Plant-Based Diets and Insulin Resistance
Yes, it can. Insulin resistance is a key driver of PCOS symptoms, affecting up to 70% of women with PCOS and even more in those who are overweight. A plant-based diet - rich in fiber, whole grains, legumes, fruits, and vegetables - can improve insulin sensitivity and help regulate hormonal imbalances. Here's why:
- Improves Insulin Sensitivity: High-fiber foods stabilize blood sugar and reduce fat buildup in cells, which enhances insulin signaling.
- Lowers Androgen Levels: Reduced insulin levels mean fewer male hormones like testosterone, easing symptoms like acne, hair growth, and irregular cycles.
- Supports Weight Management: Plant-based diets are naturally lower in saturated fats, aiding in weight loss and reducing inflammation.
- Reduces Diabetes Risk: Women with PCOS are 4-9 times more likely to develop Type 2 diabetes, but plant-based diets can lower this risk by up to 78%.
Key Research Findings:
- A 16-week vegan diet study showed significant drops in insulin resistance (HOMA-IR index: -1.0) and visceral fat (224 cm³ reduction).
- Replacing just 5% of animal protein with plant protein can reduce diabetes risk by 23%.
Meal Tips:
- Focus on ½ vegetables, ¼ whole grains, ¼ plant protein, and healthy fats like nuts or olive oil.
- Include low-glycemic carbs (quinoa, lentils) and plant-based proteins (tofu, beans).
For severe symptoms, combining this diet with medications like metformin or GLP-1 agonists can yield faster results, improving insulin sensitivity by up to 50% and reducing symptoms within weeks.
PCOS management is more effective with a tailored approach, blending diet, medical treatment, and monitoring for long-term improvements.
How Plant-Based Diets Improve Insulin Sensitivity
What Is a Plant-Based Diet?
A plant-based diet focuses on making vegetables, fruits, legumes, whole grains, nuts, and seeds the centerpiece of your meals. It doesn’t necessarily mean cutting out all animal products - though some individuals choose to - but rather prioritizing plant foods. Studies reveal that healthful plant-based diets (hPDI), which emphasize whole grains and legumes, can significantly boost insulin sensitivity. On the other hand, unhealthful plant-based diets (uPDI) loaded with refined grains and added sugars fail to provide these benefits. Let’s dive into how these dietary habits work at the cellular level to improve insulin sensitivity.
How Plant-Based Diets Work
Plant-based diets enhance insulin sensitivity through a combination of biological processes. For starters, their high fiber content slows down glucose absorption, helping to prevent sudden spikes in blood sugar. Additionally, swapping saturated fats - like palmitic acid found in animal products - with healthier fats, such as monounsaturated and polyunsaturated fats from nuts, seeds, and vegetable oils, supports better insulin signaling.
"Saturated fatty acids and palmitic acid, in particular, interfere with insulin signalling in muscle cells due to the accumulation of free fatty acid intermediates, ceramides and diacylglycerol."
- Michalina Banaszak, Faculty of Medical Sciences, Poznan University of Medical Sciences
These diets also work to reduce fat accumulation in muscle and liver cells, which is a key factor in insulin resistance. When excess fat within these cells decreases, their response to insulin signals improves. Moreover, the antioxidants and phytonutrients found in plant-based foods help combat inflammation and oxidative stress - two contributors to insulin resistance. Together, these cellular-level improvements are backed by strong clinical research, as outlined below.
What Research Shows About Plant-Based Diets
The scientific evidence in favor of plant-based diets for improving insulin sensitivity is compelling. For example, a meta-analysis found that these diets reduced fasting insulin levels by –4.13 µU/mL in individuals with overweight or obesity. Similarly, the Adventist Health Study 2 revealed that vegans had a 49% lower risk of developing Type 2 diabetes compared to non-vegetarians.
In a 16-week study conducted in Washington, DC, involving 75 overweight adults, participants following a low-fat vegan diet - consisting of approximately 75% carbohydrates, 15% protein, and 10% fat - experienced significant improvements in beta-cell glucose sensitivity and a reduction in visceral fat volume by 224 cm³.
