PCOS and Endometrial Hyperplasia Risk
Polycystic Ovary Syndrome (PCOS) increases the risk of endometrial hyperplasia, a condition where the uterine lining thickens abnormally. This happens due to hormonal imbalances caused by PCOS, particularly chronic anovulation, which leads to insufficient progesterone and unchecked estrogen exposure. Without treatment, severe forms of hyperplasia may progress to endometrial cancer, with nearly 30% of cases advancing to malignancy if left untreated.
Key Points:
- PCOS and Risk: Women with PCOS are 2-6 times more likely to develop endometrial cancer.
- Contributing Factors: Chronic anovulation, insulin resistance (affecting 70% of PCOS patients), and obesity amplify the risk.
- Symptoms to Watch: Abnormal uterine bleeding, heavy periods, or prolonged gaps between cycles.
- Treatment Options:
- Hormonal therapies like progestins or contraceptives to regulate cycles.
- Weight management through diet, exercise, and medications like Metformin or GLP-1 receptor agonists.
- Regular monitoring with ultrasounds and biopsies if hyperplasia is suspected.
- Prevention: Early diagnosis, lifestyle changes, and consistent follow-ups are critical to reducing risks.
PCOS-related hormonal and metabolic imbalances require careful management to prevent complications. Addressing symptoms early, maintaining a healthy weight, and regular medical check-ups are essential steps for long-term health.
Mayo Clinic Minute - Endometrial cancer associated with PCOS
What Is Endometrial Hyperplasia and Why PCOS Patients Are at Risk
Types of Endometrial Hyperplasia: Risk Levels and Treatment Options
Endometrial hyperplasia occurs when the uterine lining builds up excessively due to prolonged exposure to estrogen without the balancing effect of progesterone. This imbalance prevents the regular shedding of the uterine lining, leading to its continuous thickening.
This condition is considered a direct precursor to endometrioid adenocarcinoma, the most common form of uterine cancer in the U.S. In fact, in 2023 alone, approximately 66,200 cases of endometrial cancer were diagnosed.
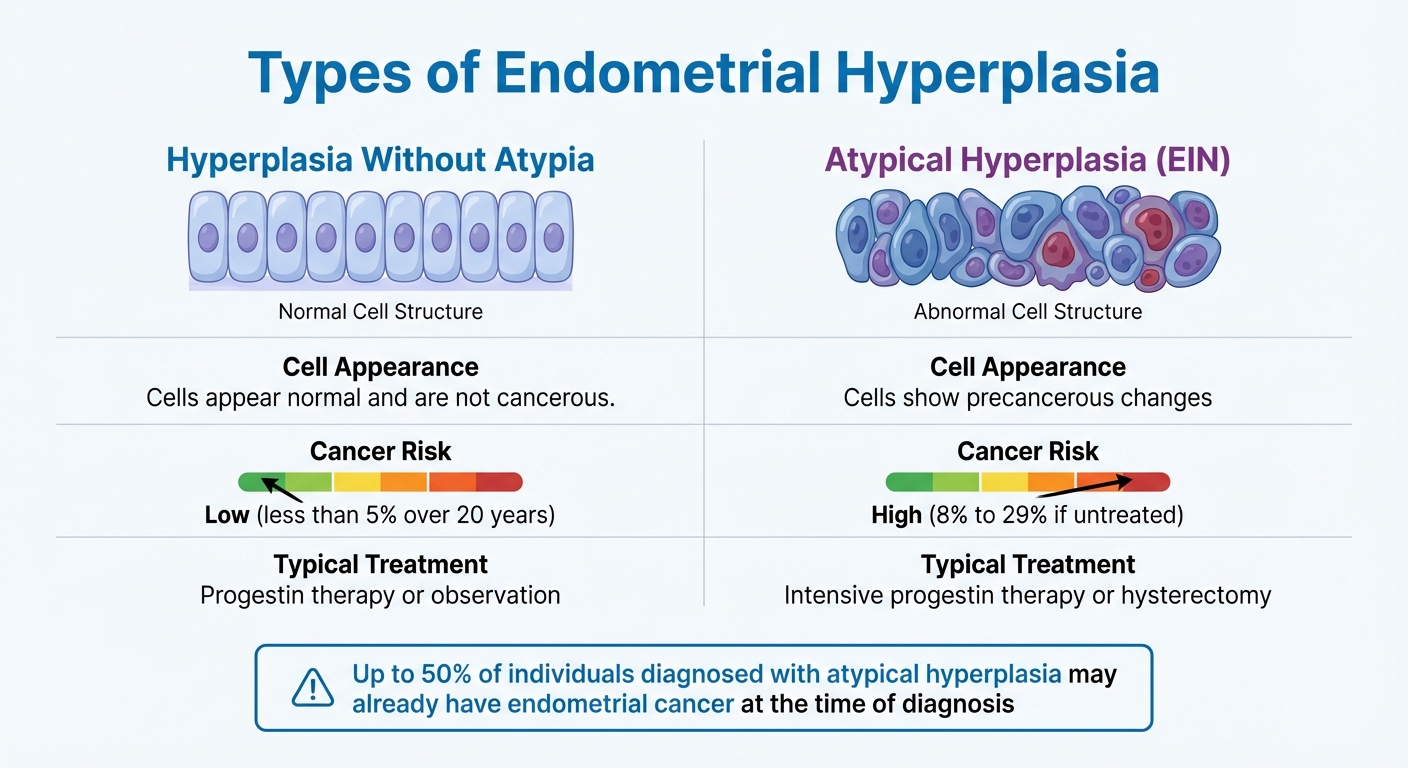
Types of Endometrial Hyperplasia
Endometrial hyperplasia is categorized into two main types based on how the cells look under a microscope:
| Type | Cell Appearance | Cancer Risk | Typical Treatment |
|---|---|---|---|
| Hyperplasia Without Atypia | Cells appear normal and are not cancerous | Low (less than 5% over 20 years) | Progestin therapy or observation |
