Ultimate Guide to Hormonal Drug Packaging Safety
Hormonal drug packaging plays a critical role in ensuring patient safety and medication effectiveness. Poor packaging can lead to dosing errors, drug degradation, and serious health risks. Here’s what you need to know:
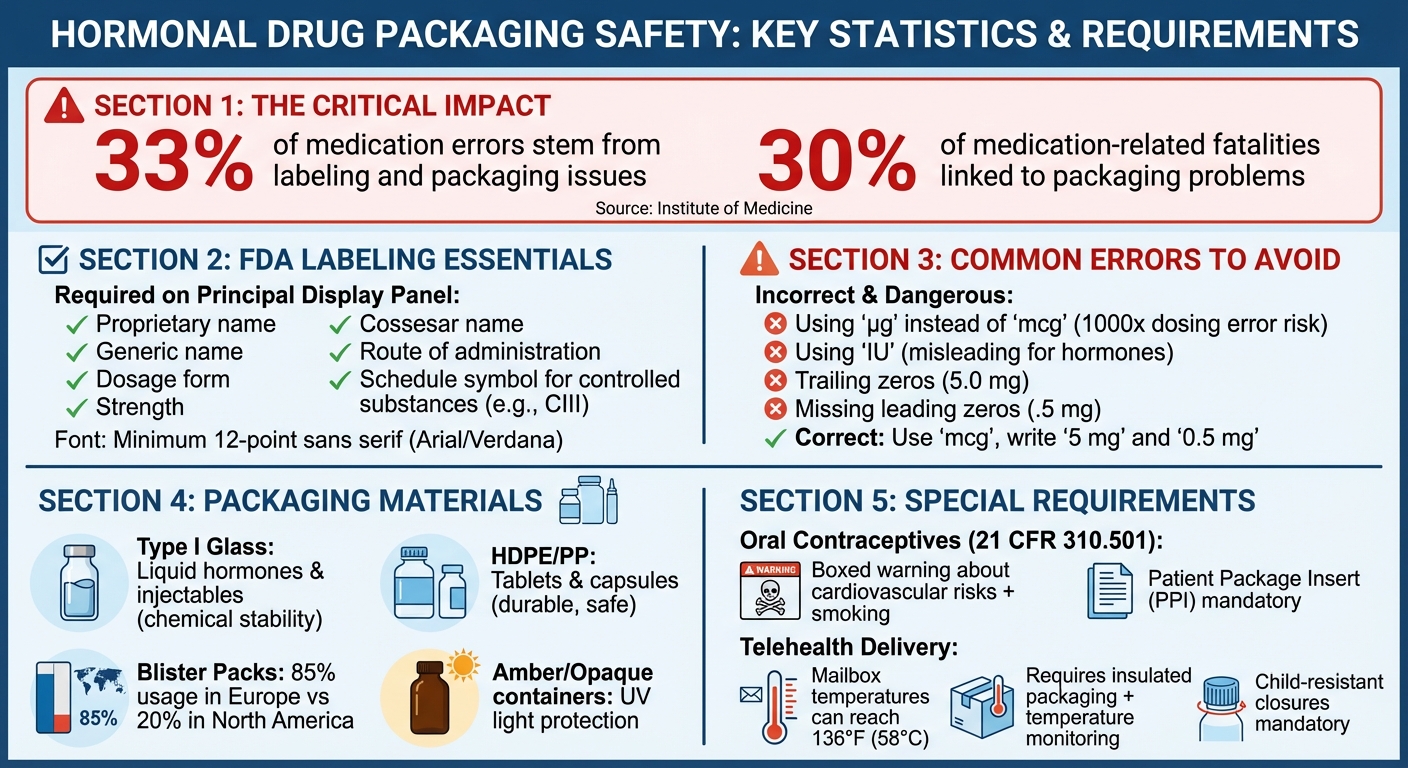
- Key Risks: Packaging issues contribute to 33% of medication errors and 30% of fatalities.
- FDA Requirements: Labels must include clear drug names, strengths, and instructions. For example, oral contraceptives require boxed warnings about cardiovascular risks.
- Packaging Materials: Blister packs, Type I glass, and HDPE are commonly used to protect against light, moisture, and contamination.
- Telehealth Considerations: Medications shipped to patients must be protected from extreme temperatures and include clear, user-friendly labeling.
- Common Errors: Misleading abbreviations like "µg" instead of "mcg" and unclear labeling increase the risk of mistakes.