Even small changes can make a big difference. Replacing just 5% of energy intake from animal protein with plant-based protein is linked to a 23% reduced risk of Type 2 diabetes. For women with PCOS, these benefits extend beyond blood sugar control, as improved insulin sensitivity leads to lower androgen levels, helping to restore hormonal balance.
Building a PCOS-Friendly Plant-Based Meal
The Basic Plate Structure
Creating meals with a plant-based focus can help improve insulin sensitivity and support hormonal balance, which is especially important for managing PCOS. A simple way to structure your plate is to divide it into sections: ½ non-starchy vegetables, ¼ whole grains or starchy vegetables, ¼ plant protein, and 1–2 thumb-sized portions of healthy fats. For an easy visual guide, think: 2 fists of vegetables, 1 cupped hand of grains or starchy vegetables, 1 palm of protein, and 1–2 thumbs of fat per meal.
Here’s how this might look in real life:
- Breakfast: Sautéed spinach, tomatoes, and mushrooms with steel-cut oats, a tofu scramble seasoned with nutritional yeast, and a topping of ground flaxseed and olive oil.
- Lunch: A hearty salad with mixed greens, colorful vegetables, cooked quinoa, baked tempeh or black beans, avocado, and a vinaigrette made from extra-virgin olive oil.
- Dinner: Stir-fried non-starchy vegetables with brown rice or buckwheat, marinated tofu or edamame, cooked in avocado or olive oil, and finished with sesame seeds.
Balancing Macronutrients for PCOS
Plant-based diets naturally include more carbohydrates, as many plant proteins - like beans and lentils - contain carbs. For PCOS, the focus should be on low to moderate glycemic index (GI) carbs, such as intact whole grains (steel-cut oats, quinoa, brown rice), beans, lentils, and starchy vegetables with their skin, like sweet potatoes. It’s best to limit refined and high-GI carbs, such as white bread, sugary cereals, pastries, and ultra-processed snacks, as these can worsen insulin resistance. To keep blood sugar stable, fill about ¼ of your plate with carbs and pair them with protein, fiber, and healthy fats.
For protein, aim for 20–30 grams per meal, which typically means 1.2–1.6 grams of protein per kilogram of body weight daily. Examples include ¾–1 cup of cooked lentils or beans (12–18 grams of protein), ½ cup of quinoa (4 grams), or 3–4 ounces of tofu or tempeh (15–20 grams). When it comes to healthy fats, include 1–2 servings per meal - this could be 1–2 tablespoons of oil, ¼ avocado, or a small handful of nuts or seeds. Focus on monounsaturated fats (from olive oil, avocado, or nuts) and plant-based omega-3 sources like ground flaxseed, chia seeds, walnuts, and hemp seeds. These fats can help address the omega-3 gap that arises when fish is excluded.
While balancing macronutrients is key, it’s also important to pay attention to specific micronutrients that are often less abundant in plant-based diets.
Nutrients to Watch on a Plant-Based Diet
Certain nutrients require extra attention when following a plant-based diet:
- Vitamin B12: Since it’s not naturally present in plant foods, include fortified options like plant milks, breakfast cereals, or consider a B12 supplement.
- Iron: Plant-based iron (non-heme iron) is found in lentils, beans, tofu, pumpkin seeds, and fortified cereals. Pair these with vitamin C-rich foods, such as bell peppers or citrus, to improve absorption.
- Zinc: Sources include beans, lentils, chickpeas, nuts, seeds, and whole grains. Soaking or sprouting these can help with absorption.
- Omega-3s (ALA): Found in ground flaxseed, chia seeds, walnuts, and hemp seeds. For additional support, some may benefit from an algae-based DHA/EPA supplement.
- Vitamin D: This nutrient is often low in many people, not just those with PCOS. It’s linked to insulin resistance and other PCOS symptoms. Include fortified plant milks and cereals, and consult with a clinician about supplementation.
For women dealing with persistent symptoms like severe insulin resistance, irregular cycles, or other PCOS-related issues, professional guidance can make a big difference. Oana Health, for example, offers a tailored approach that combines nutrition advice with prescription-based treatments. They provide personalized plans, including carbohydrate targets, supplementation (like vitamin D, B12, and omega-3s), and medication adjustments. This combination of plant-based eating and targeted treatments often leads to better symptom management than dietary changes alone.
