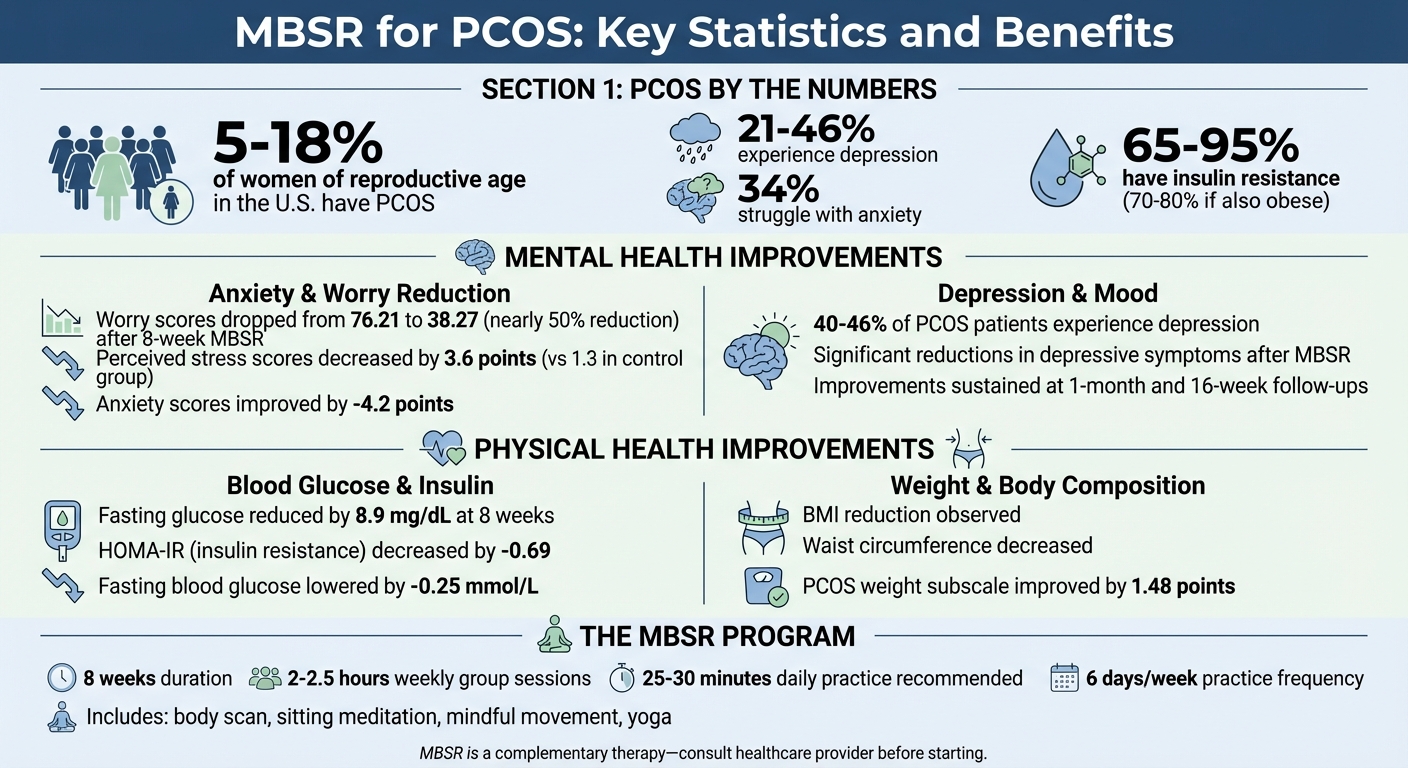
Mindfulness-Based Stress Reduction (MBSR) is gaining attention as a supportive approach for managing Polycystic Ovary Syndrome (PCOS). PCOS affects 5%–18% of women of reproductive age in the U.S., causing hormonal imbalances, irregular cycles, and symptoms like acne, weight gain, and excess hair growth. But the mental health impact is equally concerning, with 21%–46% of women experiencing depression and 34% struggling with anxiety. Stress worsens these symptoms by increasing cortisol, insulin resistance, and inflammation, creating a harmful cycle.