Safe packaging ensures hormonal medications are effective and easy to use while minimizing health risks. Whether dispensed in person or through telehealth, strict adherence to FDA guidelines is non-negotiable.
Hormonal Drug Packaging Safety Statistics and FDA Requirements
FDA Regulations for Hormonal Drug Packaging
The FDA has established specific rules for the packaging and labeling of hormonal medications. These regulations are designed to ensure that patients receive their medications safely, with all necessary details clearly presented.
FDA Labeling and Packaging Requirements
Hormonal drug packaging must include critical information on the Principal Display Panel (PDP) - the side most visible to the user. This includes the proprietary name, generic name, dosage form, strength, and administration route. For controlled substances like testosterone, the label must also prominently display the schedule symbol (e.g., CIII).
To enhance readability, manufacturers are required to use a sans-serif font (such as Arial or Verdana) in a minimum 12-point size, with all text uniformly oriented. For medications with complex administration methods, like hormonal injections or patches, manufacturers must provide clear Instructions for Use (IFU). These instructions should be written at or below the average national reading level, using straightforward, active language like "Wash your hands".
Oral contraceptives come with additional requirements under 21 CFR 310.501. Each package must include a Patient Package Insert (PPI) that contains a boxed warning about the increased risk of serious cardiovascular side effects associated with cigarette smoking. Without this insert, oral contraceptives are considered misbranded by the FDA. Hospitals and long-term care facilities must ensure that patients receive this insert before their first dose.
For blister packs, which are commonly used for hormonal medications, each individual dose cell must display the product name, strength, lot number, and expiration date. The packaging material must maintain text legibility even after doses are removed. Additionally, "mcg" should be used instead of "μg" to minimize the risk of dosing errors.
In addition to these labeling standards, manufacturers must incorporate safety features to prevent tampering and ensure child protection.
Child-Resistant and Tamper-Evident Packaging Requirements
Hormonal medications classified as controlled substances are required to have tamper-evident seals that clearly indicate if the product has been opened or tampered with. This is mandated under 21 CFR 1302.06 for products like anabolic steroids, ensuring that medications remain secure throughout distribution.
Child-resistant packaging is regulated under the Poison Prevention Packaging Act, while the FDA oversees how these features are communicated on labels. Manufacturers are encouraged to include clear statements about child-resistant packaging to help pharmacists and patients identify safe containers. For transparent containers, such as ampules or syringes, embossed or debossed text should be avoided. Instead, an overwrap with a printed label is recommended for better visibility.
To further enhance security, the Drug Supply Chain Security Act (DSCSA) requires manufacturers to include a 2D data matrix barcode on each package. This barcode encodes essential details like the National Drug Code (NDC), lot number, and expiration date. These measures are crucial for preventing counterfeiting and ensuring the authenticity of hormonal medications, directly safeguarding patient safety and treatment outcomes.
Packaging Materials for Hormonal Medications
Choosing Safe and Durable Packaging Materials
When it comes to hormonal medications, selecting the right packaging is all about balancing protection, safety, and performance. The materials used must shield the medication from environmental factors while ensuring that no harmful substances leach into the product.
For liquid hormonal medications and injectables, Type I glass is the go-to choice. Its chemical stability and ability to block gas and moisture make it ideal for preserving the medication's integrity. On the other hand, solid oral doses like tablets and capsules often rely on High-Density Polyethylene (HDPE) and Polypropylene (PP) for bottles and caps. These materials are not only durable but also meet safety standards under Food Additive Regulations.
Blister packs are particularly popular for hormonal contraceptives, especially in Europe. Here, about 85% of solid unit doses use blister packaging, compared to just 20% in North America. These packs combine thermoformed plastics like PVC with aluminum foil or paperboard lidding. This design not only protects against humidity and contamination but also helps patients follow proper dosing schedules.
Light sensitivity is another critical factor for hormonal medications. To prevent ultraviolet light from degrading the drug, manufacturers use amber or orange-colored glass and opaque plastics. For moisture-sensitive medications, adding desiccant packets can help, though care must be taken to avoid absorbent materials that could attract excess moisture.
A key concept in packaging is the functional barrier. Materials like metal foil or specialized polymers are used to block external contaminants - such as printing inks and adhesives - from migrating into the medication. For instance, the FDA requires that residual vinyl chloride monomer in PVC films for blister packs remain below 5 parts per billion. Packaging must also endure extreme transit conditions, ensuring that the medication reaches patients intact, even when distributed through telehealth services.