How Diet Affects PCOS
sbb-itb-6dba428
Combining Plant-Based Eating with Medical Treatment
Plant-Based Diet vs Diet Plus Medical Treatment for PCOS Management
How Diet and Medications Work Together
Plant-based diets can significantly improve insulin sensitivity, but when combined with targeted medications, the results can be even more impactful. The high fiber and low-glycemic-index foods in plant-based diets help slow carbohydrate absorption and stabilize blood sugar levels. On the medication side, options like metformin work by reducing glucose production in the liver and improving how cells respond to insulin. Similarly, GLP-1 agonists, such as semaglutide, slow digestion and encourage insulin release after meals. For women dealing with high androgen levels, spironolactone helps by blocking androgen receptors, which can reduce symptoms like acne and unwanted hair growth. Antioxidants from fruits and vegetables further support hormonal balance, adding another layer of benefit.
Research shows that combining a whole-food, plant-based diet with medications can lead to significant changes. For example, this pairing can reduce the need for medications by up to 43% and dramatically lower insulin resistance in just a few weeks. The reason this works so well is that medications target specific metabolic or hormonal pathways, while plant-based diets enhance these effects by improving weight management, reducing inflammation, and promoting gut health. Studies have even found that replacing animal protein with plant protein - making up about 35% of total protein intake - can lower HbA1c, fasting glucose, and fasting insulin levels. Many patients start noticing improvements in their symptoms within three to four weeks [6]. This combination of diet and medication creates a strong foundation for personalized treatment plans.
Oana Health: Personalized PCOS Treatment
Oana Health takes dietary improvements a step further by integrating customized medication plans to address insulin resistance and hormonal imbalances. Their telehealth services combine science-backed prescriptions with tailored lifestyle strategies. Licensed professionals create medication plans to target individual symptoms, such as insulin resistance, hormonal acne, unwanted hair growth, or weight management. Medications are delivered directly to your door with free shipping, making the process convenient and accessible. Options include oral or topical metformin and GLP-1 tablets, among others.
One standout feature of Oana Health's approach is the availability of topical metformin. This option offers the benefits of improved insulin sensitivity without the gastrointestinal side effects - like nausea - that often come with oral metformin. As one patient, Carrie S., shared:
"I used to struggle a lot with the side effects for oral metformin and this is a great alternative for me. I get the same benefits but no more upset stomach and nausea, and this helps me stick with it a lot more consistently." - Carrie S.