Here's how MBSR helps:
- Mental Health: Studies show reduced anxiety, depression, and stress. For example, a 2021 study in Iran found worry scores dropped by nearly 50% after an 8-week MBSR program.
- Physical Health: MBSR lowers cortisol, improves insulin sensitivity, and supports weight management. A Penn State study reported a reduction in fasting glucose levels and stress in participants.
- Lifestyle Impact: MBSR promotes mindfulness through meditation, yoga, and daily practices, helping participants manage emotional eating and adopt healthier habits.
While MBSR isn't a standalone solution, it complements traditional treatments by addressing PCOS's emotional and physical challenges. Research suggests consistent mindfulness practice (25–30 minutes daily) can make a real difference. However, more studies with diverse participants and longer follow-ups are needed to confirm its long-term effects.
If you're managing PCOS, integrating mindfulness into your routine might improve both emotional well-being and hormonal balance. Talk to your healthcare provider about whether MBSR could fit into your care plan.
MBSR Benefits for PCOS: Mental and Physical Health Outcomes
How Stress Affects PCOS and What MBSR Does
The Stress-Hormone Connection in PCOS
Stress and PCOS are closely linked through the body's hormonal responses. Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system, leading to the release of cortisol. This stress hormone can worsen PCOS symptoms in several ways. For instance, elevated cortisol increases blood sugar levels, which aggravates insulin resistance - a key issue for 75% to 95% of individuals with PCOS. It also disrupts the communication between the brain and ovaries, interfering with ovulation and menstrual cycles. Androgen-related symptoms, such as excess hair growth or acne, may also become more pronounced as a result of this hormonal imbalance.
A meta-analysis of 41 studies highlights that women with PCOS generally have higher cortisol levels compared to those without the condition.
"At its core, PCOS is about hormone imbalance, and stress could make that imbalance worse." – Novomins Nutrition
Beyond hormonal disruptions, high cortisol levels contribute to low-grade inflammation and encourage visceral fat storage, particularly around the abdomen. Additionally, research shows a significant correlation between perceived stress and prolactin levels in women with PCOS (r = 0.450; p = 0.011), suggesting that prolactin could act as a marker for chronic stress in this group. These findings underscore the importance of stress management, paving the way for mindfulness-based approaches to help restore hormonal balance.
What MBSR Programs Include
Mindfulness-Based Stress Reduction (MBSR) programs offer a structured approach to breaking the cycle of stress. Typically lasting eight weeks, these programs involve weekly group sessions of about 2 to 2.5 hours, along with a full-day silent retreat. The core practices include body scan exercises to observe physical sensations without judgment, sitting meditation focused on the breath, and mindful movement through gentle yoga and walking.
Participants are encouraged to integrate mindfulness into their daily lives. This might involve practices like mindful eating or bringing awareness to routine activities. The programs also include stress education, helping participants recognize automatic stress reactions and replace them with more intentional, thoughtful responses. Research indicates that dedicating 25 to 30 minutes daily, six days a week, to these mindfulness techniques can lead to reduced stress levels and better glucose control.
Mental Health Benefits: What Studies Show
Lower Anxiety and Stress Levels
Studies reveal that Mindfulness-Based Stress Reduction (MBSR) can significantly reduce anxiety and stress in women with PCOS. For example, a study conducted at Kerman University tracked 60 women with PCOS and found that their worry scores dropped from 76.21 to 38.27 just one month after completing MBSR. Meanwhile, the control group’s scores remained nearly unchanged at 76.13. The same research highlighted improvements across six key areas linked to PCOS: mental health challenges, interpersonal issues, physical symptoms unrelated to pregnancy, pregnancy complications, sexual health, and religious concerns.