| Atypical Hyperplasia (EIN) | Cells show precancerous changes | High (8% to 29% if untreated) | Intensive progestin therapy or hysterectomy |
This classification is crucial because the risks and treatment options differ significantly. Non-atypical hyperplasia often resolves with appropriate treatment, but atypical hyperplasia is more serious. Research shows that up to 50% of individuals diagnosed with atypical hyperplasia may already have endometrial cancer at the time of diagnosis.
Understanding these distinctions is key to recognizing how hormonal imbalances linked to PCOS can amplify the risk.
How PCOS Increases Your Risk
Women with PCOS are at a significantly higher risk - 2 to 6 times more likely - of developing endometrial cancer compared to women without the condition. This heightened risk is driven by several interconnected factors:
- Chronic anovulation: Many women with PCOS experience irregular ovulation or fail to ovulate entirely. This results in insufficient progesterone production, leaving about 41% of PCOS patients vulnerable to hyperplasia due to constant estrogen exposure.
- Insulin resistance: Around 70% of women with PCOS also have insulin resistance. This condition lowers levels of Sex Hormone-Binding Globulin (SHBG), which increases the amount of free, active estrogen circulating in the body.
- Obesity: Excess fat tissue further raises estrogen levels by converting androgens into estrogen through the enzyme aromatase.
"The longer someone goes without shedding the lining of the uterus (or having a period), in the setting of chronic estrogen exposure, the greater their risk for endometrial hyperplasia and endometrial cancer." – Harvard T.H. Chan School of Public Health
These risk factors highlight the importance of recognizing warning signs, particularly abnormal uterine bleeding. Symptoms may include unusually heavy periods, bleeding between cycles, or menstrual cycles shorter than 21 days. Additionally, chronic heavy bleeding can lead to iron-deficiency anemia, which often causes persistent fatigue. Monitoring these symptoms is essential for early detection and management.
Risk Factors and Warning Signs to Watch For
Knowing your risk profile can help with early detection. While PCOS is a key factor, other risks can also increase the likelihood of developing hyperplasia.
Hormonal and Reproductive Risk Factors
If you experience prolonged anovulation - having fewer than eight periods a year - it means your uterine lining doesn’t shed regularly. This allows it to thicken due to constant exposure to estrogen without the balancing effect of progesterone, which can lead to endometrial hyperplasia.