Environmental Impact and Sustainable Options
As sustainability becomes a growing concern, the pharmaceutical industry is under pressure to adopt eco-friendly packaging without compromising safety. The FDA's framework for recycled plastics provides a pathway for manufacturers to explore greener alternatives while ensuring patient safety.
The functional barrier concept plays a significant role in sustainability efforts. For example, if a barrier layer like metal foil effectively prevents material migration, outer layers can incorporate recycled materials without affecting drug safety. However, any sustainable packaging must still meet strict criteria: it must protect against light, moisture, and gases; remain compatible with the drug; avoid toxic extractables; and perform effectively in delivering the medication.
"A drug is deemed to be adulterated 'if its container is composed, in whole or in part, of any poisonous or deleterious substance which may render the contents injurious to health...." - Federal Food, Drug, and Cosmetic Act
To comply with safety and environmental standards, manufacturers must adhere to regulations like 21 CFR 174-186 and USP <661> and <660>. For high-risk routes of administration, toxicological evaluations are essential. These sustainable advancements are not just about reducing environmental impact - they're about maintaining the highest safety and compliance standards for hormonal medication packaging.
Packaging Requirements for Female Hormonal Health Products
Labeling Requirements for Estrogen and Progestin Therapies
Female hormonal health products are subject to some of the strictest packaging rules in the pharmaceutical world. For instance, Patient Package Inserts (PPIs) are mandatory for all prescription estrogen drugs under FDA regulation 21 CFR 310.515. Interestingly, PPIs are specifically required for only two drug categories: oral contraceptives and estrogen-containing products.
Every patient package must include a PPI with eight key details: the drug name, manufacturer information, benefits, proper uses, contraindications, serious risks, side effects, risk-reduction instructions, and the revision date. For bulk packages or multi-dose vials, there must be enough PPIs included for every patient. If the patient is in a hospital or long-term care facility, they must receive the PPI before their first dose and every 30 days thereafter during treatment.
The Principal Display Panel (PDP) also has its own requirements. It must clearly show the proprietary name, established name, dosage form, product strength, and route of administration. These details must remain easily visible. For estradiol products, the labeling must use the term "Estradiol" (current terminology) instead of the outdated "Alpha Estradiol." Additionally, potency must be listed by weight (mg or mcg) rather than international units, as the FDA considers IU declarations misleading for estrogenic hormones.
"The safe and effective use of drug products containing estrogens requires that patients be fully informed of the benefits and risks involved in the use of these drugs." - 21 CFR § 310.515
These labeling rules align with broader FDA packaging standards and are critical for ensuring safety. Non-compliance results in the product being labeled as misbranded under the Federal Food, Drug, and Cosmetic Act. This is especially important considering that labeling and packaging issues account for 33% of medication errors and 30% of related fatalities.
These stringent protocols also pave the way for additional safety measures like boxed warnings.
Black Box Warnings and Patient Safety Information
Beyond detailed labeling, boxed warnings represent the FDA's highest level of risk notification. These boxed warnings are mandatory for certain hormonal therapies to emphasize serious health risks. For example, combined hormonal contraceptives (CHCs), which are commonly prescribed for conditions like PCOS, must include a boxed warning about cigarette smoking and the risk of severe cardiovascular events. This warning must be visible on the packaging and prominently featured in the prescribing information.
For perspective, women using combined oral contraceptives face a risk of venous thromboembolism (VTE) ranging from 3 to 9 cases per 10,000 woman-years. Non-oral CHCs, such as patches or rings, carry a slightly higher risk, with 3 to 12 cases per 10,000 woman-years. With over 400 medications currently requiring FDA-assigned boxed warnings, these alerts are crucial for protecting patients.
To make sure these warnings are noticed, the FDA advises using a minimum 12-point sans serif font for critical safety information. They also recommend maintaining high color contrast and avoiding clutter or distracting graphics. Safety-related headings in patient instructions should be bolded and written in action-oriented language to minimize the risk of injury or reduced efficacy. These warnings should appear on the PDP - the section most likely to catch the user’s eye - with ample blank space around them to enhance visibility.
For hormonal medications classified as controlled substances, additional labeling rules apply. The label must clearly display the schedule symbol (like CIII) in a size large enough to be easily identified on a pharmacy shelf. Each commercial container must also feature a tamper-evident seal. Together, these layered safety measures ensure that patients receiving hormonal therapies - whether through traditional pharmacies or telehealth providers like Oana Health - are adequately protected.
sbb-itb-6dba428
Maintaining Compliance and Preventing Packaging Errors
Common Packaging Errors and Associated Risks
Packaging errors are not only frequent but also potentially dangerous, especially when it comes to medications. For hormonal drugs, such mistakes can have serious consequences, increasing the risk of medication errors.