Another randomized trial led by Dr. Nazia Raja-Khan at Penn State College of Medicine between 2011 and 2013 focused on 86 women with a BMI of 25 or higher. Participants in the MBSR group attended eight weekly 2.5-hour sessions, plus a 6-hour retreat. By the 16-week follow-up, their perceived stress scores dropped by 3.6 points, compared to just a 1.3-point reduction in the control group. Anxiety scores in the MBSR group also improved, with a mean change of –4.2.
"In women with overweight or obesity, MBSR significantly reduces stress and may have beneficial effects on glucose." – Dr. Nazia Raja-Khan, Division of Endocrinology, Diabetes, and Metabolism, Penn State College of Medicine
What sets MBSR apart is its ability to disrupt repetitive negative thinking patterns - often referred to as perseverative cognition - that keep stress levels high. By fostering a more intentional response to PCOS-related stressors, MBSR helps reduce anxiety and creates space for better emotional health .
Better Mood and Depression Outcomes
Depression is a common struggle for women with PCOS, affecting 40%–46% of patients, with lifetime rates reaching as high as 67% . MBSR has been shown to ease this burden by promoting lasting improvements in mood and emotional well-being.
In March 2023, a study at the University Medical Centre Ljubljana in Slovenia evaluated 42 women with PCOS and high metabolic risk. After completing an 8-week MBSR program, participants experienced significant reductions in depressive symptoms, along with better emotional well-being and general health perceptions. The program also helped participants develop greater attention, awareness, and self-regulation, which are essential for managing emotional challenges.
MBSR doesn’t just reduce negative emotions - it also boosts optimism and self-esteem while addressing body image concerns, which are frequent contributors to depression in PCOS patients. Participants reported feeling less constrained by emotional difficulties in their daily lives, a benefit researchers describe as reduced "emotional role limitation".
"MBSR may be a useful supplementary therapy to mitigate the deleterious effects of PCOS on mental health." – Hana Dema et al., University Medical Centre Ljubljana
Perhaps most encouraging is the lasting nature of these benefits. Studies show that improvements in mood and worry levels remain evident even at one-month and 16-week follow-ups .
Physical Health Changes Linked to MBSR
Mindfulness-Based Stress Reduction (MBSR) doesn't just help with mood and anxiety - it also impacts several physical health aspects of PCOS.
Effects on Insulin Resistance
Insulin resistance is a common challenge for women with PCOS, affecting 65% to 70% of them, with the rate climbing to 70–80% in those who are also obese. MBSR may help address this issue by lowering cortisol levels, which can reduce sugar release from the liver and stabilize blood glucose levels.
From 2011 to 2013, Dr. Nazia Raja‐Khan at Penn State Hershey Medical Center conducted a randomized controlled trial involving 86 women (31 of whom had PCOS) with a BMI of 25 kg/m² or higher. Participants who completed an 8-week MBSR program experienced a drop in fasting glucose levels - down by 8.9 mg/dL at the 8-week mark and 9.3 mg/dL at a 16-week follow-up. The control group, on the other hand, showed no significant changes.
"In women with overweight or obesity, MBSR significantly reduces stress and may have beneficial effects on glucose." – Dr. Nazia Raja‐Khan, Division of Endocrinology, Diabetes, and Metabolism, Penn State College of Medicine
A 2024 meta-analysis reviewing 12 randomized controlled trials found that mind-body interventions, including MBSR, improved insulin sensitivity with a mean HOMA-IR reduction of –0.69 and lowered fasting blood glucose by –0.25 mmol/L. While MBSR seems to improve how cells respond to insulin, it doesn't necessarily reduce overall insulin production. Interestingly, mindfulness may even influence DNA methylation in genes tied to insulin signaling.
Effects on Weight Management
MBSR has also been shown to support weight-related improvements in people with PCOS. A 2024 meta-analysis noted that mind-body interventions boosted the weight subscale of the PCOS Questionnaire by 1.48 points and slightly reduced the waist-hip ratio by 0.02.