Oana Health also provides supplementation recommendations to address potential nutrient gaps that can arise with a plant-based diet. Clinical studies reveal that 81% of women using targeted PCOS treatments report significant improvements within one year [6]. Victoria A., another patient, shared her experience:
"Oana's telehealth service is fantastic! It's helped manage my insulin levels and reduce excess hair growth I was experiencing due to PCOS." - Victoria A.
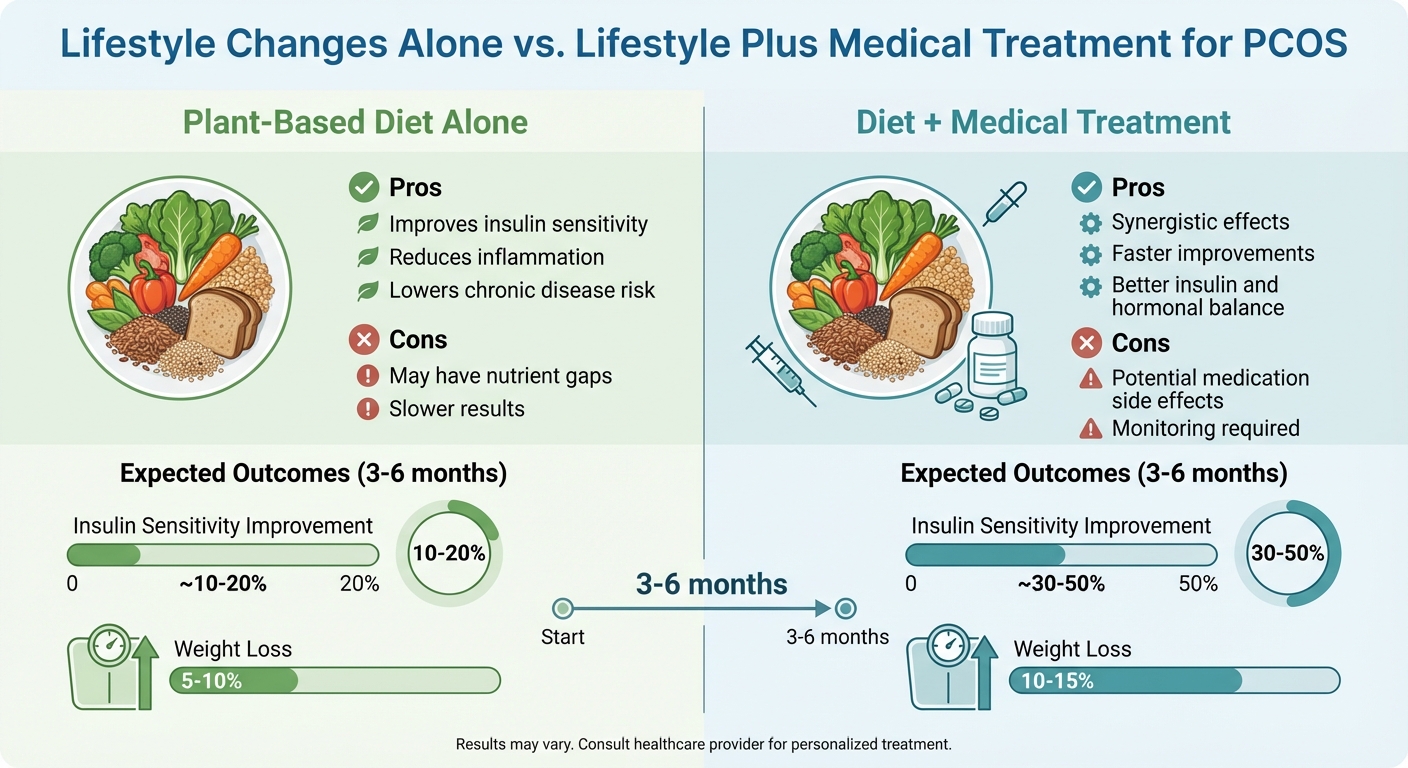
Lifestyle Changes Alone vs. Lifestyle Plus Medical Treatment
Deciding between focusing solely on diet or combining it with medical treatment depends on how severe the symptoms are and how quickly results are needed. A plant-based diet alone can improve insulin sensitivity by about 10–20% and lead to modest weight loss (5–10%) over three to six months. However, for those with more severe insulin resistance or obesity, adding medications can boost insulin sensitivity by 30–50% and support greater weight loss (10–15%) in the same period.
Here's a comparison of the two approaches:
| Approach | Pros | Cons | Expected Outcomes (3–6 months) |
|---|---|---|---|
| Plant-Based Diet Alone | Improves insulin sensitivity; reduces inflammation and chronic disease risk | May have nutrient gaps and slower results | ~10–20% improvement in insulin sensitivity with 5–10% weight loss |
| Diet + Medical Treatment | Synergistic effects leading to faster improvements in insulin and hormonal balance | Potential medication side effects; monitoring required | ~30–50% improvement in insulin sensitivity, 10–15% weight loss |
For women with severe symptoms or persistent insulin resistance, the combined approach often delivers better results. Medications typically take three to four weeks to build up in the body, and noticeable improvements follow shortly after [6]. As Allison L. explained:
"It's been a little over 5 weeks, and I've noticed a dramatic reduction in my facial hair growth... You really have to stick with it and be patient to notice results!" - Allison L.
If you're unsure how to start, consider consulting a healthcare provider. Platforms like Oana Health's telehealth service can help you explore the best combination of dietary changes and medical treatments tailored to your specific needs.
Conclusion: Managing PCOS Through Diet and Medical Care
Shifting to a whole-food, plant-based diet can play a powerful role in managing PCOS symptoms. By stabilizing blood sugar, reducing inflammation, and supporting weight management, this approach improves insulin sensitivity and helps women experience better energy levels, more regular cycles, and improved blood sugar control. However, it’s important to remember that diet is just one piece of the puzzle.