Some common issues include missing or poorly displayed information on the Principal Display Panel (PDP). If critical details - like the product name, dosage form, or strength - are unclear or require users to rotate the container to find them, the likelihood of errors increases. Oversized logos, decorative graphics, and unnecessary design elements can also distract from essential information. Another major concern is look-alike packaging, where similar color schemes or identical branding across different strengths can lead to selection mistakes.
Legibility is another significant factor. Text that's too small, uses thin or condensed fonts, or lacks sufficient color contrast can make it harder to read. For example, the abbreviation "µg" for micrograms is often misinterpreted as "mg", potentially resulting in a thousand-fold dosing error. Injectable hormonal medications in clear containers present their own challenges - overlapping text printed on opposite sides can become unreadable. Similarly, blister packs without clear labeling on individual cells can lead to confusion about the product name and strength.
"Poor label or labeling design can contribute to medication errors by making it difficult for end users to readily locate and understand critical safety information." - FDA Guidance for Industry
To address these risks, a systematic checklist approach is critical for ensuring compliance and avoiding packaging errors, whether for traditional distribution or telehealth delivery of hormonal medications.
Compliance Checklist for Hormonal Drug Packaging
Preventing packaging errors requires a methodical approach. Start by ensuring that the PDP includes all essential details, such as the proprietary name, established name, dosage form, product strength, route of administration, and any necessary warnings. For combined hormonal contraceptives, make sure the boxed warning about cigarette smoking and cardiovascular risks is prominently displayed.
Replace abbreviations like "µg" with "mcg" to avoid misinterpretation, and avoid using "IU", which can also lead to dosing confusion. Always eliminate trailing zeros (e.g., write "5 mg" instead of "5.0 mg") and include leading zeros for decimals (e.g., "0.5 mg" instead of ".5 mg"). Use at least a 12-point sans serif font, such as Arial, with high contrast between the text and background. Arrange all critical information within the same field of vision to eliminate the need for container rotation. For products with multiple strengths, use bold text, boxes, or distinct colors to clearly differentiate them.
Don’t forget the technical details. The National Drug Code (NDC), lot number, and expiration date should be displayed in both human-readable and machine-readable formats, including the 2D data matrix barcode required by the Drug Supply Chain Security Act. For injectable hormonal products, ensure that enough of the container remains transparent so users can properly inspect the contents.
"Product naming, labeling, and packaging should be designed for the end user - the provider in the clinical environment and/or the consumer." - Institute of Medicine
Safe Packaging for Telehealth Delivery
Packaging Standards for Telehealth-Prescribed Hormonal Medications
When hormonal medications like Spironolactone are delivered through telehealth services, the packaging must adhere to the same stringent FDA standards as traditional pharmacy dispensing. However, additional considerations are necessary for shipping and home delivery. These standards, previously detailed in discussions about Prescription Drug Packaging (PDP) requirements, remain consistent to ensure a seamless transition from traditional dispensing to telehealth.
A 1995 FDA study revealed that mailbox temperatures can soar to 136°F (58°C), far exceeding typical ambient conditions. This highlights the importance of using insulated packaging and temperature monitoring for shipping heat-sensitive medications. To address these challenges, telehealth providers often rely on insulated packaging with gel packs or temperature monitors to maintain the stability of hormonal medications during transit.
Child-resistant closures are another critical requirement to prevent accidental ingestion by children. Additionally, moisture-sensitive medications must include desiccants, while light-sensitive drugs require amber or opaque containers. Packaging must also comply with DSCSA-mandated markings, as outlined in earlier sections.
Telehealth companies like Oana Health ensure that medications delivered to patients' homes meet these rigorous standards while maintaining convenience. Each shipment includes essential documentation, such as patient package inserts written in clear, easy-to-understand language. Furthermore, FDA-regulated pharmacies involved in telehealth delivery utilize unit-of-use packaging, where an entire course of therapy is sealed in a single container.
Case Study: Hormonal Drug Packaging in Telehealth
The Institute of Medicine has reported that 33% of medication errors and 30% of related fatalities stem from labeling and packaging issues. To mitigate these risks, telehealth services often use unit-dose packaging for convenience and safety. Each unit-dose container must display key details, including the medication's established name, active ingredient quantity, expiration date, lot number, and manufacturer information.