In a 2023 study led by Hana Dema and Jurij Bon at the University Medical Centre Ljubljana, 42 women with PCOS and high metabolic risk participated in an 8-week MBSR program. This included weekly two-hour group sessions and one individual meeting. The results? Participants saw reductions in BMI, waist circumference, and blood glucose levels, alongside improvements in overall health.
"MBSR was associated with a reduction in body mass index, waist circumference and blood glucose level, an improvement in subjectively perceived general health... and levels of pain." – Hana Dema et al., Department of Health Care Quality, University Medical Centre Ljubljana
The success of MBSR in this area seems to come from its ability to boost self-efficacy around diet and exercise - key strategies for managing PCOS. By promoting mindful responses to stress, it helps curb emotional eating and encourages healthier lifestyle habits. While some studies report mixed outcomes for overall weight loss, consistent improvements in waist circumference, body composition, and body image highlight MBSR's potential as a supportive tool alongside traditional PCOS treatments.
sbb-itb-6dba428
Research Gaps and What's Needed Next
Current studies on MBSR (Mindfulness-Based Stress Reduction) and PCOS (Polycystic Ovary Syndrome) offer encouraging insights, but there are still many unanswered questions about how this approach works across different groups and over extended periods.
Study Limitations
Several limitations in existing research make it difficult to draw broad conclusions. For instance, studies often involve small sample sizes, typically ranging from 42 to 60 participants, which limits how applicable the findings are to larger populations. Additionally, short follow-up periods - spanning only 1 month to 16 weeks - make it hard to determine whether the benefits of MBSR last over time.
Demographic bias is another issue. Most studies focus on married women, leaving single women underrepresented. Furthermore, women with severe psychiatric conditions or those taking medications like metformin are frequently excluded, which narrows the scope of the findings. Baseline differences, such as variations in age or metabolic markers like triglycerides, can also skew results and make comparisons less reliable.
These challenges highlight the need for more robust and inclusive research designs.
Future Research Directions
To make MBSR a more effective complementary treatment for PCOS, future studies need to address these gaps. Including adolescents in research is particularly important. The "PCOS Kind Mind Program", conducted in Central Texas in 2021, demonstrated improvements in nutrition self-efficacy and physical activity among participants aged 14–23.
"These findings are encouraging and suggest the need for larger-scale, randomized controlled trials with longer-term follow-up to more robustly evaluate the effects of the PCOS Kind Mind Program on the psychological and physiological health of adolescents and young people with PCOS." – PCOS Kind Mind Program Study
Another promising area for future research is exploring whether MBSR leads to long-term epigenetic changes in insulin signaling and stress response pathways. Understanding these mechanisms could provide deeper insights into how MBSR impacts PCOS over time.
Researchers should also aim to recruit more diverse populations to ensure findings are widely applicable. Standardized guidelines for study design and evaluation would help improve the consistency and reliability of results. Additionally, assessing the cost-effectiveness of MBSR could make it a more accessible option for those managing PCOS.
As Saeeda Khan from the Faculty of Nursing and Midwifery at Ziauddin University emphasized:
"The analysis suggests that there is an urgent need for significant advancements in PCOS research concerning mental health assessment and therapies".
Conclusion
Research highlights that Mindfulness-Based Stress Reduction (MBSR) can provide measurable benefits for women managing PCOS, addressing both mental and physical challenges that conventional treatments may not fully resolve. Studies have shown notable decreases in anxiety, depression, and PCOS-related worries. These emotional improvements are accompanied by physical changes, including lower fasting blood glucose levels, better insulin sensitivity, and reductions in BMI and waist circumference. These results emphasize the potential of incorporating MBSR into broader PCOS management strategies.
What sets MBSR apart is its non-drug approach, which helps alleviate the psychological strain of living with PCOS. Hana Dema from the University Medical Centre Ljubljana explains:
"MBSR may be a useful supplementary therapy to mitigate the deleterious effects of PCOS on mental health".