Certain reproductive factors also play a role. For instance, starting your period before age 12 (early menarche) increases your lifetime exposure to estrogen. Similarly, nulliparity - never having been pregnant - raises the risk because pregnancy interrupts estrogen exposure. In fact, women who have given birth have a 35% lower risk of developing endometrial cancer compared to those who haven’t. Additionally, infertility might signal underlying hormonal imbalances that make the uterine lining more vulnerable.
Metabolic factors, often linked to PCOS, can amplify these risks even further.
Metabolic and Lifestyle Risk Factors
Metabolic issues tied to PCOS significantly influence hyperplasia risk. Obesity, for example, not only disrupts hormonal balance but also increases estrogen production. This happens because fat tissue converts androgens into estrone, a type of estrogen. Research shows that for every 5 kg/m² increase in BMI, the risk of endometrial cancer rises 1.5 times.
Insulin resistance, which affects approximately 70% of women with PCOS, also contributes. It can directly encourage endometrial growth while reducing levels of sex hormone-binding globulin (SHBG). When insulin resistance progresses to Type 2 diabetes, the risk becomes even higher. Considering that 38% to 88% of women with PCOS are overweight or obese, managing weight is a critical step. Even losing as little as 5% of body weight can help restore regular ovulation and improve overall metabolic health.
Symptoms That Require Medical Attention
Imbalances in hormones and metabolism often show up as noticeable symptoms. Some of these symptoms should prompt you to seek medical advice, as they may signal the onset of hyperplasia. The most common warning sign is abnormal uterine bleeding. This includes periods that are unusually heavy or last longer than normal, bleeding between cycles, or cycles shorter than 21 days. On the other hand, going for long stretches without a period can also be concerning, as it allows the uterine lining to thicken unchecked.
Other symptoms, like fatigue and pallor, could point to anemia caused by chronic heavy bleeding. Keeping track of your menstrual cycles is essential - if you have fewer than eight periods a year or your cycle length falls outside the 21- to 35-day range, it’s time to consult a healthcare professional.
sbb-itb-6dba428
Treatment Options to Lower Your Risk
Treatment focuses on restoring hormonal balance and addressing metabolic concerns to safeguard the uterine lining.
Hormone Therapy to Regulate Your Cycle
Hormone therapy is key to preventing unopposed estrogen exposure, which is the primary cause of endometrial thickening in PCOS. The go-to treatment for menstrual irregularities related to PCOS is combined hormonal contraceptives (COCs). These are available as pills, patches, or rings and work by supplying regular progesterone to counteract estrogen's effects on the uterine lining. Studies show that using oral contraceptives for five years can reduce the relative risk of endometrial issues by 24%.
For those who cannot tolerate or have contraindications to COCs - such as smokers over 35, individuals with high blood pressure, or those with a history of blood clots - alternative options are available. One effective choice is a progestin-releasing IUD (like the 52-mg levonorgestrel device), which offers reliable contraception while significantly lowering the risk of endometrial hyperplasia.
"Progestin IUDs will not help hyperandrogenism but are highly effective at preventing hyperplasia and providing safe, highly effective contraception"
Another option is cyclic progestins, which help regulate your cycle by ensuring the uterine lining is shed regularly. However, these do not provide contraception or address symptoms related to androgen excess.
Managing Insulin Resistance and Weight
Addressing insulin resistance plays a crucial role in reducing the risk of hyperplasia. Even modest weight loss - just 5% to 10% of your body weight - can restore normal ovulatory cycles and improve fertility outcomes. A combination of a calorie-restricted diet and regular exercise is a good starting point.
For medication support, metformin is a well-researched option that enhances insulin sensitivity and helps restore ovulatory cycles in 30% to 50% of PCOS patients. It’s often recommended as a second-line treatment for menstrual irregularities when hormonal contraceptives are not an option. Additionally, GLP-1 receptor agonists (such as liraglutide or semaglutide), either on their own or combined with metformin, can promote weight loss while improving glucose and androgen levels.
For those interested in personalized care, Oana Health provides telehealth options for these medications. Their offerings include oral GLP-1 & Metformin starting at $199/month and oral Metformin ER at $22/month, with prescriptions handled by licensed professionals and delivered to your home with free shipping.