Clear labeling is especially important for telehealth patients who may not have immediate access to a pharmacist. Labels must use a minimum 12-point sans serif font, such as Arial, with high contrast for better readability. When medications are repackaged for telehealth delivery, the expiration date is generally limited to six months or 25% of the remaining time on the original manufacturer’s bulk container - whichever is shorter. For drugs available in multiple strengths, color differentiation is helpful to reduce selection errors, but it should not be the sole method of identification. Proper packaging ensures the medication's potency is preserved by protecting it from moisture, light, and reactive gases like oxygen, which can degrade active ingredients during shipping and storage.
"The advantages of unit dose dispensing are that the drug is fully identifiable and the integrity of the dosage form is protected until the actual moment of administration." - FDA Compliance Policy Guide
For injectable hormonal medications or those stored in clear containers, telehealth providers add individual overwraps with clear, legible labels. These overwraps safeguard the product until use while leaving enough space for patients to inspect the medication for discoloration or precipitates.
Conclusion
Hormonal drug packaging plays a vital role in ensuring patient safety, from the moment a product is manufactured to when it’s used. With labeling and packaging issues accounting for 33% of medication errors and 30% of related fatalities, the design of pharmaceutical packaging is far more than a technicality - it’s a critical safeguard.
These principles remain consistent whether medications are dispensed at a local pharmacy or shipped through telehealth services. Key packaging features include clearly labeled drug names, strengths, and dosage forms, mandatory safety warnings like boxed warnings for combined hormonal contraceptives, child-resistant closures, tamper-evident seals, and error-reducing practices such as replacing "μg" with "mcg" for clarity.
"Product naming, labeling, and packaging should be designed for the end user - the provider in the clinical environment and/or the consumer." – Institute of Medicine
Whether medications are delivered through traditional pharmacies or telehealth providers like Oana Health, strict adherence to these packaging standards is essential. Packaging materials must shield hormonal drugs from moisture, light, and extreme temperatures - especially since mailbox temperatures can soar to 136°F (58°C) under direct sunlight. Each package must strike a balance between protection, safety, and usability to ensure patients receive effective treatment without added risks. By upholding these standards, every stakeholder contributes to safeguarding patient health and well-being.
FAQs
What are the most common packaging errors for hormonal drugs, and how can they be avoided?
The most common packaging mistakes for hormonal drugs often come down to unclear or poorly thought-out labels and containers. Problems like look-alike containers, tiny or hard-to-read fonts, and missing key details - such as dosage instructions, warnings, or expiration dates - can easily lead to errors. Other frequent issues include weak tamper-evident seals, incorrect or mismatched barcodes, and packaging that doesn’t adequately prevent leaks or contamination.
To tackle these issues, manufacturers should focus on creating user-friendly designs and performing rigorous testing. Some effective strategies include using bold, high-contrast fonts and distinct colors for drug names and strengths, placing critical safety information where it’s easy to see, and ensuring strong, reliable tamper-evident seals. Unique packaging shapes or sizes can also make hormonal medications stand out, reducing the risk of mix-ups. Companies like Oana Health implement these practices to ensure their prescription hormonal treatments are safe, clearly labeled, and compliant with FDA packaging safety standards.
How does telehealth delivery influence the packaging of hormonal medications?
Telehealth providers like Oana Health ship hormonal medications straight to patients’ homes, making secure and protective packaging a top priority. Unlike medications stored in traditional pharmacies, these shipments face potential risks like physical damage, exposure to moisture, and temperature fluctuations during transit. To address these challenges, packaging must include tamper-evident seals, offering patients peace of mind about the safety of their medications.
The FDA has strict requirements for packaging materials and labeling. The primary container must be durable and made from high-quality materials to ensure the medication’s integrity. Outer packaging must display FDA-compliant labeling, clearly listing the drug name, dosage, storage instructions, and expiration date. For oral medications, unit-dose packaging may also be necessary, making it easier to identify and manage individual doses. These precautions ensure the medication remains safe and effective from the moment it’s shipped to the moment it’s used.
What materials are best for ensuring hormonal medications stay safe from environmental factors?
To keep hormonal medications safe from light, moisture, air, and temperature fluctuations, using amber glass vials, pharmacopeial-grade plastics like HDPE or PET, metal containers or foils, and inert rubber or elastomeric closures is strongly advised. These materials act as a barrier, protecting the medication's quality and potency from environmental damage. Storing them correctly is crucial to preserving their safety and effectiveness.