PCOS is influenced by factors like genetics, insulin resistance, and inflammation. Combining a thoughtful diet with medications such as metformin or hormonal therapies often leads to better outcomes. This combination can improve metabolic health, regulate menstrual cycles, and enhance reproductive results. While a plant-based diet offers many benefits, it may not address all hormonal imbalances or symptoms on its own.
It’s essential to manage expectations and track progress. Monitoring cycles, energy levels, and symptoms over time can help you and your healthcare provider make informed adjustments to your plan. Keeping a detailed record of these changes allows for a more personalized approach to both diet and medical treatments.
For those looking to expand their care options, telehealth services provide convenient, customized solutions. For example, Oana Health offers evidence-based treatments delivered directly to your door with free shipping. By integrating plant-based nutrition with professional medical guidance, you can create a well-rounded plan to tackle PCOS. Start small - introduce more plant-based meals into your routine - and consult with a healthcare provider to review your symptoms and lab results for long-term improvements in insulin sensitivity and hormonal balance.
FAQs
How can a plant-based diet help improve insulin resistance in PCOS?
A plant-based diet can play a significant role in improving insulin resistance in individuals with PCOS by providing essential nutrients that promote better blood sugar management. For example, foods high in fiber help slow the absorption of glucose, which can prevent sudden spikes in blood sugar levels. Additionally, plant-based diets tend to be lower in saturated fats, which are known to contribute to insulin resistance.
Plant-based foods are also loaded with antioxidants and phytochemicals that help combat inflammation and oxidative stress - both of which can exacerbate insulin resistance. Over time, these dietary adjustments may enhance insulin sensitivity, support hormonal balance, and reduce visceral fat, all of which are key for managing PCOS effectively.
What nutrients might be missing in a plant-based diet for PCOS, and how can you make up for them?
A plant-based diet can help improve insulin sensitivity by cutting down on saturated fats and increasing fiber intake. However, women with PCOS might find it challenging to get enough of certain nutrients, such as vitamin B12, iron, calcium, vitamin D, zinc, and omega-3 fatty acids. These nutrients play a crucial role in hormone balance and managing insulin resistance, but they’re often harder to source from plants alone.
To fill these nutritional gaps, consider incorporating fortified foods and supplements into your diet. For vitamin B12, look for options like B12-fortified plant-based milks, cereals, or nutritional yeast, and think about adding a daily B12 supplement. To boost calcium, try fortified almond or soy milk, calcium-set tofu, or leafy greens like kale. Vitamin D can be obtained through safe sun exposure or by taking a 1,000–2,000 IU D3 supplement. For iron and zinc, include foods like legumes, pumpkin seeds, and tempeh in your meals, and pair them with vitamin C-rich foods (like citrus fruits) to enhance absorption. As for omega-3 fatty acids, ground flaxseed, chia seeds, walnuts, and algae-based EPA/DHA supplements are great plant-based sources.
If you’re looking for more personalized help, Oana Health provides tailored telehealth solutions designed to meet your specific needs. They can create a custom supplement plan to support your hormonal health and improve insulin sensitivity, with treatments conveniently delivered right to your door.
How can a plant-based diet combined with medical treatments help manage PCOS?
Polycystic ovary syndrome (PCOS) is often tied to insulin resistance, which can trigger symptoms like irregular periods, weight gain, and elevated androgen levels. Addressing insulin resistance plays a crucial role in managing these symptoms and improving hormonal balance.
Adopting a plant-based diet can be a powerful way to boost insulin sensitivity. Foods rich in fiber - such as fruits, vegetables, legumes, and whole grains - help stabilize blood sugar levels. Plus, plant-based diets tend to include less saturated fat and more antioxidants, which can lower inflammation and oxidative stress, both of which are linked to insulin resistance.
Combining dietary changes with medical treatments like metformin, hormonal therapies, or anti-androgen medications can amplify results. This approach may improve insulin function, regulate menstrual cycles, aid in weight control, and ease symptoms like acne or excess hair growth. Oana Health offers tailored, prescription-based PCOS treatments along with nutrition support, making it simpler to integrate these strategies into your daily life.