Treatment for Diagnosed Hyperplasia
If endometrial hyperplasia is diagnosed, treatment will depend on whether it is atypical or non-atypical. For non-atypical hyperplasia, continuous progestin therapy is typically effective, as restoring progesterone levels often reverses hyperplastic changes. Research suggests that a levonorgestrel IUD produces higher regression rates than oral progestins alone, and combining the two may lead to regression rates of up to 85%.
For atypical hyperplasia (also known as endometrial intraepithelial neoplasia), the stakes are higher due to an 8% annual risk of progression to cancer. In such cases, a hysterectomy is the definitive treatment. However, for those prioritizing fertility or unable to undergo surgery, high-dose progestin therapy is the standard alternative. Patients undergoing conservative treatments are typically advised to have repeat endometrial biopsies every 3 to 6 months to monitor their progress.
The American College of Obstetricians and Gynecologists also emphasizes the importance of lifestyle changes, particularly weight loss and improved blood sugar control, to enhance overall health and potentially reduce the risks of EIN–AEH and endometrial cancer.
These approaches underscore the importance of consistent monitoring and follow-up care to ensure long-term health.
Monitoring and Follow-Up Care
Once initial treatment strategies are in place, regular monitoring becomes key to preventing the progression of endometrial hyperplasia into something more severe. This condition serves as a warning sign for endometrial cancer, which is the most common gynecologic cancer in developed countries. For women with PCOS, the risk of endometrial cancer is three times higher than average.
Regular Screening and Check-Ups
Keeping track of your menstrual cycle is a simple yet crucial step. Use a calendar or an app to monitor your periods. If you notice fewer than 6 to 8 periods per year or cycles lasting longer than 35 days, it’s time to consult your doctor.
Metabolic health is another area to watch closely. Scheduling an oral glucose tolerance test (OGTT) every 3 to 5 years helps check for impaired glucose tolerance or Type 2 Diabetes, both of which can increase your risk of hyperplasia. Additionally, monitoring your BMI and waist circumference during regular check-ups can flag early metabolic risks. If you notice weight gain or increased abdominal fat, it may be necessary to schedule more frequent tests.
| Monitoring Tool | Purpose | Recommended Frequency |
|---|---|---|
| Menstrual History | Identify irregular shedding and anovulation | Every clinical visit |
| OGTT (75-g glucose load) | Screen for diabetes and insulin resistance | Every 3–5 years (or more often if needed) |
| BMI & Waist Circumference | Assess metabolic risk factors | At regular check-ups |
| Transvaginal Ultrasound | Measure endometrial thickness | When abnormal bleeding occurs |
| Endometrial Biopsy | Detect precancerous cells | If the endometrium is thickened or bleeding is abnormal |
These tools help identify potential issues early, allowing for timely decisions about further interventions like biopsies.
When You Need an Endometrial Biopsy
A transvaginal ultrasound is often the first step in determining whether a biopsy is necessary. If the endometrial thickness measures ≤4 mm, the likelihood of endometrial cancer is extremely low, with a negative predictive value greater than 99%.
However, a biopsy may be warranted if you experience abnormal uterine bleeding - especially if it’s heavy, lasts longer than 8 days, or occurs between periods. The Pipelle biopsy, a simple in-office procedure, has a 91% detection rate for endometrial abnormalities in premenopausal women. If hyperplasia is diagnosed and treated with progestins, follow-up biopsies are usually done every 3 months until two consecutive negative results confirm the condition has resolved.
"To effectively prevent the progression to endometrial malignancy, clinicians must remain vigilant regarding the signs and symptoms of endometrial hyperplasia, especially when treating patients with polycystic ovarian disease and obesity." – StatPearls
Ongoing follow-up, including remote consultations, ensures that these evaluations remain on track.
Using Telehealth for PCOS Management
Telehealth offers a convenient way to manage follow-up care and monitoring. Virtual consultations can help coordinate in-office procedures, such as biopsies, and allow for remote reviews of critical health markers. For example, services like Oana Health connect you with licensed medical professionals who can prescribe and monitor hormonal treatments (like oral contraceptives) and metabolic medications, such as oral Metformin ER ($22/month) or oral GLP-1 & Metformin ($199/month). Medications are shipped directly to your home with free delivery.