Additionally, early research suggests that MBSR might even influence stress response and metabolism at the genetic level, hinting at possible long-term benefits.
Incorporating mindfulness practices into your PCOS care routine could bring real improvements to both hormonal and emotional health. Participants in these studies practiced mindfulness for 25 to 30 minutes a day, six days a week, to achieve these outcomes. This makes it a practical addition to medications, lifestyle adjustments, and other treatments.
While mindfulness isn’t a substitute for standard medical care, it can address the emotional challenges that often accompany PCOS. Evidence also points to benefits like improved quality of life, better emotional health, and more regular menstrual cycles. For a well-rounded, evidence-based approach to managing PCOS - including support for hormonal balance, mental health, and weight management - consider speaking with a trusted healthcare provider, such as Oana Health, about integrating mindfulness into your treatment plan.
FAQs
How can Mindfulness-Based Stress Reduction (MBSR) help with PCOS symptoms?
Mindfulness-Based Stress Reduction (MBSR) can be a powerful tool for managing PCOS by tackling the effects of chronic stress on hormones, metabolism, and emotional health. Research shows that MBSR helps lower stress, anxiety, and depressive symptoms - challenges that many individuals with PCOS face. Participants in MBSR programs often report feeling emotionally healthier, experiencing less psychological distress, and enjoying an improved quality of life.
The benefits aren't just emotional; they extend to physical health too. Studies reveal that MBSR is associated with reductions in body mass index (BMI), waist circumference, and fasting blood sugar levels. It’s also been linked to lower levels of stress hormones like cortisol and may even support insulin signaling and hormonal balance through epigenetic changes.
By incorporating MBSR into a PCOS care plan, individuals can address both the emotional and physical symptoms of the condition. Oana Health offers tailored, science-based telehealth programs that combine mindfulness techniques with medical treatments, making it easier to manage PCOS effectively from the comfort of home.
Can mindfulness-based stress reduction (MBSR) be used with traditional PCOS treatments?
Yes, mindfulness-based stress reduction (MBSR) can work hand-in-hand with traditional PCOS treatments, such as hormonal contraceptives, metformin, anti-androgens, or weight-loss programs. Research suggests that MBSR may boost emotional well-being, lower stress levels, and even help with clinical symptoms - all without interfering with standard medications.
For instance, one study found that an eight-week mindfulness program helped women with PCOS and high metabolic risk see improvements in their symptoms. Other trials have reported noticeable reductions in anxiety and stress after MBSR sessions. These positive effects were observed while participants continued their usual treatments, making MBSR a valuable addition to their care plans.
Because MBSR emphasizes stress management, emotional balance, and mindful eating, it doesn’t interfere with medications. Patients using Oana Health’s telehealth services can discuss with their clinicians how MBSR might complement their PCOS treatment plan, addressing issues like insulin resistance, weight management, acne, and mental health.
What are the challenges in studying MBSR for PCOS?
Research into mindfulness-based stress reduction (MBSR) for managing polycystic ovary syndrome (PCOS) is still in its early stages and faces several hurdles. Many studies have been conducted with small participant groups and tend to focus on short-term outcomes. This makes it challenging to determine whether MBSR provides lasting benefits for hormonal and metabolic health. Adding to the complexity, differences in study designs, intervention methods, and measurement tools make it hard to compare results and apply findings broadly.
A common issue is the reliance on self-reported outcomes, such as anxiety levels or overall quality of life, while fewer studies investigate measurable markers like hormone levels or insulin resistance. To fully understand the potential of MBSR for PCOS, larger studies with diverse participants, standardized methods, and longer follow-up periods are essential.
Even with these limitations, MBSR has shown potential in helping women improve emotional well-being and manage stress - key factors in PCOS care. For those looking for tailored, evidence-based support for PCOS, Oana Health provides telehealth programs crafted by licensed medical professionals, addressing hormonal balance, weight management, and mental health.