Telehealth also simplifies tracking warning signs and supports lifestyle changes, such as weight loss counseling and dietary guidance - both of which are essential for managing metabolic and reproductive risks. At-home testing kits for biomarkers like testosterone, insulin, and HgbA1c make it easier to stay on top of your health, with results reviewed during virtual appointments. This combination of remote and in-person care ensures a comprehensive approach to managing PCOS and its associated risks.
Conclusion
Managing hormonal and metabolic imbalances plays a crucial role in preventing endometrial hyperplasia in individuals with PCOS. The connection between PCOS and endometrial hyperplasia stems from unopposed estrogen - a condition where chronic anovulation causes the uterine lining to thicken without progesterone to trigger its shedding. This imbalance increases the risk of endometrial cancer threefold for women with PCOS compared to those without the condition. However, proper management can significantly lower this risk.
Hormonal contraceptives are often the first step in managing this condition, helping regulate menstrual cycles and ensuring regular endometrial shedding. Addressing metabolic factors is equally important. Medications like Metformin help reduce androgen levels and decrease estrogen stimulation. Lifestyle changes, including weight loss and improved habits, further mitigate metabolic risks.
"The hyperplastic changes often regress if physiological progesterone levels are resumed or therapeutic progestins are utilized." – StatPearls
Tracking menstrual cycles and promptly addressing abnormal bleeding are essential for early detection. Regular follow-up biopsies, typically every three months, confirm whether the condition is resolving.
Telehealth services, such as Oana Health, simplify long-term management by connecting patients with licensed medical professionals. These platforms can prescribe treatments like oral Metformin ER ($22/month) or oral GLP-1 & Metformin ($199/month), delivered directly to your door. Through remote consultations, patients receive support for symptom tracking, medication adjustments, and lifestyle counseling - all critical components in preventing the progression of endometrial changes.
FAQs
What is the connection between PCOS and endometrial hyperplasia?
Polycystic ovary syndrome (PCOS) is linked to a higher risk of endometrial hyperplasia, largely due to hormonal imbalances. Women with PCOS often experience chronic anovulation, meaning ovulation doesn’t happen regularly. This results in prolonged exposure to elevated estrogen levels without enough progesterone to balance it - a condition referred to as unopposed estrogen. Over time, this imbalance can cause the endometrial lining to thicken excessively, which raises the risk of developing hyperplasia.
Addressing PCOS through lifestyle adjustments, hormone therapy, or other medical treatments can help lower this risk. For tailored advice and treatment, it’s a good idea to consult a healthcare provider who specializes in PCOS and hormonal health.
What are the early signs of endometrial hyperplasia in women with PCOS?
Early signs of endometrial hyperplasia in women with PCOS often show up as noticeable changes in menstrual bleeding patterns, largely due to prolonged exposure to unopposed estrogen. Symptoms to watch for include heavy or prolonged periods, short menstrual cycles (fewer than 21 days), spotting between periods, or even bleeding after menopause. Some women may also experience pelvic discomfort, a sensation of pressure, or pass unusually large blood clots.
Because the hormonal imbalances tied to PCOS can mask or complicate these symptoms, it’s crucial to stay alert to any new or worsening heavy bleeding, unexpected spotting, or signs of unexplained anemia. If these symptoms sound familiar, Oana Health’s telehealth services can guide you through assessing your risk, arranging testing, and accessing personalized, prescription-based treatments - all without leaving your home.
How can lifestyle changes help reduce the risk of endometrial hyperplasia in women with PCOS?
Lifestyle adjustments that improve insulin sensitivity and reduce excess estrogen exposure can play a big role in lowering the risk of endometrial hyperplasia for women with PCOS. Since unopposed estrogen - often linked to excess body fat and irregular ovulation - is a major factor, even a small weight loss (about 5% of body weight) can help restore ovulation and decrease this risk.
Focusing on a balanced diet rich in whole foods, high in fiber, and low in refined carbs and dairy can aid in weight loss and help lower insulin levels. This, in turn, reduces ovarian androgen production and excess estrogen. Adding regular physical activity, such as aerobic exercises like brisk walking or cycling, along with resistance training, can further improve insulin sensitivity and support a healthy weight.
For those who need extra guidance, Oana Health provides personalized, science-backed telehealth programs designed to manage PCOS symptoms, balance hormones, and reduce the risk of endometrial hyperplasia - all without leaving home.
